Professional Documents
Culture Documents
Foundations Midterm Study Guide
Uploaded by
Khooshbu PatelOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Foundations Midterm Study Guide
Uploaded by
Khooshbu PatelCopyright:
Available Formats
CHAPTER 1 Introduction to Nursing Describe the historic background of nursing Early civilizations illness had supernatural causes o Theory
ry of Animism cause of mysterious changes in bodily functions everything in nature was alive with invisible forces and endowed with power. Good spirits brought health; evil spirits brought sickness and death. o Physician was medicine man who treated diseases by chanting, inspiring fear, or opening the skull to release evil spirits. Nurse was the mother who cared for her family during sickness by providing physical care and herbal remedies. [nurse as nurturing and caring] Temples became centers of medical care because of the belief that illnesses were caused by sin and gods displeasure. o Priests were regarded as physicians. o Nurse was viewed as slave, carrying out small tasks based on the orders of the priestphysician. Christian period nursing began to have a formal and clearly defined role. o Women called deaconesses made the first visits to sick people. o During Crusades (11th 13th) hospitals were built for the pilgrims needing healthcare and nursing became respectable. By end of Middle Ages nursing had developed purpose, direction, and leadership. Beg. Of 16th emphasis from religion to warfare, exploration, and expansion of knowledge. o There was a shortage of people. Women who had committed crimes were recruited into nursing to serve jail time. Nurses received low pay and worked long hours. Middle of 18th 19th - Nightingale: o Established training school for nurses o Identified needs of patient and roles of nurse to meet those needs. o Established standards for hospital management, occupation for women, nursing education o Recognized 2 parts of nursing: health and illness o Believed nursing as separate and distinct from medicine o Recognized nutrition is important to health o Stressed need for continuing ed. For nurses o Instituted occupational and recreational therapy for sick people o Maintained accurate records, recognized as the beginnings of nursing research 19th 21st : Battle casualties during Civil War focused attention on the need for educating nurses in the US. o Schools in connection with hospitals o Lead to lack of educational standards (no boundary between nursing service and nursing education), male dominance in healthcare, and idea that women depended on men WWII women worked outside of home o More independent and assertive o Lead to emphasis on education o War resulted in knowledge explosion in medicine and technology o Schools of nursing were based on educational objectives and were increasingly developed in university and college settings o Lead to degrees in nursing for men, women, and minorities Nursing broadened in all areas o practice in a wide variety of healthcare settings o Development of a specific body of knowledge
o o o
Conduct and publication of nursing research Recognition of the role of nursing in promoting health Increased emphasis on nursing knowledge as the base for EB has led to the growth of nursing as a professional discipline
Definitions of nursing Nurse: nutrix to nourish o Nursing: person who nourishes, fosters, and protects and who is prepared to take care of sick, injured, and aged people. International Council of Nurses (2002): Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups, and communities, sick or well and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled, and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. American Nurses Association (ANA): describes values and social responsibility for nursing, provides a definition and scope of practice for nursing, discusses nursings knowledge base, and describes the methods by which nursing is regulated within its Nursings Social Policy Statement o Nurses focus on human experiences and responses to birth, health, illness, and death within the context of individuals, families, groups, and communities. o Knowledge base for nursing practice includes diagnosis, interventions, and evaluation of outcomes from an establish plan of care. o Nurse integrates objective data with knowledge gained from an understanding of the patients or groups subjective experiences, applies scientific knowledge in the nursing process, and provides a caring relationship that facilitates health and healing. Focus in all definitions of nursing is patient and includes physical, emotional, social, and spiritual dimensions of that person. o Nursing concepts now include prevention of illness and promotion and maintenance of health for individuals, families, and communications. Status of nursing as a profession and as a discipline. Nursing uses existing and new knowledge to solve problems creatively and meet human needs within ever-changing boundaries. Nursing recognized as a profession: o Well-defined body of specific and unique knowledge o Strong service orientation o Recognized authority by a professional group o Code of ethics o Professional organization that sets standards o Ongoing research o Autonomy Nursing involves/is: o Specialized skills and application of knowledge based on an education that has both theory and clinical practice o Guided by standards set forth by professional organizations and an establish code of ethics o Focuses on human responses to health probs and is focused on wellness, an area of caring that includes nurses knowledge and abilities. o Recognized as scholarly, with academic qualifications, research, and publications. o Nursing interventions are focused on EBP
CHAPTER 5 Theory, Research, and Evidence-Based Practice Outline the steps in implementing evidence-based practice. Step 1. Ask a question about a clinical area of interest or an intervention: o Most common PICO: P Patient, population, or problem at interest (Need for explicit description; may include setting, limiting to subgroups such as age) I Intervention of interest (More defined, more focused search of literature will be; may include exposure, treatment, patient perception, diagnostic test or predicting factor) C Comparison of interest (usually to another treatment or standard of care) O Outcome of interest (Identifying outcome to enable a literature search to find evidence that examined the same outcome in different ways) Step 2. Collect the most relevant and best evidence. o Level of strength: 1 strongest and 7 lowest o Strongest evidence found from systematic reviews, EBP guidelines, and meta-analyis Systematic reviews: summarize finding from many studies of a specific clinical practice question or topic, and recommend practice changes and future directions for research. Evidence-based practice guidelines: synthesize info from multiple studies and recommend best practices to treat patients with a disease, a symptom or a disability Meta-analysis: uses statistical analysis of the effect of a specific intervention across multiple studies, providing stronger evidence than results from a single study. If these arent available, collect reviews of descriptive or qualitative studies or articles of original quantitative studies in databased from MEDLINE and CINAHL Step 3. Critically appraise the evidence o Ask 3 questions: What were the results of the study? Are the results valid (did the investigator measure what was intended to be measured) and reliable (were the measurements consistent across time) Will the results of the study improve patient care? Step 4. Integrate the evidence with clinical expertise, patient preferences, and values in making a decision to change. o If patient doesnt want change or if its too costly or risky, it shouldnt occur. X-rays allow one to see but are more riskier b/c of exposure to radiation. Step 5. Evaluate the practice decision or change. o Essential to determine if the change is effective for a particular patient or setting and if the expected outcomes resulted from the change. CHAPTER 6 Values, Ethics, and Advocacy Compare and contrast the principle-based and care-based approaches to bioethics. Principle based approach includes: Utilitarian (rightness or wrongness of an action depends on the consequences of the action) Deontologic (action is right or wrong independent of its consequences) o It identifies 4 key principles:
Autonomy - respect the rights of patients or their surrogates to make healthcare decisions (provide info to patients and families to make the decision that is right for them; might need to collaborate with other professionals) Nonmaleficience - avoid causing harm (seek not to inflict harm; seek to prevent harm or risk of harm whenever possible) Beneficence benefit the patient, and balance benefits against risks and harms (commit yourself to actively promote the patients benefit (health and wellbeing or good dying) Justice give each his or her due; act fairly (always seek to distribute the benefits, risks, and costs justly) o Many nurses add fidelity - keep promises (never abandon a patient), veracity (truthfulness), accountability (responsible), privacy, and confidentiality. Be aware: people identify benefits and harms differently o Ethical dilemmas arise when an attempt to adhere to basic ethical principles results in two conflicting courses of action. No way to identify which is most important. There are 2 or more correct courses of action where both cannot be followed You are doing something right and something wrong Most involve ethical conduct or conflicting traits of character
Care based approach care as foundation for nursings ethnical obligations. Directs attention to the specific situations of individual patients viewed within the context of their life narrative. o How you chose to be and act each time you encounter a patient or colleague is a matter of ethnical significance. Characteristics: o Centrality of the caring relationship o Promotion of the dignity and respect of patients as people o Attention to the particulars of individual patients o Cultivations of responsiveness to others and professional responsibility o Redefinition of fundamental moral skills to include kindness, attentiveness, empathy, compassion, and reliability. Use an ethical framework and decision-making process to resolve ethical problems. Ethnical distress: nurse knows right thing to do but either personal or institutional factors make if difficult to follow the correct course of action. There is a barrier keeping you from doing something thats right There is a barrier because something is wrong, but you are not sure what it is Use nursing process: o 1. Assess the situation (gather data): Involves the people involved, overall nursing, medical, and social situation, and relevant legal, administrative, and staff considerations. o 2. Diagnose (identify) the ethical problem: Clarify that the issue is ethical is there a conflict at the personal, interpersonal, institutional, or societal level? Is there a question that arises either at the level of thought or feeling? Does the question have a moral or ethical component (does it raise issues of rights or moral character?)?
