Professional Documents
Culture Documents
Staphylococci: Streptococcus Pyogenes
Uploaded by
Pharmacy2015Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Staphylococci: Streptococcus Pyogenes
Uploaded by
Pharmacy2015Copyright:
Available Formats
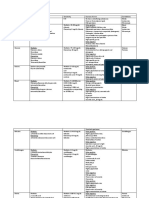
Staphylococci Physiology/Structure Pathogenesis/Immu nity Epidemiology Gram positive cocci Thick peptidoglycan with lipoteichoic acid, ribitol teichoic
acid with polysaccharide A residues Catalase positive, coagulase positive, protein A Commonly found as part of vaginal flora Virulence factors adherence to host tissue avoiding phagocytosis, toxins, hydrolytic enzymes Usually found in blood, vagina, nose and synovial fluid Normal flora on skin and mucosa Organisms can survive on dry surfaces Person-person spreading Risk factors foreign body presence, surgery, antibiotics that suppress normal flora Infants at risk for scalded skin syndrome Young children at risk for impetigo and skin infections Menstruating women can get TSS Patients with catheter, IV and shunts Patients with compromised respiratory function Toxic Shock Syndrome fatal infection with cutaneous and soft tissue involvement, multi-organ toxicity and protracted recovery period Toxin-mediated 1) food poisoning 2) TSS 3) Scaled skin syndrome Pyogenic 1) Impetigo (bullous, pustular) 2) folliculitis 3) furuncle 4) carbuncle (S. aureus) 5) wound infection 6) systemic disease Microscopy pyogenic, not toxin Can grown on non-selective agar S. aureus grows on mannitol-salt agar On blood agar, is B-hemolytic Oxacillin, vancomycin Abscess must be identified and drained Patients with food poisoning are only treated for symptoms Proper cleansing of wound and hand washing
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Physiology/Structure
Streptococcus pyogenes Gram positive, cocci, B-hemolytic
Pathogenesis/Immuni ty
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Arranged in pairs/chains Facultative anaerobes with complex nutritional requirements (blood/serum agar) Ferment carbohydrates and produce lactic acid, catalase negative Classified based on 1) serologic properties (Lancefield grouping) 2) hemolytic patterns complete B, incomplete A and no G 3) biochemical properties (CAMP reaction) Specific carbohydrate (A antigen) and specific proteins (M protein) in cell wall Avoids phagocytosis by capsule, M protein and C5a peptidase 1) hyaluronic acid capsule poor immunogen interfering with phagocytosis 2) conserved region of M protein binds to serum B-globulin factor H 3) C5a peptidase disrupts mediation of inflammation Adhere to and invade host cell by M protein, lipoteichoic acid and F protein internalization is believed to be the cause of persistent infection (recurrent strep throat) Produce toxins by exotoxins, streptolysin S/O, DNases 1) streptococcal pyrogenic exotoxin (Spe) similar to C. diptheriae 2) streptolysin S oxygen stable/nonimmunogenic, can lyse RBC, WBC and platelets 3) streptolysin O oxygen stable, can lyse RBC, WBC, platelets and cultured cells, antibodies readily formed against 4) streptokinase A and B, lyse plasminogen cleaves fibrin/fibrinogen lyse clots 5) DNase A through D, depolymerize free DNA in pus Colonization in upper respiratory tract and skin Person to person spread by respiratory droplets and vectors Children at risk age 2-15, people with skin infections, patients with prior strep infections Pharyngitis and soft tissue infection M protein strains Erysipelas (erythema, bullae) Impetigo, necrotizing fascilitis Scarlet fever rash on tongue and skin Rheumatic fever Microscopy for soft tissue infection Direct test for Group A infection, negatives must be cultured Catalase test used to confirm positives Antistreptolysin O (ASO) test confirm rheumatic fever, glomerulonephritis Anti-DNase B Test Penicillin, cephalosporin, vancomycin Beginning therapy within 10 days prevent rheumatic fever (prophylaxis for patients with history of fever)
Physiology/Structure
Pathogenesis/Immuni ty
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Streptococcus pneumoniae Elongated diplococci, gram positive Teichoic acid rich with amidase (autolytic) in cell wall Catalase negative 1) Colonizes oropharynx surface protein adhesion 2) Spread into normally sterile tissue pneumolysin, IgA protease 3) Local inflammation teichoic acid, peptidoglycan, pneumolysin 4) Evade phagocytes polysaccharide capsule Spread or naso/oropharynx to distal sites (lungs, ears, sinuses) Person to person spread is rare Individuals that cannot clear respiratory tract are at higher risk Children/elderly most susceptible to meningitis Patients with hematologic disorder and functional asplenia are at risk More common during cooler months Pneumonia Sinusitis Otitis media Meningitis Bacteremia Microscopy is highly useful not for patients treated with antibiotics Antigen test for pneumococcal C polysaccharide Chest X-ray Catalase test, optochin test, solubility in bile Penicillin, fluoroquinolone, vancomycin/ceftriaxone Vaccines