State problem, identify your relationship to the decision. Identify time parameters. o 3. Plan: identify options and short/long term consequences: Use ethical reasoning to decide on a course of action that you can justify equally. Identify your personal and professional moral positions and those of other involved individuals. Apply pertinent ethical theories and principles. Apply codes of conduct and ethics, professional position statements or guides as applicable. Consider consultation with a respected and wise colleague or an institutional ethics committee. Decide on the course of action you are best able to support. o 4. Implement your decision: And compare your action outcome with what you considered and hoped for in advance. o 5. Evaluate your decision: What have you learned from this process that will help you in the future? How can you improve your reasoning and decision making in the future? In what ways does your institutional culture need to chance to prevent similar conflicts in the future? 8 ethical considerations in patient care: o Balance between benefits and harms in the care of patients o Disclosure, informed consent, and shared decision making 3 models Paternalistic: clinicians act to benefit the patient and decide what should be done and inform the patient and patient has to comply Patient sovereignty: patients or their surrogates express their right to be autonomous, tell the clinican what they want, and clinicians role is to comply. Most clinicians believe in shared decision making. Objective for all clinical decision making is decisions that secure the health and well being of the patient and that honor and respect the integrity of all participants in the decision making process. o Norms of family life Sensitivity of how a patients injury or illness influences family members Relationship between clinicians and patients o Professional integrity of clinicians While patient is main focus, nurses owe integrity to other professionals sacrificing personal integrity to meet the needs of others. o Cost-effectiveness and allocation Needs of patients and their families and the limited resources available to professional caregivers. Justice distributes benefits and burdens of healthcare delivery fairly. o Issue of cultural and/or religious variation Conflicts among religions o Considerations of power Clinicians who believe that they lack power to influence care settings and delivery may also experience ethical conflict and distress Examples of ethical problems/dilemmas
o Examples of o
o Examples of o o
Paternalism Does preventing harm justify violating the patients right to autonomy and make it acceptable for the nurse to act as a parent and choose an action the patient doesnt want b/c the nurse believes it to be in the patients best interest? Deception New student in order to decrease patients anxiety, should student say, no Ive given this before? Confidentiality If the nurse believes anxiety is interfering with the patients ability to obtain needed healthcare, would it be ethical to break the womans confidence to obtain help for her? Allocation of scare nursing resources You know you cannot meet everyones needs well; how do you distribute your nursing care? Advocacy in marker-driven environment Woman has to be discharged but you know she would be better off staying b/c no family but she has no money to pay for more days What do you do? Valid consent or refusal Should you administer the medication knowing the patient no longer consents to this procedure? Conflicts between the patients and nurses interests Homeless man nurse pregnant is a nurse ever justified in refusing to provide care to a patient assigned to his or her care? Conflicts concerning new technologies In vitro fertilization physician/nurse problems Disagreements about the proposed medical regimen Patient wants to die and doesnt want to go through tests but dr. tells you to do it do you prepare the patient for the tests? Are there grounds to refuse participation? Conflicts regarding the scope of the nurses role Even if dr. says no is nurse obligated to make a recommendation for the patient? Unprofessional, incompetent, unethical, or illegal physician practice Is the nurse obligated to report the slacking physician? nurse/nurse problems Claims of loyalty Patient dies while nurse is sleeping; do you report it? Unprofessional, incompetent, unethical or illegal nurse practice Patient reported nurse touching her inappropriately what should you do?
CHAPTER 21 Communicator List at least eight ways in which people communicate nonverbally o Aka body language helps nurse to understand subtle and hidden meanings in what is being said verbally. Touch o Means different things for different people based on family, religion, class o One of the most effective nonverbal ways to express feelings of comfort, love, affection, security Eye contact
Glance attention-getting method to open convo Some cultures respect & willingness to listen while others as invasion to privacy or inferiority o Eyes fix in a stare = anger, narrow = disgust, open wide = fear o Blank stare = daydreaming Facial expressions o Most expressive part of the body Posture o People in good health hold their bodies well; depressed = slouch; rigid, stiff = tension/pain Gait o Bouncy, purposeful walk carries a message of well-being o Shuffling = sad/discouraged; bent over = recovery from surgery Gestures o Thumps up = victory, kicking an object = anger, waving = come over o Used when two people speaking in different languages attempt to communicate with each other General physical appearance o Dry skin = dehydration; radiate = good health Mode of dress and grooming o Dress well = high self-esteem Sounds o Crying, moaning, gasping, sighing Silence o Complete understanding of each other, thinking, or angry with each other o o
Describe the interrelation between communication and the nursing process Assessing o Gather info from verbal & nonverbal communication forms o Written word used to obtain data concerning patients and when reading a patients records or charts before meeting them o Spoke word give and receive reports to and from other health providers o Data collected verbally and nonverbally is analyzed to others through oral and written communication Diagnosing o Communicate with other nurses through writing and word o Written diagnosis becomes permanent part of patients record o Outcome identification and planning o Planning requires communication among patient, nurse, and others as outcomes are developed and interventions are determined o Need to inform others on what needs to be done Implementing o Teach, counsel, and support patients/families o Nursing order requires many messages between nurse and patient Evaluating o Rely on verbal and nonverbal cues from patient to see whether objectives or goals have been achieved o Negative messages facilitates revision of parts of the care plan Documenting communication o Assessment of patients needs and conditions requires accurate documentation.