Physiology/Structur
Enterococci faecalis & faecium Gram positive cocci seen in pairs or short chain
e Pathogenesis/Immu nity
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Group D cell wall antigen glycerol teichoic acid associated with plasma membrane Adhere to host surfaces 1) aggregation substance hairlike protein facilitating plasmid exchange and binding to epithelial cells 2) enterococcal surface protein collagen binding adhesin 3) carbohydrate adhesin binding to hosts Secrete cytolysins and proteases tissue damage 1) cytolysin inhibits growth of gram positive bacteria 2) pheromone chemical attractant for neutrophils 3) gelatinase hydrolyzes gelatin, collagen and hemoglobin Antibiotic resistant to aminoglycosides, B-lactams, vancomycin Colonizes GI tract and mucosa of humans/animals Survives on surfaces for long time Infections result from patients normal flora Patients with other infection or on broad-spectrum antibiotics are most at risk Urinary tract infection pyuria (pus) and dysuria (pain), common in patients with catheters Wound infection (intrabdomical and polymicrobic) abdominal swelling/pain following surgery or trauma Bacteremia Endocarditis infection of heart endothelium or valves, acute or chronic *not usually deadly bacteria Grows well on nonselective media Catalase negative PYR positive Resistant to bile and optochin Combination of aminoglycoside with cell-wall active antibiotic like penicillin/ampicillin or vancomycin New drugs like linezolid, dalfopristin and fluoroquinolones
Physiology/Structure Pathogenesis/Immuni ty
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Corynebacterium diphtheriae Gram positive rods, pleomorphic Diphtheria toxin A-B exotoxin that inhibits protein synthesis, travels through blood Tox gene codes for exotoxin via lysogenic bacteriophage (B-phage) Two step process: 1) cleavage of toxin protein during secretion from bacterial cell 2) cleavage of toxin molecule into 2 polypeptides (A and B) attached by disulfide bone A-B exotoxin Organism does not need to enter blood to cause disease Asymptomatic carriers worldwide in oropharynx and skin Human only known carriers Spread person to person via contact and respiratory droplets More common in unvaccinated people and urban close-living areas Uncommon in U.S. Diphtheria respiratory or cutaneous Respiratory sudden onset with sore throat, fever, phlegm in throat and discomfort Cutaneous papule leading to non-healing ulcer maybe systemic symptoms Microscopy is nonspecific may see metachromatic granules Culture on nonselective (blood) agar and selective (cysteine-tullerite, Tinsdale) agar ID based on presence of cysteinase Most follow up with biochemical testing Extoxin observed via PCR or Elek test Diphtheria antitoxin neutralize toxin Penicillin, erythromycin kill bacteria stopping toxin production Immunization stimulate antibody production (for whole susceptible population as well) Booster shots
Physiology/Structure
Pathogenesis/Immuni ty
Epidemiology
Clinical Disease
Lab Diagnosis Treatment, Prevention, Control
Neisseria gonorrhoeae Gram negative, diplococci Fastidious growth requirements 35oC, humid, O2 and CO2 rich Oxidase and catalase positive, acid producing by oxidation of glucose Outer surface is antigen rich 1) proteins pili (initial attachment), Por (prevent phago-lysozome fusion), Opa (mediates attachment to eukaryotic cells), Rmp (protects antigens from antibiotics) 2) protein receptors for: transferrin, lactoferrin, hemoglobin acquire iron 3) lipooligosaccharide endotoxin 4) immunoglobulin protease destroys IgA 5) B-lactamase hydrolyzes B-lactam ring in penicillin Strictly a human pathogen Attach and penetrate mucosal cells, passing through to subepithelial space Pili, Por and Opa facilitate penetration LOS stimulates release of cytokine (TNF-a) which causes most associated symptoms Humans are the only hosts Women carriers can be asymptomatic but are more at risk to acquire disease Transmission is mainly sexual (2nd top STD) Most common in blacks, age 15-24, southeastern U.S., promiscuous individuals Patients with complement deficiency disseminated infection Gonorrhea purulent discharge from involved site (cervix, urethra, anus) Spreading of infection through blood to skin or joints, rash and/or arthritis Ophthalmia neonatorum eye infection acquired by infant at birth Gram stain in symptomatic males only Culturing is sensitive/specific replaced by nucleic acid amplification assay Ceftriaxone If patient has Chlamydia too, use doxycycline or azithromycin as well Neonates get silver nitrate prophylactically No vaccines available Education on safe-sex practices needed and follow up with all sexual partners
Neisseria meningitides
Physiology/Structure
Pathogenesis/Immuni ty