Describe how each type of ineffective communication hinders communication Failure to perceive patient as human being o Address patient by formal name Mr. Mrs. Dr. vs slang honey, sweetie o Focus on whole person not simply on illness Failure to listen o Closed mind or focusing on own needs o Nurses who lack confidence may become defensive o Defensiveness = barrier to open and trusting communication Inappropriate comments or questions Cliches o Clich sterotypes, trite, or pat answer everything will be all right. o Generalizations men tolerate pain poorly. Using questions requiring only yes or no answer o Did you have a good day? o Are you ready to get out of bed? Using questions containing the words why and how o Why were you not tired? How did you ever go on a crash diet? o Seem intimidating Using questions that probe for information o May become resentful, stop talking, and try to avoid further conversation o lets get to the bottom of this Using leading questions o Produce answers that might please the nurse but are unlikely to encourage the patient to respond honestly without feelings intimidated o You arent going to smoke that are you? Using comments that give advice o Implies that the nurse knows what is best for the patient and denies him or her the right to make decisions and have feelings. o Increases patients dependence on caregivers. o Can be good when requested and if nurse is an expert Using judgmental comments o You arent acting very grown up. Changing the subject o Patient may be ready to discuss something and can be frustrated if put off by a change in topic o Nurse may feel uncomfortable and change subject (death, suicide, abortion) ex. of ignoring the patient and worrying about own needs Giving false assurance o Impression that nurse isnt interested in their problems Gossip and rumor o Can be used to inform, influence others, entertain, or vent o Can damage reps of individuals who are the subject of the info Aggressive interpersonal behavior o With physicians, horizontal violence nurse to nurse o Angry patients remain with patient, be calm/assertive, restraints as a last resort CHAPTER 24 Vital Signs Identify sites for assessing temperature, pulse, and blood pressure, assess temperature, pulse, respirations, and blood pressure accurately, and demonstrate knowledge of the normal ranges for temperature, pulse, respirations, and blood pressure across the lifespan Temperature
o o
o o
Factors affecting site are age, state of consciousness, amount of pain Tympanic membrane: core temp Should not be used with patient who has drainage from ear or scars Oral Patient must close mouth around probe If patient drank hot or cold fluids or smoked or chewed gum, wait 15-30 minutes to allow oral tissue to return to normal temp. Should not be taken in people with diseases of oral cavity and those who had surgery in nose and mouth or in person with O2 (can drop). Rectal: core temp When oral cannot be used Not used in newborns, children with diarrhea Stimulates vagus nerve decreases BP Cant use with person low WBC or spinal cord injury Axillary Newborns Normal temps: >98.6 F = pyrexia (fever) Older adults at risk for an extreme; lose body temp Infants & children respond more to changes in body temp Steps to assess temp: Hand hygiene & PPE Identify patient Close curtains around bed privacy and discuss procedure Make sure thermometer is working Put on gloves it dealing with body fluid Tympanic: turn on, put disposable probe, insert in ear towards jawline, pull pinna up and back to straighten ear canal, then activate (2 sec) Oral: place probe under patients tongue in posterior sublingual pocket in contact with blood vessels lying close to surface Rectal: adjust bed to elbow of caregiver, side-lying position, expose only buttocks, lubricate probe 1 inch with water-soluble lubricant, insert in anus 1.5 in. in adult & 1 in. in child, use toilet tissue to remove feces, place bed in lowest position Axillary: place end of probe in center of axilla and bring arm down close to body Temporal artery: like a remote, press on and hold, and spread through forehead, midline, hairline NORMAL TEMPERATURES IN ADULTS RECTAL AXILLARY TYMPANIC 99.5 F 97.7 F 99.5 F 37.5 C 36.5 C 37.5 C FOREHEAD 94.0 F 34.4 C
ORAL 98.6 F 37.0 C Pulse o
Peripheral arterial pulses Temporal, carotid, brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis Radial most common
Carotid emergency people in shock or cardiac arrest Brachial infants Apical pulse If peripheral is weak, irregular, very rapid Assessed when giving meds that alter heart rate or rhythm 5th and 6th intercoastal space, 3inc left of the median line and slightly below nipple Apical-radial pulse When radial pulse irregular, count pulse at apex and radial artery together Difference between the rates pulse deficit indicates that all of the heart beats are not reaching the peripheral arteries or are too weak to be palpated Normal rates: Adults/adolescents 60-100 beats/min Decrease w/ age Assessing peripheral pulse by palpitation Check medical order Perform hygiene Identify patient Close curtains and explain procedure Lightly compress artery so pulsations can be felt and counted If normal, count 30 sec and multiply by 2; if abnormal count whole min Note rhythm & amplitude (+2 normal)
Respirations o Involves ventilation, diffusion, and perfusion Ventilation (breathing)- movement of gases in and out of lungs Ventilation has both autonomic and voluntary control Inspiration (inhalation) act of breathing in Expiration (exhalation) act of breathing out Diffusion exchange of oxygen and carbon dioxide between the alveoli of the lungs and the circulation blood Perfusion exchange of oxygen and carbon dioxide between the circulating blood and tissue cells o Assess respiratory rate (breaths/min), depth (deep or shallow), and rhythm (regular or irregular) by inspection (observing and listening) or by listening with stethoscope Can also monitor arterial blood gas results and pulse oximeter to determine oxygenation of blood o Normal respirations: Adults 12-20/min Infants/young children breathe more rapidly o Assessing respiration while fingers on pulse measurement, count respirations for 30 sec and x2 for respiratory rate/min Blood pressure o Force of the moving blood against arterial walls Max BP when exerted on the walls of the arteries when the LV of the heart contracts & pushes blood thru aortic valve into the aorta at the beginning of systole Pressure rises as ventricle contracts (systole) and falls as heart relaxes (diastole)
Assessing blood pressure Sphyhmomanometer Cuff & manometer Bladder inside cuff should enclose at least 2/3 of the adult limb and all of a childs limb If cuff too narrow = too high reading If cuff too wide = too low reading Length should be 80% of arm circumference and width 40% of arm circumference Bladder inflated enough to obstruct flow of blood through artery & needle valve allows cuff to be deflated while pressure is being read Automated blood pressure monitors May have PR, puse oximetry, or temp Doppler ultrasound Amplifies sound Used if sounds are indistinct or inaudible Direct electronic measurement Insert thin catheter into artery; tip senses pressure and transmits it to display waves of systolic and diastolic Used in intensive care Assessing brachial artery BP Should not be taken on arm with IV line or AV fistula or shunt Should be avoided in the arm on the side of an axillary node dissection Assessing politeal artery BP Systolic = normally 10-40 mm Hg higher; diastolic same Prone position Palpatiing the BP Cuff inflated 30 mm Hg above point at which artery disappears Normal BP 120/80 Rise or fall of 20-30 mm Hg is significant Older people higher BP Lowest in the am Women lower BP until menopause BP incr. with food, exercise, contraceptives, emotions, weight, and when sitting (as compared to lying) Assessing BP Forearm should be supported at level of heart and palm of hang upward Palpate brachial artery center bladder of cuff over brachial artery, about midway on the arm, so that the lower edge of the cuff is about 2.5 5 cm (1-2 in.) above inner aspect of the elbow Line artery marking on the cuff up with the patients brachial artery Wrap cuff around arm smoothly and snugly, dont allow any clothing to interfere with proper placement of cuff Palpate radial artery, inflate cuff and note when pulse disappears Pump pressure 30 mm HG above systolic Note when first faint, but clear sound appears that slowly increase in intensity systolic Note when sound completely disappears - diastolic
AGE Newborn 1 3 yrs 6 8 yrs 10 yr Teens Adults >70 yrs
AGE-RELATED VARIATIONS IN NORMAL VITAL SIGNS TEMPERATURE (F) PULSE (BEATS/MIN) RESPIRATIONS (BREATHS/MIN) 36.8 (axillary) 80 180 30 80 37.7 (rectal) 80 140 20 40 37 (oral) 75 120 15 25 37 (oral) 75 110 15 25 37 (oral) 60 100 15 20 37 (oral) 60 100 12 20 36 (oral) 60 100 15 20
BLOOD PRESSURE (MM HG) 73/55 90/55 95/75 102/62 102/80 120/80 120/80
CHAPTER 27 Asepsis and Infection Control Explain the infection cycle
Infection - disease state that results from the presence of pathogens (disease-producing microorganisms) Infectious agent o Bacteria most significant and most commonly observed infection-causing agents Sperical (cocci), rod-shaped (bacilli), or corkscrew shaped (spirochetes) Gram + : thick cell wall that resists decolorization and are stained violet Gram - : decolorized by alcohol & do not stain o Virus smallest of all organisms, seen only in EM Given antiviral meds during prodromal stage to shorten full stage of the illness o Fungi plant-like & present in air, soil, water Organisms ability to produced disease in a person depends on: o Number of organisms o Virulence of organism, or its ability to cause disease o Competence of the persons immune system o Length and intimacy of the contact between the person and the microorganism Reservoir o Growth and multiplication of microorganism o Is natural habitat of the organism o People, animals, soil, food, water, milk, other people Portal of exit o Point of escape for organism from reservoir o Respiratory, gastrointestinal and genitourinary tracts, blood tissues, and breaks in skin Means of transmission o Direct or indirect, vectors, airborne, and droplets Portal of entry o Organism enters new host; usually same as entrance Susceptible host o Microorganisms can continue to exist only in a source that is acceptable host and only if they overcome any resistance by the hosts defenses o Susceptibility degree of resistance the potential host has to be the pathogen
Describe nursing interventions used to break the chain of infection Assessing o Early detection and surveillance techniques o Ask about patients immunizations and previous/recurring infections o Observe signs/symptoms of a local or system infection o Lab results Diagnosing o Nursing dx : Risk for Infection related to Impaired ... related to o Reflects patients condition Outcome identification and planning o Review assessment data, cycle of events leading to infection, and incorporate principles of infection control o Plan outcomes that prevent infection o Good hand hygiene, identify signs of infection, nutritional intake, disposal of soiled articles, disinfect, reduce stress Implementing o Asepsis all activites to prevent infection or break the chain of infection o Medical asepsis clean technique involves procedures and practices that reduce the number and transfer of pathogens Hang hygiene & wearing gloves o Surgical asepsis sterile technique, includes practices used to render and keep objects and areas free from microorganisms Insert indwelling urinary catheter, or IV catheter Medical asepsis o Contaminated if they bear or are suspected of bearing pathogens o Hand hygiene most effective way to help prevent spread of infectious agents Hand washing with plain soap and water, use of antiseptic hand rubs (waterless alcohol based products or surgical hand antisepsis) Clean hands when they are soiled, after each contact with contaiminated materials, and after removing gloves Use alcohol base rubs before and after direct contact with patients, gloves, before invasive devices that do not require surgical placement, and contact with objects Rub 15 sec or until dry Wash hands 1 inch above area of contamination Sterilizing and disinfecting o Disinfection destroys all pathogenic organisms except spores Used when preparing skin for a procedure or cleaning a piece of equipment that does not enter a sterile body part o Sterilization destroys all microorganisms, including spores On equipment that is entering a sterile portion of the body Techniques to clean equipment o Wear waterproof gloves o Rinse articles with cold water first o Wash articles with warm water that has detergent or soap o Use a brush with stiff bristles to clean thoroughly o Rinse and dry article o Prepare cleansed equipment for sterilization or disinfection o Discard gloves, brush PPE personal protective equipment: gloves, gowns, masks, and eye gear
Gloves contact with fluid Gowns patients blood and body fluids o Masks prevent wearer from inhaling large particle aerosols High-efficiency particulate air HEPA filter respirator or N95 respirator certified by NIOSH must be worn when entering a room of a patient with known or suspected TB They filter inspired air o Eyewear Goggles or face shield worn when risk of contaminating mucous membranes of the eyes Suctioning a tracheostamy or assisting with invasive procedure that results in splattering of blood or other body fluids requires protection for the caregiver Surgical asepsis o Used in OR, labor, delivery areas, and diagnostic testing o Insert urinary catheter, sterile dressing changes, or preparing injectable medication o Areas are contaminated if they are touched by an object that is not sterile o Most solutions are unsterile after 24 hrs after theyre opened o Grasp bottle so label is on palm of your hand prevents any liquid froom running over the label and making it illegible o Sterile drape o
o
List the stages of an infection Incubation period o Interval between the pathogens invasion of the body and the appearance of symptoms of infection o Organisms are growing and multiplying Prodromal stage o Person is most infectious here o Early signs and symptoms of disease are present, but these are often vague and nonspecific, ranging from fatigue and malaise to a low-grade fever o Patient does not realize that he or she is contagious Full stage of illness o Presence of specific signs and symptoms indicates full stage of illness o Type of infection determines length of illness and severity of the manifestations o Systemic or local symptoms Convalescent period o Recovery period from infection o Signs/symptoms disappear and person returns to healthy state Identify factors that reduce the incidence of healthcare-associated infection Instituting constant surveillance by infection-control committeees and nurse epidemiologists o Their work can reduce infections when aggressive control measures are initiated based on their findings Having written infection-prevention practices for all agency personnel o Adhere to hand hygiene recommendations and infection-control precaution techniques can prevent HAI Use practices to promote and keep patients in the best physical condition o Measures include meeting the patients needs for nutrition, fluids, rest, oxygen, and physical and psychological comfort and security. Staffing
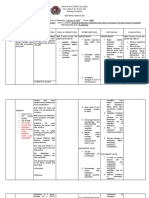
Identify situations in which hand hygiene is indicated (see above) Describe strategies for implementing CDC guidelines for standard and transmission-based precautions when caring for patients Standard precautions o Used in the care of all hospitalized individuals regardless of their diagnosis or possible infection status o Apply to blood, all body fluids, secretions, and excretions except sweat (whether or not blood is present or visible), nonintact skin, and mucous membranes o Respiratory hygiene/cough etiquette, safe injection practices, and directions to use a mask when performing high-risk procedures involving spinal cord punctures o Clean nonsterile gloves, PPE, cough on tissue, 3 foot separation, dont recap needles (needlestick), safe injection single dose vials, face mask Transmission-based precautions o Used in addition to standard precautions for patients in hospitals with suspected infection with pathogens that can be transmitted by airborne, droplet, or contact routes TRANSMISSION BASED PRECAUTIONS AIRBORNE DROPLET TB, chicken pox, measles, Rubella, mumps, diphtheria SARS Private room, door may be Private room, keep door open closed and patient in room PPE upon entry into room for Monitored negative air all interactions pressure in relation to Transport patient out of surrounding areas, 6-12 air room only when necessary changes/hr, and appropriate and place surgical mask on d/c of air outside or patient monitored filtration if air is Keep visitors 3 feet from recirculated infected person Wear mask or respiratory when entering room unless immune to disease Transport patient out only if necessary and place surgical mask on patient
CONTACT MDRO Private room PPE whenever you enter room Change gloves after contact with infective material Remove PPE before leaving patient environment and wash hands with antimicrobial or waterless antiseptic agent Limit movement of patient out of room Avoid sharing patient-care equipment
Implement recommended techniques for medical and surgical asepsis (see above) CHAPTER 31 Hygiene Assess the condition of the patients skin, oral cavity, hair, and nails using appropriate interview and physical assessment skills Assessing/interviewing o Daily/weekly bathing habits Skin o Rashes, lumps, itching, dryness, lesions o How long have you had this problem? Does it bother you? How does it bother you?