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Gram negative diplococci Fastidious growth requirements 35oC, humid, O2 and CO2 rich Oxidase and catalase positive, acid producing by oxidation of glucose and maltose Polysaccharide capsule prevents antibody mediated phagocytosis Pili allow for colonization of nasopharynx Endotoxin LOS Humans are only natural hosts Person to person spread via respiratory droplets in the air Most common in children under 5, nursing home patients Occurs worldwide but most often in dry, cold seasons Meningitis pus-filled inflammation of meninges, headache fever (high mortality) Meningococcemia thrombosis of small blood vessels, skin lesions Pneumonia occurs in patients with underlying bronchial disease Gram stain of CSF (too few organisms present) Culture is definitive but organism dies quickly Detection of antigens is insensitive and nonspecific Breast-fed infants have passive immunity Penicillin Prophylaxis with Rifampin, ciprofloxacin Vaccine (not available for serotype B)
Physiology/Structure
Mycobacterium tuberculosis Lipid rich cell wall that is very complex (similar to gram positive w/ thick peptidoglycan layer)
Pathogenesis/Immuni ty
Epidemiology
Clinical Disease Lab Diagnosis
Treatment, Prevention, Control
Lipoarabinomannan (LAM) protein anchored to cell wall, similar to O-antigen of LPS Acid fast, aerobic, fastidious Presence of mycolic acids w/ 70-90 carbons 61-71% guanine-cytosine in DNA Intracellular bacteria that establishes lifelong infection Enters alveoli and is phagocytozed by alveolar macrophages Prevents phagolysozome fusion but fuses with other vacuoles for nutrition Survives by forming reactive nitrogen intermediates formed between nitric oxide and superoxide anions Macrophages are activated secrete IL-12, TNF-, T cells and NK cells arrive TH1 differentiation INF- Granuloma formation alveolar macrophages, epitheloid cells, Langhans giant cells w/ intracellular bacteria form necrotic mass, surrounded by CD4, CD8 and NK cells If the granuloma is small, bacteria are killed but if large, killing by macrophages is prevented and the bacteria lie dormant until patients immune system is susceptible 1/3 of world is infected Most common is Southern Asia, Africa and Eastern Europe Most susceptible are those with HIV, drug/alcohol abusers, homeless Humans are only reservoirs and can be spread person-person by aerosols Tuberculosis Purified protein derivatives (PPD skin test) IFN - release tests Microscopy/culture sensitive/specific Species-specific molecular probes Chest x-ray Acid fast staining w/ carbolfuchsin and fluorescent dyes (auramine and rhodamine) Isoniazid, ethambutol, pyrazinamide, rifampin for 2 months followed by 4-6 months of more antibiotics Prophylaxis Immunoprophylaxis for endemic countries Control of disease via health departments
Physiology/Structure Pathogenesis/Immuni ty
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Mycobacterium leprae Weakly gram positive, acid fast rods Lipid rich cell wall Tuberculoid forms results in few bacteria but severe immune reponse many granulomas and lymphocytes Usually elicits cytokine production macrophage activation phagocytosis bacillary clearance Found in Nepal, India and Brazil Lepromatous form is highly infection (not tuberculoid) Person-person spread through aerosols or direct contact Disease is primarily from host response to infection Tuberculoid Lepromatous Unable to be cultured Microscopy is useful for lepromatous form Skin testing confirms tuberculoid Prompt recognition and treatment is key Antibiotic therapy longer and use of multiple drugs for lepromatous form
Physiology/Structure Pathogenesis/Immuni ty Epidemiology
Mycobacterium avium Weakly gram positive, acid fast rods Lipid rich cell wall Disease primarily from host response to infection Problematic in AIDS patients, immunocompromised, existing pulmonary disease Seen where TB is less common Aquired through ingestion of contaminated food/water Asymptomatic colonization Chronic pulmonary disease Solitary nodule or disseminated Microscopy and culture sensitive and specific Combination antibiotic therapy for long period Prophylaxis in AIDS patients
Clinical Disease
Lab Diagnosis Treatment, Prevention, Control
Physiology/Structur e Pathogenesis/Immu nity Epidemiology
Clinical Disease
Lab Diagnosis Treatment, Prevention, Control
Enterobacteriaceae Salmonella typhi Gram negative rods, bipolar staining Facultative anaerobe Fermenter, oxidase negative More than 2500 O serotypes LPS Tolerant of acids in phagocytes Can survive within macrophages and disseminate throughout body Ubiquitous found in soil, water and intestinal flora Originate from animal reservoir or human carrier Eating contaminated food, especially poultry, eggs and dairy Fecal-oral spread Patients on antacid therapy and the immunocompromised are most susceptible Infection most common during warm months Always associated with human disease Bacteremia Urinary tract infection Enteritis fever, nausea, vomiting, diarrhea Enteric fever Asymptomatic colonization Isolation from stool specimen on selective media Antibiotics Proper preparation of food avoiding contamination Vaccination Enterobacteriaceae Escherichia coli