o Document patients typical hygiene practices and any complaints (use of creams, soaps) Oral cavity o History of teeth, tongue, salivary glands o Identify variables that cause oral problems deficient self-care, poor nutrition, or excess of sugars, family history Eyes, ears, nose o Glasses, contacts, hearing aids Hair o Texture, amount of hair, treatments, malnutrition Nails & feet o Type of footwear worn, foot problems, history of biting nails o Perineal and vaginal areas o Foley cath, childbirth, surgery, UTI, diabetes Physical assessment Skin o Cleanliness, color, texture, temperature, turgor, moisture, sensation, lesions o Lesion type, color, size, distribution & grouping, location, and consistency o Dry skin, acne, rashes Oral cavity o Odors o Lips: color, moisture, lumps, ulcers, lesions, edema o Buccal mucosa: color, moisture, lesions, nodules, bleeding Color of gums and surface of gums: lesions, bleeding, edema, exudates o Teeth: loose, missing, decayed teeth; dentures or other orthodontic devices o Tongue: color, symmetry, movement, texture, lesions o Hard and soft palates: intactness, color, patches, lesions o Oropharynx: movement of uvula and condition of tonsils if present o Caries: decay of teeth wit the formation of cavities o Plaque: invisible, destructive, bacterial film that builds up and leads to destruction of tooth enamel o Gingivitis: inflammation of gingival, the tissue surrounding the teeth o Periodontitis: inflammation of gums that also involves degeneration of the dental periosteum (tissues) and bone o Halitosis: strong mouth odor Eyes, ears, and nose o Check position, alignment, and appearance of eye Check eyelashes are equally distributed and curl outward Note lesions nodules, redness, swelling, crusting, flaking, tearing or discharge of eyelids Check color of conjunctiva and test blink reflex o Ear: position, alighment and appearance Buildup of wax in canal, dryness, crusting, or presence of any d/c or foreign body o Nose: position and appearance, nostrils, check tenderness, dryness, edema, bleeding, discharge or secretions Hair o Texture, cleanliness, and oiliness o Scaling, lesions, infections on scalp o Dandruff, hair loss, infestations o Pediculosis: infestation with lice Nails and feet
o o
Observe nail base for redness, swelling, bleeding, d/c, tenderness Cleanliness and intactness
Describe the priorities of scheduled hygiene care Early morning o After patient wakes up, assist with toileting o Prepare for breakfast or diagnostic tests o Wash face, hands, and mouth care Morning care (AM care) o After breakfast, assist with oral care, bathing, back massage, skin care measures (pressure ulcers), hair care (shaving), cosmetics, dressing, and positioning for comfort Afternoon care (PM care) o Toileting, handwashing, oral care o Straighten bed linens Hour of sleep care (HS care) o Change any soiled linens As needed care (PRN care) o Oral care every 2 hours o Change bed linens if soiled Demonstrate techniques for assisting patients with hygiene measures, including those used when administering various types of baths and those used in cleaning each part of the body. (also oral care unconscious patient) Shower & tub baths o Shower preferred method in patients who can move o Gather soap, washcloth, towel, gown o Provide place to sit stool or chair o Temperature 110F 115F o Lower temp for kids and older people o Keep door unlocked o Bed baths o Use emollient agents moisturizes which can be applies as location, cream, gel, or ointment They seal water into skin and replace lipids in skin, hydrating skin and recreating waterproof barrier Backrubs 4-6 minutes Keep oral mouth moist 1-2 hours CHAPTER 32 Skin Integrity and Wound Care 1. Discuss the processes involved in wound healing Hemostasis o Immediately after tissue injury o Involved blood vessels constrict and blood clotting begins through platelet activation and clustering o These same blood vessels then dilate and capillary permeability increases, allowing plasma and blood parts to leak out into the area that is injured, forming a liquid exudates o Accumulation of exudates leads to swelling and pain o Increased perfusion results in heat and redness o If wound is small, clot loses fluid and a hard scab is formed to protect the injury o Platelets release substances that stimulate other cells to migrate to the injury Inflammatory phase
Lasts 4-6 days WBC, leukocytes, and macrophages move to the wound o Leukocytes arrive 1st to ingest bacteria and cellular debris o 24 hrs after injury, macrophages enter wound area and remain o They release growth factors that attract fibroblasts that help to fill wound Proliferation phase o Aka fibroblastic, regenerative, or connective tissue phase o Lasts several weeks o New tissue built to fill wound space, mainly through action of fibroblasts o Fibroblasts are CT cells that synthesize & secret collagen, produced GF responsible for inducing BV formation & incr. # and movement of endothelial cells o Capillaries grow around wound bring O2 & nutrients o Fibrin clot o Granulation tissue forms scar tissue Maturation phase o 3 weeks after injury o Collagen remodeled to become stronger scar tissue o o
2. Identify factors that affect wound healing Pressure o Interferes with blood flow & tissue and delays healing Desiccation o Process of drying up o Cells dehydrate & die in dry environment o causes crust to form o Moist wounds = enhanced epithelial cell migration Maceration o Overhydration urinary & fecal incontinence impaired skin integrity o Trauma o Edema o Insufficient O2 and nutrients to tissue Infection o Bacteria inc. stress requires inc. energy to deal with invaders o Toxins released when bacteria die interfere with wound healing & cause cell death Necrosis o Death of tissue slough, moist, yellow stringy tissue o Eschar dry, black, leathery Age o Small infants & children at increase o Older adults longer to heal Circulation & oxygenation o Need enough of it to remove toxins & bacteria o Fat people delay healing Nutritional status o Vit A & C epithelization and collagen synthesis o Zinc proliferation of cells Wound condition o Large contaminated infected wounds or wounds with foreign bodies heal slowly Medications and health status
Corticosteroid drugs (dec. inflam process) & postop radation therapy (depress bone marrow dec. WBC) delay healing o Chemotherapy impair proliferation of growing cells o ABT secondary infection & superinfection Immunosupression o AIDS, lupus
o
Identify patients at risk for pressure ulcer development Immobility o Long time in bed or seated without shifting body weight o Unconscious, paralyzed, cognitive impairment, fractures and others who remain in 1 position for a long time o Emotionally depressed Nutrition and hydration o Protein & calorie malnutrition o Leads to neg N2 balance, electrolyte imbalance & skin injury Moisture o Reduces resistance to trauma o Urinary & fecal incontinence incr. risk for skin damage due to chem.. irritation from ammonia in urine Mental status o Apathy, confused, and comatose state dec. Age o Older people Describe the method of staging of pressure ulcers Blanching (pale/white) of skin under pressure ulcer Ischemia makes skin look paler Hyperemia reddening of skin when pressure removed o Body floods area w/ blood to nourish & remove wastes from cells o Area appears red & feels warm but blanches when slight pressure applied o Circulation impaired & pressure ulcer develops o Deep-tissue injury purple/maroon localized area or blood-filled blister Stage I pressure ulcer = intact skin w/ nonblanchable redness of a localized area usually over a bony prominence Stage II partial thickness loss of dermis Stage III ulcer with full thickness tissue loss o Subcutaneous fat may be visible o Undermining and tunneling Stage IV full thickness tissue loss w/ exposed bone, tendon, muscle o Slough or eschar may be present & undermining/tunneling o Unstageable o Base of ulcer covered by slough (yellow, tan, gray, green, or brown) or eschar (tan, brown, black) in wound bed o Eschar thick leathery scab or dry crust that is necrotis Stable (dry, intact) eschar on heel serves as bodys natural biological cover & cant be removed 5. Accurately assess and document the condition of wounds Skin assessment o Acute care setting: every 48 hrs; stable patients in icu are daily; unstable every shift
Long-term care setting: every 48 hrs 1st week, weekly 1st month, then monthly quarterly o Home healthcare: every visit Risk assessment (scale w/ qs Braden scale) o Assess mobility, nutritional status, moisture, & incontinence o Moisture makes skin more susceptible to injury o Microorganisms can multiply Wound assessment o Appearance o Document size (L x W x D) o Edges (meet), dehiscence, or evisceraton o Type of tissue in wound granulation, slough, eschar Drainage serous (clear, watery), sanguine (bloody), serosanguine (serums & RBC; light pink to blood tinged), purulent (WBC, yellow, green) Assess pain
o
Provide nursing interventions to prevent pressure ulcers. Reposition pt every 2 hrs Oblique best as alt. to side lying Use pillows, foam wedges under calves raises heels Avoid massage over boney area Air, gel, water mattresses
Apply hot and cold therapy effectively and safely Heat o Hot water bags may leak or burn o Electronic heating pads electric shock, dont place under pt o Aquathermia pads (Aqua K) help with back pain, muscle spasms, inflammation o Hot packs o Warm moist compressors promote circulation, healing, and dec. edema o Sitz bath inc. vasodilation, relaxation Warm soaks inc. blood supply, aid in cleaning wounds like burns, improve circulation, apply medication Sterile technique if on large wound 15-20 min/soak Cold o Ice bags 30 min o Cold packs o Cold moist compressors used for injured eye, headache, tooth extraction 30 min; change 2-3 hrs CHAPTER 35 Comfort Describe specific elements in the pain experience Transduction
Conversion of painful stimuli into electrical impulses that travel from periphery to spinal cord at dorsal horn o Nociceptors peripheral nerve fibers that transmit pain o Damaged cell releases histamine, which excited nerve endings o Lactic acid accumulates in tissues injured by lack of blood supply & is believed to excite/activate nerve endings & cause pain o Bradykinin vasodilator; incr. capillary permeability & constricts smooth muscle; triggers release of histamine & produces redness, swelling, & pain when inflammation is present o Prostaglandins hormone-like that send additional pain stimuli to CNS o Substance P sensitizes receptors on nerves to feel pain & also inc. rate of firing of nerves Transmission of pain stimuli o Pain from site of injury or inflammation are conducted along pathways to spinal cord & to higher centers transmission o Free nerve ending pain receptors incl. afferent (fibers carrying impulses from pain receptors to brain), fast conducting A delta fibers (acute, well-localized pain) and slow-conducting C fibers (diffuse, visceral pain burning & aching) o Protective pain reflex Sensory impulses travel over A fibers through dorsal root ganglion to dorsal horn of spinal cord Sensory nerve impulse synapse with a motor neuron & impulse is carried along efferent nerve pathways back to the site of the painful stimulus in a reflex arc results in immediate muscle contraction that removes injured part from source of the pain Perception of pain o Sensory process that occurs when stimulus for pain is present o Persons interpretation of pain o Pain threshold lowest intensity of stimulus that causes subject to recognize pain Modulation of pain o Sensation is inhibited or modified by neuromodulators (endogenous, opioid compounds [naturally presenting] morphine-like chemical regulators in the spinal cord & brain) o Endorphins - @ neural synapses @ various points along CNS Powerful blocking chemicals that have prolonged analgesic effects & produce euphoria Pain sensation & relief o 1) Pains path begins as a message & is received by nerve endings in a burned finger substance P, bradykinin, prostaglandins r released, sensitizing nerve endings, helping to transmit pain message from injured finger toward brain, & settings stage for healing (inflammatory response) 2) pain signal from burned finger travels as an electrochemical impulse along length of nerve to the dorsal horn on the spinal cord, a region that runs the length of the spine & received signals from all over body 3) message is relayed to thalamus, a sensory center in the brain where sensations such as heat, cold, pain, and touch first become conscious 4) it then travels on to the cortex where the intensity & location of pain are perceived 5) pain relief begins as a signal from the brain & descends by way of spinal cord 6) in dorsal horn, chemicals such as endorphins are released to diminish the pain message from the injured finger
o
Compare and contrast acute and chronic pain ACUTE PAIN Rapid in onset, varies in intensity from mild CHRONIC PAIN Lasts beyond normal healing period
to severe Protective in nature; warns individual of tissue damage or organic disease
3-6 months Remission no symptoms present Exacerbation - symptoms reappear Often perceived meaningless and leads to withdrawal, depression, anger Poorly localized
Identify factors that may affect an individuals pain experience Culture o Patients in pain may be calm, objective, and uncomplaining approach to pain o Be aware of pain tolerance, expressions of pain, and alternative practices used to manage pain Ethnic variables o Jewish and Italian men tend to be more vocal and outwardly emotional w/ their experiences of pain o Difficult to anticipate individual responses to pain b/c nowadays are mixed Family, gender, and age variables o Spouses may reinforce pain o Children in diff families may be brave o Women verbalize more o Young kids express more pain than older adults these adults accept it as a daily norm Religious beliefs o Pain & suffering as a lack of goodness o Way of purification Environment and support people o Lights, noise, lack of sleep can influence pain o Presence of loved family member is essential to sense of well-being & may decr. Pain Anxiety & other stressors o People who were taught preop what to expect postop did not require as much medication for pain as those who did not receive this teaching Past pain experience o People who dont know severe pain have no fear of it o People who received immediate relief dont fear it o People who experienced extreme pain tend to anticipate more pain o Painful memories may provoke a violent response Administer analgesic agents safely to produce the desired level of analgesia without causing undesirable side effects Analgesic pharmaceutical agent that relieves pain o Reduce persons perception of pain & to alter persons responses to discomfort o If patient sleeps, give naloxone o When respiratory rate > 9 breaths/min can resume Physical dependence body physiologically becomes accustomed to opioid & suffers withdrawal symptoms if opioid is removed or dose is rapidly decr. Tolerance body becomes accustomed to opioid & needs larger dose each time for pain relief Addiction compulsive opioid use for means other than pain control Craving for substance, compulsive use, lack of control over drug, and continued use despite harm OPIOID ANALGESICS MODERATE SEVERE PAIN NONOPIOID ANALGESICS ACETAMINOPHEN & NSAIDS
RELIEVE PAIN OF EVERY TYPE BIND TO RECEPTORS IN BRAIN MORPHINE SIDE EFFECTS: SEDATION, NAUSEA, CONSTIPATION DEPRESSION 1 = AWAKE & ALERT; NO ACTION NECESSARY 2 OCCASSIONALLY DROWSY BUT EASY TO AROUNE; REQUIRES NO ACTION 3 FREQUENTLY DROWSY & DRIFTS OFF TO SLEEP DURING CONVERSATION; DECR. OPIOID DOSE 4 SOMNOLENT W/ MIN OR NO RESPONSE TO STIMULI; D/C OPIOID & CONSIDER USE OF NALOXONE (ANTAGONIST) CONSIDER: PATIENTS PAIN RATING, SEDATION LEVEL, COMFORT-FUNCTION GOAL (ALLOWS PATIENT TO DO ACTIVITY)
MILD-MODERATE OVER THE COUNTER & PRESCRIBED NSAIDS ANTIIFLAMMATORY POTENTIAL FOR GASTRIC BLEED COX -2 INHBITORS LOWER RISK OF GI BLEED LOW DOSES FOR SHORT PERIODS OF TIME
ADJUVANT DRUGS ENHANCE EFFECTS OF OPIOIDS BY PROVIDING ADDITIONAL PAIN RELIEF REDUCE SIDE EFFECTS FROM PRESCRIBED OPIOIDS OR LESSEN ANXIETY ABOUT PAIN EXPERIENCE
Applying analgesic o Review pain scale of choice o Discuss benefits of pain scale o Try pain control measures o Use pain control measures before pain increases in severity o Ask patient whats been proven effective in the past o Select and modify pain control measures based on patients respons o Encourage patient to try pain treatment several times before labeling it ineffective o Be open-minded about alt. pain relief o Be persistent o Be safe
CHAPTER 39 Oxygenation Describe the principles of respiratory physiology (medulla) Pulmonary ventilation (breathing) movement of air into and out of the lungs o Inspiration (inhalation) active phase movement of muscles & the thorax to bring air into lungs o Expiration (exhalation) passive phase movement of air out of the lungs o Inspiration Diaphragm contracts & descends, lengthening thoracic cavity External intercostal muscles contract, lifting ribs up & out Sternum pushed forward, enlarging chest from front to back Incr. lung volume & decr. Intrapulmonic pressure allows atm air to move form area of greater pressure (outside air) into area of lower pressure (within lungs) o Relaxation/recoil expiration Diaphragm relaxes & moves up; ribs move down, & sternum drops back into position
Causes decr. Volume in lungs & incr. In intrapulmonic pressure Air moves from high pressure to low & air expired
Respiration o Gas exchange at terminal alveolar capillary system o Gases exchanged b/w air & blood thru dense network of capillaries in the respiratory portion of the lungs & think alveolar walls Via diffusion O2 & CO2 between air (alveoli) and blood (capillaries) O2 in alveoli moves to capillaries containing unoxygenated venous blood CO2 diffuses across capillary into alveoli & exhaled o Diffusion dependent on 4 factors Change in surface area available (atelectasis incomplete lung expansion or collapse of alveoli) Thickening of alveolar-capillary membrane Partial pressure (less O2 = less available for diffusion) Solubility & molecular weight of gas CO2 greater solubility & faster able to release thru exhalation Perfusion o Oxygenated capillary blood passes thru tissues of body o Greater activity inc. blood o Dependent on position, activity level, & blood supply o Hypoxia inadequate amount of oxygen available to cells o Dyspnea difficulty breathing o Hypoventilation - decreased rate or depth of air movement into lungs Leads to small PP, incr. BP, restlessness, anxiety, confusion, clubbing, decr. Urinary output, weakness of extremity muscles & muscle pain
Describe age-related differences that influence the care of patients with respiratory problems RESPIRATORY VARIATIONS IN THE LIFE CYCLE INFANT (<1 YEAR) EARLY CHILD (1 LATE AGED ADULT (65>) 5) CHILD (612) RR 30-60 20-40 15-25 16-20 breaths/min breaths/min breaths/min breaths/mi n RESPIRATORY Abdominal Abdominal Thoracic Thoracic; regular PATTERN breathing, breathing; breathing; irregular in rate irregular regular & depth CHEST WALL Thin, little Same as infants Further Thin, structures muscle, ribs & but more fat subcut. prominent sternum visible Fat &
BREATH SOUNDS
Loud, harsh crackles at end of deep inspiration Round Lungs go from fluid filled to air filled organs Surfactant formed 34-36 weeks
Loud harsh expiration longer than inspiration Elliptical Eustachian tubs, bronchi & bronchioles are enlarged routine colds & infections decr. Until child enters school
SHAPE OF THORAX MISC.