Physiology/Structur e Pathogenesis/Immu nity Epidemiology Clinical Disease
Gram negative Facultative anaerobe Fermenter, oxidase negative Can acquire virulence factors from plasmids and bacteriophages LPS: O-polysaccharide, core polysaccharide, lipid A (endotoxin) Endogenous spread of organism is susceptible patient Most common organism found in GI tract Normal commensal flora that cause opportunistic infections Hemmorhagic coilitis Hemolytic uremic syndrome
Lab Diagnosis Treatment, Prevention, Control
Gastroenteritis 1) enterotoxigenic enterotoxin causing diarrhea (small intestine) 2) enteropathogenic disruption of microvilli causing diarrhea (small intestine) 3) enteroaggregative adherence of rods causing diarrhea (small intestine) 4) enterohemmorhagic Shiga toxins disrupt protein synthesis causing bloody diarrhea (large intestine) 5) enteroinvasive destruction of epithelial lining in colon causing bloody diarrhea (large intestine) Grow rapidly on most media Pathogenic strains are detected on in research labs Treated symptomatically unless disease disseminated Infection control practices to reduce nosocomial infection Proper hygienic methods and cooking of beef products (EHEC) Enterobacteriaceae Shigella
Physiology/Structur e Pathogenesis/Immu nity Epidemiology
Clinical Disease
Lab Diagnosis Treatment, Prevention, Control
Gram negative rod Facultative anaerobe Fermenter, oxidase negative LPS S. diphtherieae produces Shiga toxin (exotoxin) which disrupts protein synthesis/endothelial damage Originate from human carrier Spread person-person Fecal-oral spread Those at risk are young children in day cares or schools, male homosexuals Occurs worldwide in no particular season Always associated with human disease Gastroenteritis diarrhea, tenesmus Bacterial dysentery Asymptomatic carriage Isolation from stool specimen on selective media Antibiotics In vitro susceptibility tests Empiric therapy fluoroquinolones Infection control and hygienic measures
Vibrio Cholerae Physiology/Structur e Pathogenesis/Immu nity Curved rods, gram negative Fermentative, facultative anaerobes, require salt Single polar flagellum 1) produce cholera toxin similar to E. coli enterotoxin -bacteriophage CTX encodes gene for toxin A and B -bacteriophage binds to pilus and enters cell integrating genome -bacteriophage is lysogenic ace gene (accessory cholera toxin), zot gene (zonula toxin), cep gene (chemotaxis) -5 identical B subunits of cholera toxin bind to GM1 receptor on intestinal epithelial cells -A subunit is internalized and facilitates ATPcAMP -results in hypersecretion of water and electrolytes (can lose up to 1 liter per day) 2) express toxin pili -adhere to mucosal cell layer via pili and chemotaxis proteins Serotype O1/O139 responsible for pandemics Found in marine environment, especially where shellfish are present Levels in water increase during summer Spread via eating/drinking contaminated items Infectious dose required is high so person-person spread not likely Cholera water diarrhea (rice water stools containing little protein w. fishy odor), vomiting resulting in severe dehydration/acidosis/shock/anuria/muscle cramping/low BP (O1) Gastroenteritis milder form when strain is toxin negative (non-O1) Culture of stool is not helpful because organism too dilute Should be performed early in onset keeping stool at neutral-alkaline pH Fluid/electrolyte replacement Antibiotics Improve hygiene Vaccine provides limited protection and herd immunity
Epidemiology
Clinical Disease Lab Diagnosis Treatment, Prevention, Control
Helicobacter pylori Physiology/Structur e Pathogenesis/Immu nity Curved rod, gram negative Also have coccoid form Produces urease Multiple layer unipolar flagellum Gastric colonization pass through gastric mucus and adhere to epithelial cells Inflammation IL-8 production which attracts neutrophils release proteases and ROS Alteration of acid production bacterial acid inhibition protein, neutralization of acid by ammonia produced by urease Tissue destruction mediated by urease byproducts (mucinase, phospholipases, vacuolating cytotoxin A) Common especially in those of low socioeconomic class/developing nations Humans are primary reservoir Typical oral-fecal spread Ubiquitous/worldwide, not seasonal Acute gastritis Chronic gastritis Peptic ulcers Gastric adenocarcinoma MALT lymphoma Microscopy is sensitive and specific Urease test/urease breath test Antigen test w/ stool sample Cultures require microaerophilic environment, hard to grow Serology Proton-pump inhibitor + macrolide + B-lactam for 2 weeks No vaccine
Epidemiology
Clinical Disease
Lab Diagnosis
Treatment, Prevention, Control
Physiology/Structur e
Pathogenesis/Immu nity
Epidemiology
Clinical Disease
Lab Diagnosis Treatment, Prevention, Control
Pseudomonas aeruginosa Gram negative diplo-bacillus Simple nutrition Colonies produce diffusable pigments pyocyanin blue, pyorubin red Typically motile Obligate aerobes Oxidase positive Mucoid appearance due to polysaccharide capsule (cystic fibrosis) Opportunistic infecting patients on broad-spectrum antibiotics 1) adhesins - flagella, pili, LPS - alginate capsule 2) secrete toxin/enzyme - type III secretion system can inject toxins into host cell - exotoxin A, cyanins, protease, phopholipase 3) antimicrobial resistance Ubiquitous found in nature Not part of human flora but found often in hospital settings (nosocomial) Not seasonal Transiently colonizes respiratory and GI tract Skin infection existing wounds or burns Folliculitis Lung infection mild to necrotizing UTI/ear or eye infection Bacteremia Grows rapidly on most media IDd by colony characterisitics B hemolysins, pigment, grape odor Biochemical testing oxidase Resistant to most antibiotics Must use multi-drug therapy Hospital efforts necessary to minimize contamination
Haemophilus influenzae
Physiology/Structur e Pathogenesis/Immu nity
Epidemiology
Clinical Disease Lab Diagnosis Treatment, Prevention, Control
Small, pleomorphic, gram negative rods Requires hemin (X factor) and NAD (V factor) to grow Polysaccharide capsule LPS w/ endotoxin activity can damage cilia of epithelium 6 serotypes (A-F) B commonly responsible for most infections because it contains polyribitol phosphate Adhere to host cell via pili and other adhesins Bacteria can pass through epi/endothelial cell wall to enter circulation *opsonic antibodies (1st defense) are needed to break capsule Found on mucous membranes of humans encapsulated strain is problematic and not normal Spread locally to cause disease in ear, eye sinuses and throat Disseminated disease is uncommon but can occur in unvaccinated children, eliminated Most at risk are those lacking antibodies or complement, have undergone splenectomy Meningitis unimmunized children Epiglottitis unimmunized children, possible obstruction of airways Pneumonia in elderly with other respiratory condition Use gently heat sheep blood agar chocolate agar Bacterium isolated from CSF, synovial fluid and lower respiratory tract Antigen tests are only for type B H. infuenzae Type B Vaccine (HIB) conjugated PRP Broad spectrum cephalosporins
Legionella pneumophila
Physiology/Structur e
Pathogenesis/Immu nity
Epidemiology
Clinical Disease Lab Diagnosis
Treatment, Prevention, Control
Thin, pleopmorphic, gram negative rods Stain with Dieterle silver stain Obligate aerobes Fastidious - require L-cysteine and iron to grow Non-fermentative, get energy from amino acid metabolism Serotypes 1-6 commonly isolated (1 and 6 are most problematic) Acquire iron from host cell Like lungs alveolar cells Intracellular parasites multiply in amoeba, alveolar macrophages/epithelial cells, monocytes -complement C3b (humoral) deposited on bacterial surface -bacteria bind to CR3 receptor on Monocyte Phagolysozome fusion is inhibited Chemokines/cytokines produce severe inflammation Multiply in vacuoles and produce proteolytic enzymes that kill host Immunity is mainly CELL-mediated (TH1 activate macrophage IFN- Half of species (25 genus) implicated in human disease Pneumophila causes 90% of disease Inhale infectious aerosols from water (cooling towers, AC units) Sporadic, epidemic, nosocomial Patients with existing lung conditions are most at risk Legionnaires disease rapid pneumonia Pontiac Fever influenza like, not deadly Growth on supplemented media buffered charcoal yeast extract (BCYE) Culture sputum or blood NO microscopy Antigen test for serotype 1 ELISA of urine Nucleic acid amplification assay Serology study of antibodies FAT/ELISA of serum Macrolides Reduce environmental exposure superheating, hyperchlorination
Clostridium perfringens Physiology/Structur Gram positive rods
e Pathogenesis/Immu nity Epidemiology Clinical Disease Lab Diagnosis
Treatment, Prevention, Control
Type A strain cause most human infections Spore formation Grow well in nutritionally rich, oxygen poor environment like dead tissue Produce histolytic toxin, enterotoxin (bind to small intestine receptors), neurotoxin Ubiquitous in soil, water and sewage Wound infection Colitis/diarrhea due to enterotoxin Gas gangrene Gram staining Grow well in culture sheep blood agar (theta) hemolysis complete - (alpha) hemolysis partial Surgical debridement Penicillin Symptomatic for food poisoning
Clostridium tetani Physiology/Structur e Pathogenesis/Immu nity Epidemiology Clinical Disease Lab Diagnosis Treatment, Prevention, Control Gram positive rods Tetanospasmin neurotoxin that blocks release of neurotransmitters Ubiquitous as they colonize soil and GI tract of humans Disease common in developing countries where access to vaccine is poor Having the disease does NOT induce immunity Tetanus severe, constant muscle spasms (ANS), risus sardonicus (facial muscle spasm) Neonatal tetanus Difficult to grow in culture Based on clinical presentation Toxin/antibodies not detected Surgical debridement Antiobiotics Immunization w/ antitoxin globulin and vaccination with tetanus toxoid Booster every 10 years