structures less prominent Clear inspiration is longer than expiration Elliptical
Clear
Barrel shaped or elliptical Airways are less elastic Diaphragm moves less efficiently Chest cant stretch as much Airways collapse
Perform a respiratory assessment using appropriate interview questions and physical assessment skills Assessing o Health history o Ask patient, labs figure out what problems can be treated independently by nursing Nursing history o Why patient needs nursing care & what kind of care is required to maintain a sufficient intake of air o Interview qs help identify current or potential health deviations, actions performed by patient for meeting respiratory needs * effects of such actions, contributing factors, the use of any aids to improve intake of air & effects on patients lifestyle & relationships with others Usual patterns of respiration how would you describe your breathing & do you have allergens? Medications are you taking any for breathing? Health history do you have heart, lung, or breathing conditions? Recent changes do you have chest pain, respiratory infections? Lifestyle & environment do you smoke? Cough do you wheeze, where do you work? Sputum do you ever spit out mucus? What color? Chest pain where is the pain, how long? Physical assessment Inspection o Adult chest slightly convex w/ no sternal depression Front-back diameter < transverse o Infants chest wall thin ribs, sternum & xiphoid process seen Front-back = transverse o Bony landmarks prominent b/c loss of fat o Contour of intercoastal space should be flat & depressed o Movement of chest symmetrical Skin warm, dry, even in color Normal respirations quiet & nonlabored
o o
Tachypnea rapid breathing Bradypnea slow breathing
Palpation o Palpate trachea equidistant from each clavicle o Measure thoracic excursion by placing hands on patients posterior thorax @ 10th rib with both thumbs almost touching vertebrae Ask pt to take few deep breaths & watch movement of hands Thumbs usually move 5 8 cm at max inspiration o Tactile fremitus Capacity to feel sound on chest wall Place palm to patients chest wall, avoiding bony areas (scapula) Ask patient to repeat multi-syllable words and feel vibration Greatest intensity anterior & posterior base of neck & along trachea & large bronchi Pneumonia incr. & COPD decr. Sounds [solid tissue conducts better sounds) Percussion o Position of lungs, density of lung tissue & identify changes in tissue Auscultation o Stethoscope move from apex to base of lungs, comparing 1 side w/ the other side while listening to complete respiratory cycle (inspiration & expiration) o Normal breath sounds: Vesicular (low pitched, soft sounds heard over peripheral lung fields) Bronchial (loud, high pitched sounds heard over trachea & larynx) Bronchovesicular (medium pitched blowing sounds heard over major bronchi) o Breathe through open mouth Record location, changed in breath sounds after coughing, & phase of respiration in which abnormal sound is heard (wheezing on expiration) Adventitious abnormal lung sounds discontinuous or continuous Crackles heard on inspiration, soft high pitched d/c popping sounds o Produced by fluid in airways or alveoli & delayed reopening of collapsed alveoli o Occur due to inflammation or congestion (pneumonia, COPD) o Crackles fine or coarse Fine brief (hair rubbing) Coarse louder, moist, bubbling Wheezes continuous, musical sounds, produced as air passes thru airways constricted by swelling, narrowing, secretions, or tumors o Sibilant or sonorous Sibilant high pitched & whistling Sonorous wheezes heard over larger airways like a snore Asthma, tumors or buildup of secretions Common diagnostic tests o Pulmonary function studies Evaluates patients with respiratory disorders & are performed routinely to evaluate pulmonary status & detect abnormalities Inert gas dilution, nitrogen washout & body plethysmography measure lung volumes Diffusion capacity estimates patients ability to absorb alveolar gases & determines if gas-exchange problem exists Max respiratory pressures help evaluate neuromuscular cause of respiratory dysfunction
Spirometry
Exercise testing helps evaluate dyspnea during exertion
Volume of air in L exhaled or inhaled by a patient over time Evaluates lung function & airway obstruction thru respiratory mechanics Measures degree of airway obstruction & evaluates response to inhaled meds o Spirometer - measures lung V & airflow Peak expiratory flow rate o PEFR pt of highest flow during forced expiration o Reflects changes in size of pulmonary airways & is measured using a peak flow meter o Used for patients with moderate or severe asthma to measure severity of disease & degree of disease control o Patient stands straight & takes deep breath & places peak flow meter in mouth, closing lips o Forcibly exhales into meter & indicator rises to a # (3x done) o Normal values established thru height, age, gender o Used to track disease progression & regulate treatment Pulse oximetry o Measures arterial oxyhemoglobin saturation (SaO2 or SpO2) of arterial blood o Monitors pts with O2 therapy, titrating O2 therapy, monitoring those at risk for hypoxia & monitoring postop patients o Desat indicates gas exchange abnormalities o 95% - 100% normal o <90% are abnormal, indicate that oxygenation to tissues is inadequate & should be investigates for potential hypoxia or technical error Thoracentesis o Procedure of puncturing the chest wall & aspirating pleural fluid o Patient sits on chair, arms folded & resting on pillow o Fluid removed with syringe o Monitor patients color, pulse, RR o Large amt of fluid removed decr. In RR
Describe nursing strategies to promote adequate respiratory functioning & identify their rationale Promoting optimal function Teaching about pollution-free environments o Involve job change, protective equipment o Dusting & vaccuming 2x/week o Pollution alerts stay home or reduce activities o Stop smoking Reducing anxiety o Listen & dont judge Maintaining good nutrition o Measure H, W, protein o Intake vitamins o 6 small meals vs 3 Promoting comfort Positioning Fowlers position (tilted 45-60 deg) Prone position (lie on abdoment) Maintaining adequate fluid intake 2-3 qts/day