Clostridium botulinum Physiology/Structur e Pathogenesis/Immu nity Epidemiology Gram positive rods Botulinum toxins A to G (commonly A and B) Prevents release of ACh flaccid paralysis Ubiquitous in soil Transmission through contaminated foods (especially canned) Inhalation of spores Most common is developing countries Botulism Infant botulism consumption of contaminated foods like honey Wound infection Detection of toxin in serum, feces, vomit Metronidazole or penicillin Keep foods at acidic pH, store at 4oC and add preservatives Toxin is heat sensitive and can be destroyed by cooking Clostridium dificile Physiology/Structur e Pathogenesis/Immu nity Gram positive rods Produce two toxins 1) enterotoxin attract neutrophils, release of cytokines 2) cytotoxin increases intestinal wall permeability spore formation antibiotic resistance allows the bacterium to overgrow in GI tract Colonize the GI tract of some individuals Disease caused by overgrowth due to antibiotic therapy Spores found in environment Highly virulent strain found CDif Antibiotic associated diarrhea Pseudomembranous colitis Detecting enterotoxin or cytotoxin Stop current antibiotic Relapse is common as antibiotics cannot kills spores Cleaning of infected room Bacteroides fragilis
Clinical Disease Lab Diagnosis Treatment, Prevention, Control
Epidemiology
Clinical Disease Lab Diagnosis Treatment, Prevention, Control
Physiology/Structur e
Pathogenesis/Immu nity
Epidemiology Clinical Disease
Lab Diagnosis Treatment, Prevention, Control
Pleomorphic gram negative rods Anaerobic Polysaccharide capsule Grow in 20% bile Hydrolyze esculin LPS NO endotoxin activity because lipid A is missing phosphate groups Adhesins 1) adhere to peritoneal surfaces 2) epithelial cells 3) extracellular molecules (fibrinogen, lactoferrin) via fimbriae pro-inflammatory cytokines (TNF- and IL-1 ) Capsule and short chain fatty acids prevents phagocytosis Have catalase (neutralize hydrogen peroxide) and superoxide dismutase (neutralize superoxide free radicals) Cytotoxic enzymes tissue destruction Enterotoxin 1) zinc metalloprotease toxin morphological changes to GI epithelium resulting in diarrhea chloride secretion is required to maintain surfactant in lungs and negativity of the cell 2) IL-8 secretion causing inflammation Part of normal GI flora Produce disease when moving from GI tract to sterile site Intra-abdominal infection Respiratory tract infection Brain abscess Skin infection Rarely isolated in clinical specimens Microscopy and culture Biochemical ID gram stain, colony morphology, resistance to antibiotics, growth in bile Surgical debridement and antibiotic therapy Produce B-lactamase so NO penicillins
Physiology/Structur e
Pathogenesis/Immu nity
Epidemiology
Clinical Disease Lab Diagnosis Treatment, Prevention, Control
Chlamydiaceae (trachomatis) Obligate intracellular parasites very small Similar to gram negatives w/ inner and outer membrane (NO peptidoglycan) Have both DNA and RNA Have prokaryotic ribosomes Synthesize own proteins, lipids and NA LPS Unique development - metabolically inactive/infectious elementary bodies (EB) - metabolically active/noninfectious reticulate bodies (RB) infects non-ciliated columnar, cuboidal and transitional epithelial cells prevents phagolysozome fusion Three species responsible for human disease 1) Chlamydia trachomatis 2) Chlamydophila psittaci 3) Chlamydophila pneuomoniae Most common STD in US (ocular present in Africa, Asia, Middle East) Trachoma chronic inflammation of eye surface leading to ulcers, scarring and blindness Lymphogranuloma venereum painless ulcer that heals, then systemic symptoms Culture and antigen testing is specific, NOT senstivie Molecular amplification test is best method Susceptible to most antibiotics Safe sex practices and treatment of partner(s)
You might also like
- Gram-positive bacteria of medical importance overviewDocument58 pagesGram-positive bacteria of medical importance overviewGx NavinNo ratings yet
- Immuno SeroDocument80 pagesImmuno SeroDocAxi Maximo Jr AxibalNo ratings yet
- IMS - Immunomodulation & ImmunodeficienciesDocument3 pagesIMS - Immunomodulation & ImmunodeficienciesJeanne RodiñoNo ratings yet
- A. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusDocument8 pagesA. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusRuel MaddawinNo ratings yet
- Serologic Tests Part 1Document4 pagesSerologic Tests Part 1Joshua TrinidadNo ratings yet
- (Microbio) Staphyloccocus and Streptococcus-Dr. Salandanan (BHND)Document16 pages(Microbio) Staphyloccocus and Streptococcus-Dr. Salandanan (BHND)Lee Delos Santos100% (1)
- Gram Positive Cocci Sem 1 1Document45 pagesGram Positive Cocci Sem 1 1Charmaine Corpuz Granil100% (1)
- MICROBIOLOGY MEDIADocument3 pagesMICROBIOLOGY MEDIAAisle Malibiran PalerNo ratings yet
- Gram Negative Cocci (Lecture Notes)Document5 pagesGram Negative Cocci (Lecture Notes)Dayledaniel Sorveto100% (1)
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua TrinidadNo ratings yet
- 3 SEMR421 Bacteriology Part 3Document14 pages3 SEMR421 Bacteriology Part 3Micah Daniel TapiaNo ratings yet
- Microbiology MnemonicsDocument5 pagesMicrobiology MnemonicsFritzel SusbillaNo ratings yet
- Bacteriology Study SheetDocument50 pagesBacteriology Study Sheetvishal_life27100% (5)
- Using Colonial Morphology to Presumptively ID MicroorganismsDocument6 pagesUsing Colonial Morphology to Presumptively ID MicroorganismsJean BelciñaNo ratings yet
- The Medically Important MycosesDocument8 pagesThe Medically Important MycosesNatasha JeanNo ratings yet
- S. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusDocument14 pagesS. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusMugiNo ratings yet
- IMS - Intro To Immunology and SerologyDocument3 pagesIMS - Intro To Immunology and SerologyJeanne RodiñoNo ratings yet
- Hematology Tables Morphology of RBCsDocument5 pagesHematology Tables Morphology of RBCsGlydenne Glaire Poncardas GayamNo ratings yet
- Review Parasitology ChartsDocument8 pagesReview Parasitology Chartseezah100% (2)
- Bacteriology SummaryDocument35 pagesBacteriology SummarykevinNo ratings yet
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- Viral Basics and Replication CyclesDocument21 pagesViral Basics and Replication CyclesfrabziNo ratings yet
- Bacteria Study Guide: Cell Structure, Growth, Detection & IdentificationDocument11 pagesBacteria Study Guide: Cell Structure, Growth, Detection & IdentificationCarmelle Zia Reyes100% (1)
- Mycology and VirologyDocument8 pagesMycology and VirologyMaybelle Acap PatnubayNo ratings yet
- Clinical Microscopy ExamDocument3 pagesClinical Microscopy ExamKarla GiorlaNo ratings yet
- Chapter 2 Introduction To Urinalysis PDFDocument4 pagesChapter 2 Introduction To Urinalysis PDFJulie Anne Soro ValdezNo ratings yet
- Mtap - Bacteriology FinalsDocument6 pagesMtap - Bacteriology FinalsMoira Pauline LibroraniaNo ratings yet
- AnemiaDocument9 pagesAnemiaMila Canoza HerreraNo ratings yet
- MUST KNOW FUNGAL ID TERMSDocument16 pagesMUST KNOW FUNGAL ID TERMSJustine Alexandrea RamirezNo ratings yet
- HistotechniquesDocument9 pagesHistotechniquesDivineGloryMalbuyoNo ratings yet
- Agents of Mycoses Identification and CharacteristicsDocument44 pagesAgents of Mycoses Identification and CharacteristicsRia AlcantaraNo ratings yet
- HematologyDocument5 pagesHematologyIvy Jan OcateNo ratings yet
- A. Neisseria Gonorrhoeae B. Moraxella Catarrhalis C. Neisseria Meningitidis D. Neisseria LactamicaDocument7 pagesA. Neisseria Gonorrhoeae B. Moraxella Catarrhalis C. Neisseria Meningitidis D. Neisseria LactamicaWynlor AbarcaNo ratings yet
- AUBF Finals Vaginal SecretionsDocument37 pagesAUBF Finals Vaginal SecretionsLyra Dennise LlidoNo ratings yet
- 5 Must To Know in Clinical Micros PDFDocument43 pages5 Must To Know in Clinical Micros PDFYelai CarveroNo ratings yet
- Bacteriology Final Coaching Notes 2Document9 pagesBacteriology Final Coaching Notes 2Mylene TamoriteNo ratings yet
- AUB - Microscopic Analysis of UrineDocument4 pagesAUB - Microscopic Analysis of UrineJeanne Rodiño100% (1)
- General Pathology Lecture Group 1 HandoutDocument6 pagesGeneral Pathology Lecture Group 1 HandoutCecille AnnNo ratings yet
- Gram Negative Rods GuideDocument8 pagesGram Negative Rods GuideRuel Maddawin100% (1)
- Bacte TestDocument10 pagesBacte TestRiondalionNo ratings yet
- Introduction to Pathology and Disease MechanismsDocument17 pagesIntroduction to Pathology and Disease MechanismsAngela ReyesNo ratings yet
- Compre HistopatDocument21 pagesCompre HistopatMark FuerteNo ratings yet
- Family of StreptococcaceaeDocument10 pagesFamily of StreptococcaceaeLovely B. AlipatNo ratings yet
- Parasitology-Lec 8 TaeniaDocument7 pagesParasitology-Lec 8 Taeniaapi-3743217100% (3)
- Bacteriology Genera Visualized by Bright-Field MicroscopeDocument6 pagesBacteriology Genera Visualized by Bright-Field MicroscopeRachelle AbonalesNo ratings yet
- Common Fungal OpportunistsDocument7 pagesCommon Fungal OpportunistsAlliah Erika DoydoraNo ratings yet
- Immunology Serology ReviewDocument211 pagesImmunology Serology ReviewRachel Marie M. Gania100% (1)
- Staphylococcus Spp. Gram Positive. ClusteredDocument15 pagesStaphylococcus Spp. Gram Positive. ClusteredIvy NNo ratings yet
- Coagulation NotesDocument14 pagesCoagulation NotesthrowawyNo ratings yet
- MUST To KNOW in Histopathology1 PDFDocument34 pagesMUST To KNOW in Histopathology1 PDFEdel Gannaban BinasoyNo ratings yet
- Clin Path Lab 6 Urinalysis Part 2Document7 pagesClin Path Lab 6 Urinalysis Part 2api-3743217100% (3)
- Microbio Lec 1 - Bacterial Morphology and Ultra StructureDocument8 pagesMicrobio Lec 1 - Bacterial Morphology and Ultra Structureapi-3743217100% (3)
- Biochemical Test MicrobiologyDocument2 pagesBiochemical Test MicrobiologyGab BautistaNo ratings yet