Providing humidified air Dry air removes normal moisture in passages that protect against irritation & infection Steam vaporizer Cool mist can be medium for pathogen if not cleaned properly Promoting proper breathing Efficient ventilations, decr. Work of breathing Deep breathing Overcome hypoventilation (decr. Amt of air enters & leaves lungs) Using incentive spirometry Visual reinforcement for deep breathing by the patient Assists pt to breathe slowly & deeply & to sustain max inspiration Pursed-lip breathing For pts with dyspnea or panic Exhaling thru pursed lips allows slow & prolonged expiration Prevents collapse of small airways, improves air exchange Relaxation Sitting upright, inhales thru nose while counting to 3 & exhales slowly During exhalation, pt counts to 8 Abdominal or diaphragmatic breathing Dec. RR, incr. tidal V, reduced functional residual capacity Place 1 hand on stomach & other on middle of chest Breathe in slow thru nose, letting abdomen protrude out Breathe thru pursed lips while contracting abdominal muscles, w/ 1 hand pressing inward & upward on abdomen Repeats for 1 min & rest for 2 min Promoting & controlling coughing o Dry nonproductive Sputum clearing throat o Most effective when sitting upright with feet on floor Voluntary coughing o Improves oxygenation, taste of food, removes secretions o Assisted cough pressure placed on abdomen below diaphragm in rhythm w/ exhalation o Similar to Heimlich but less force Involuntary cough o Respiratory tract infections & irritations Cough meds Expectorants o Remove secretions o Liquifies thick mucus o Taking fluids aid Cough suppressants o Depress a body function cough reflex o Codeine o Drowsiness side effect o Dexromethorphan Lozenges o Relieve mild, nonproductive cough in people w/o congestion o In mouth until dissolves Chest physiotherapy o Loosen & mobilize secretions, incr. mucus clearance o Dome-shaped rythym strike area of lung 30-60 sec several times a day
o Hold hands plat on chest wall as patient exhales Postural drainage o Fowlers (head of bed elevated 45 60 deg) apical secretions of upper lobes of lung o Lying position posterior sections of lungs o Lying on left side w/ pillow drain rt lobe of lung o Trendelenburg (lie pillow b/w butt & back knees bent) drain lower lobes of lung Suctioning o Remove secretions sterily o Irritates mucosa & can lead to hypoxemia - insuffient O2 in blood o Pre-ox pt b4 suctioning o Incr. ox or take breathes b4 o Relieves respiratory distress Oxygen o Flow rate amt of O2 delivered to patient Masks o Simple connected to oxygen tubing, humidifier, & flow meter Has vents on its sides that allow room air to leak in at many places dilutes source of O2 Incr. delivery needed for <12 hours o Partial rebreather same as simple except has reservoir bag for collection of 1st part of pts exhalation Rest of exhaled air exists thru vents Patient rebreathes 1/3 of expired air from reserved bag Can inhale room temp O2 if supply in mask is interrupted o Nonbreather highest concentration of O2 2 1way valves prevent patient from rebreathing exhaled air Reservoir bag filled with O2 that enters mask on inspiration Exhaled air escapes thru side vents o Venturi - allows mask to deliver most precise concentrations of O2 Large tube with O2 inlet As tube narrows, pressure drops, causing air to be pulled in thru side ports Ports are adjusted according to prescription Oxyen tent like a fridge
Plan, implement, and evaluate nursing care related to select nursing diagnoses involving respiratory problems Planning o Improved gas exchange in lungs by absences of cyanosis or chest pain & pulse oximetry >95% o Relate causative factors if known & demonstrate a method of coping with these factors o Preserve pulmonary function by maintaining an optimal level of activity o Demonstrate self-care behaviors that provide relief from symptoms & prevent further pulmonary probs o (By March 15 patient will be able to walk one flight of stairs without dyspnea) Implementing o Suctioning, chest physiotherapy, meds, oxygen, CPR, etc. Evaluating o Examine patients projected progress in meeting outcomes planned
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Stars Academy Lahore: Stars Entry Test SystemDocument2 pagesStars Academy Lahore: Stars Entry Test SystemMemoona GullNo ratings yet
- Introduction to Mechanical VentilationDocument4 pagesIntroduction to Mechanical VentilationvgmanjunathNo ratings yet
- Ineffective Airway ClearanceDocument4 pagesIneffective Airway ClearanceArabelle GONo ratings yet
- 3 Spinal Cord Injury Nursing Care PlanDocument9 pages3 Spinal Cord Injury Nursing Care PlanCyrus De Asis88% (8)
- Mechanical VentilationDocument18 pagesMechanical VentilationM BNo ratings yet
- Thoracic SurgeryDocument28 pagesThoracic Surgeryapi-3840195100% (5)
- Nursing Care Plan for Impaired Gas ExchangeDocument5 pagesNursing Care Plan for Impaired Gas ExchangeCuttie Anne GalangNo ratings yet
- NCP - Ineffective Breathing PatternDocument4 pagesNCP - Ineffective Breathing PatternPRINCESS KOBAYASHINo ratings yet
- QualifiedPhysio Acute-Respiratory Interview Preparation Pack PDFDocument36 pagesQualifiedPhysio Acute-Respiratory Interview Preparation Pack PDFdanypunct100% (2)
- Oxylog 3000plus Guia Ajustes InicialesDocument3 pagesOxylog 3000plus Guia Ajustes InicialesFrancisco José Lencina SalarNo ratings yet
- Pulmovista 500: Bedside Respiratory MonitoringDocument8 pagesPulmovista 500: Bedside Respiratory MonitoringMaria DronNo ratings yet
- Nursing Care Plan for a Client with Ineffective Breathing PatternDocument3 pagesNursing Care Plan for a Client with Ineffective Breathing PatternPrincess Faniega SugatonNo ratings yet
- 1808 - Data Nov SD TGL 15, Mic, PhenotypeDocument108 pages1808 - Data Nov SD TGL 15, Mic, PhenotypeDeasy NatalianiNo ratings yet
- Cat Anatomy and PhysiologyDocument44 pagesCat Anatomy and PhysiologyJovana Stankovic Popovic100% (3)
- First Periodical Test g9Document7 pagesFirst Periodical Test g9lucia h. enriquezNo ratings yet
- Respiratory System LessonDocument11 pagesRespiratory System LessonAcza Jaimee C. Kalaw100% (5)
- SH emDocument4 pagesSH emMaura NuezcaNo ratings yet
- Flexovit Abrasives - Shop and Plumber RollsDocument1 pageFlexovit Abrasives - Shop and Plumber RollsFlexovit AbrasivesNo ratings yet
- Normal NewbornDocument19 pagesNormal Newbornkozume kenmaNo ratings yet
- Care of Clients With Problems in Oxygenation: Lecturer: Roselle Joy C. Balaquit, RNDocument74 pagesCare of Clients With Problems in Oxygenation: Lecturer: Roselle Joy C. Balaquit, RNdodong skyrose100% (2)
- Respiratory System GuideDocument54 pagesRespiratory System GuideHannah YsaBelle LeguroNo ratings yet
- Lecture 1 Chest TraumaDocument19 pagesLecture 1 Chest Traumaj.doe.hex_870% (1)
- Anatomy and Physiology of NoseDocument32 pagesAnatomy and Physiology of NoseBinita ShakyaNo ratings yet
- Introduction to Respiratory System ExaminationDocument131 pagesIntroduction to Respiratory System ExaminationMohamed HefnyNo ratings yet
- SPS Science F3 01 PDFDocument13 pagesSPS Science F3 01 PDFMac SensNo ratings yet
- SDS Underwater Welding Electrodes 2018 PDFDocument11 pagesSDS Underwater Welding Electrodes 2018 PDFVictor AcostaNo ratings yet
- Polytetrafluoroethylene Toxicosis in ChicksDocument4 pagesPolytetrafluoroethylene Toxicosis in ChicksCamila IssaNo ratings yet
- Fccu Catalyst Material Safety Data Sheet (2001)Document2 pagesFccu Catalyst Material Safety Data Sheet (2001)Knipselkrant CuracaoNo ratings yet
- Pathophysiology: Risk FactorsDocument4 pagesPathophysiology: Risk FactorsEdson John DemayoNo ratings yet
- Chest TubesDocument3 pagesChest TubesKay BristolNo ratings yet