- Senior Medical Laboratory Technician: Passbooks Study GuideFrom EverandSenior Medical Laboratory Technician: Passbooks Study GuideNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Safe Blood: Purifying the Nations Blood Supply in the Age of AFrom EverandSafe Blood: Purifying the Nations Blood Supply in the Age of ANo ratings yet
- The Difference and Antibacterial Property of Human Tears and Eggwhites Against Staphylococcus AureusDocument51 pagesThe Difference and Antibacterial Property of Human Tears and Eggwhites Against Staphylococcus AureusNikos BelenNo ratings yet
- Ecoli - Risk AssesmentDocument16 pagesEcoli - Risk AssesmentZsuzsa KomlóNo ratings yet
- Production of Pharmaceutical Compounds Through Microbial FermentationDocument2 pagesProduction of Pharmaceutical Compounds Through Microbial FermentationSAFC-Global100% (1)
- Antibacterial Activity of Papaya Flower Extract Against E. coliDocument28 pagesAntibacterial Activity of Papaya Flower Extract Against E. coliJairah Mapa BerbosoNo ratings yet
- 6 - Application of Bacillus Spp. Isolated From The Intestine of Black Tiger Shrimp (Penaeus Monodon Fabricius From Natural Habitat For Control Pathogenic Bacteria in Aquaculture-1Document8 pages6 - Application of Bacillus Spp. Isolated From The Intestine of Black Tiger Shrimp (Penaeus Monodon Fabricius From Natural Habitat For Control Pathogenic Bacteria in Aquaculture-1Nguyen Van MinhNo ratings yet
- Viome Sample ReportDocument48 pagesViome Sample ReportshanmugapriyaNo ratings yet
- Pharmacology and Venipuncture Nosocomial InfectionDocument55 pagesPharmacology and Venipuncture Nosocomial InfectionArvic Pascua MaltizoNo ratings yet
- Nghiên Cứu Đặc Tính Kháng Khuẩn Của Tinh Dầu Tràm Trà Và Khả Năng Ứng Dụng Trong Mỹ Phẩm - 1149008Document8 pagesNghiên Cứu Đặc Tính Kháng Khuẩn Của Tinh Dầu Tràm Trà Và Khả Năng Ứng Dụng Trong Mỹ Phẩm - 1149008Đường Thị Đoan TrangNo ratings yet
- Biosafety HazardDocument27 pagesBiosafety HazardMuhammad ArshadNo ratings yet
- 3 Peekate and Chilowe 2016 JABU 7Document9 pages3 Peekate and Chilowe 2016 JABU 7Lekeah Pedro PehkatehNo ratings yet
- Vacuum: Chaitanya B. Hiragond, Anuraj S. Kshirsagar, Vividha V. Dhapte, Tanaya Khanna, Prasad Joshi, Priyesh V. MoreDocument8 pagesVacuum: Chaitanya B. Hiragond, Anuraj S. Kshirsagar, Vividha V. Dhapte, Tanaya Khanna, Prasad Joshi, Priyesh V. MorezibaNo ratings yet
- Role of Probiotics in AquacultureDocument24 pagesRole of Probiotics in AquacultureGopi NuthalapatiNo ratings yet
- MICROBIOLOGY BOARD EXAM QUESTIONSDocument6 pagesMICROBIOLOGY BOARD EXAM QUESTIONSchristinejoan100% (1)
- Prokaryotes and EukaryotesDocument6 pagesProkaryotes and EukaryotesC Bala DiwakeshNo ratings yet
- Antimicrobial Activity of Some Commonly Used Indian SpicesDocument6 pagesAntimicrobial Activity of Some Commonly Used Indian SpicesSalmaNo ratings yet
- DISTINCTIVE PHARMACOLOGICAL ACTIVITIES OF Eclipta Alba AND IT'S COUMESTAN WEDELOLACTONEDocument7 pagesDISTINCTIVE PHARMACOLOGICAL ACTIVITIES OF Eclipta Alba AND IT'S COUMESTAN WEDELOLACTONEBaru Chandrasekhar RaoNo ratings yet
- Acido HipoclorosoDocument20 pagesAcido HipoclorosorxnlrNo ratings yet
- Glossary by Category: AbcdefghijklmnopqrstuvwxyzDocument31 pagesGlossary by Category: Abcdefghijklmnopqrstuvwxyzkaivalya chaaitanya ugaleNo ratings yet
- Highlight Your Results: With VITEK 2 ID CardsDocument2 pagesHighlight Your Results: With VITEK 2 ID CardsBrijeshNo ratings yet
- Classification of Microorganisms: Prokaryotes vs EukaryotesDocument40 pagesClassification of Microorganisms: Prokaryotes vs EukaryotesRadwa MohamedNo ratings yet
- USMLE Practice Questions on BacteriologyDocument67 pagesUSMLE Practice Questions on BacteriologyKiran KrupaNo ratings yet
- Lec 1Document11 pagesLec 1Ahmed JamalNo ratings yet
- PAG7 1 Student The Effects of Antibiotics On Microbial Growth v1 0Document3 pagesPAG7 1 Student The Effects of Antibiotics On Microbial Growth v1 0Kutezz C MikeNo ratings yet
- In Vitro in VitroDocument11 pagesIn Vitro in VitroJohn MacioNo ratings yet
- Bacterial Transformation MechanismsDocument14 pagesBacterial Transformation MechanismsSHAIKHNo ratings yet
- Prospectus Syllabus: Post Graduate Diploma Course in Food Analysis and Quality AssuranceDocument19 pagesProspectus Syllabus: Post Graduate Diploma Course in Food Analysis and Quality Assurancepriyanka thapliyal100% (1)
- Process Considerations On The Application of High Pressure Treatment at Elevated Temperature Levels For Food PreservationDocument102 pagesProcess Considerations On The Application of High Pressure Treatment at Elevated Temperature Levels For Food PreservationWilliam Rolando Miranda ZamoraNo ratings yet
- Aynadis Thesis CorrectedDocument78 pagesAynadis Thesis CorrectedBantider GetachewNo ratings yet
- Virus NotesDocument6 pagesVirus NotesHuiqing TeoNo ratings yet
- Chapter 4-Food Spoilage: Chemical and Biological Spoilage Spoilage in Canned FoodsDocument20 pagesChapter 4-Food Spoilage: Chemical and Biological Spoilage Spoilage in Canned FoodsDaniel IsmailNo ratings yet