Professional Documents
Culture Documents
Labor and Delivery
Uploaded by
Jinky TenezaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Labor and Delivery
Uploaded by
Jinky TenezaCopyright:
Available Formats
LABOR and DELIVERY
Also known as Parturition, childbirth, birthing. Is the process by which the fetus & placenta are expelled from the uterus and the vagina into the external environment. PROSTAGLANDIN THEORY A parturient is a woman in labor. It has been known that when fetus has Toco - and toko- (Gr.) are combining reached maturity, the fetal membranes forms meaning childbirth. produce large amount of arachidonic acid Eutocia normal labor which is converted by maternal decidua Dystocia difficult labor into a prostaglandin, a hormone that Normally, labor begins when the fetus is initiates uterine contractions. sufficiently mature, yet not too large to During labor the level of arachidonic acid cause difficulties in delivery. in the amniotic fluid is very high resulting In some instances, labor begins before in increased productions of the fetus is mature (premature birth); in prosttaglandin. others labor is delayed (postmature birth). It is unknown why this occurs 1. THEORY OF THE AGING PLACENTA As the placenta ages, it becomes less THEORIES ON THE ONSET OF LABOR efficient, producing decreasing amount of progesterone. 1. FETAL ADRENAL RESPONSE THEORY This progesterone decline allows the Hippocrates, the father of medicine, concentration of prostaglandin and was the first person to propose this estrogen to rise steadily. theory which states that certain hormones produced by the fetal adrenal and pituitary gland initiates labor contraction. 1. OXYTOCIN STIMULATION THEORY Studies have shown that as pregnancy near term, oxytocin production by the posterior pituitary gland while the production of oxytocinase by the placenta . Oxytocin stimulates uterine contractions while oxytocinase inhibits uterine contractions. As a result the uterus becomes increasingly sensitive to oxytocin. 1. UTERINE STRETCH THEORY According to this theory any hallow organ stretched, will always contract & expel its content. A pregnancy advances, the uterus becomes increasingly distended by the growing fetus, placenta and amniotic fluid, distention of the uterus creates pressure on the nerve endings which stimulates uterine contractions. 1. PROGESTERONE DEPRIVATION THEORY Progesterone helps maintain pregnancy by its relaxant effect on the smooth muscles of the uterus, thereby, preventing uterine contractions. PRELIMINARY SIGNS OF LABOR 1) LIGHTENING (The baby dropped) or descent of the fetal presenting part into the pelvis, occurs approximately 10 14 days before labor begins. Engagement descent of the biparietal
plane of the fetal head to a level below that of the pelvic inlet. Fixation is descent of the fetal head to the inlet to a level below that of the pelvic inlet. Floating When head is still movable above the pelvic inlet on palpation
As pregnancy nears term, the production of progesterone by the placenta decreases, this decline in progesterone allows uterine contraction to occur.
2) h IN LEVEL OF ACTIVITY 3) WEIGHT LOSS 2 wks before labor, the woman experience sudden weight loss of about 2-3 lbs. 4) BRAXTON HICKS CONTRACTION 5) RIPENING OF THE CERVIX goodells sign
SIGNS OF TRUE LABOR Uterine contractions surest sign Show Bloody show, blood mixed with mucus (operculum). Rupture of the membranes
Bending of the head onto the chest making the smallest anterior-posterior diameter (suboccipitobregmatic) present to the birth canal. Effacement softening & thinning of cervix. Use % in unit of measurement Primigravidas usually efface more quickly than they dilate. Multiparas typically will experience effacement and dilatation at the same time. Dilatation widening of cervix. Unit used is cm.
INTERNAL ROTATION Occiput rotates until it is superior or just below the symphysis pubis bringing the head into the best relationship with the pelvic outlet; shoulder enterd the pelvic inlet. EXTENSION Extension of the head; face and chin are born. 5 Ps of LABOR (Factors of Labor) EXTERNAL ROTATION 1. PASSAGES (Pelvic Area) or Restitution Hard passages: Bony pelvis Head rotates back to diagonal or Soft passages: Lower uterine segment, transverse position, shoulders cervix, vagina, pelvic floor and enter the outlet and are born. perineum. EXPULSION 2. POWER Rest of the baby is born. Primary force: Involuntary uterine contractions. MANEUVER Secondary force: Voluntary use of thoracic, diaphragm and abdominal 1. RITGENS MANEUVER Insertion muscles when the mother bears of the hand and application of down. upward pressure on the fetal chin 3. PASSENGER (Baby) and as to the other hand applies Fetal positions, presentation gentle downward pressure on the and attitude. fetal occiput to allow controlled 4. PERSON (Mother) delivery of the fetal head. Maternal attitude during labor 5. POSITION 2. BRANDT ANDREWS MANEUVER Maternal position during labor is a manual technique to help and delivery facilitate the delivery of the MECHANISM OF LABOR Remember: ED FIRE ERE E Engagement D Descent F Flexion I Internal R Rotation E Extension E External R Rotation E Expulsion ENGAGEMENT Setting of the fetal head into the pelvis. DESCENT Downward movement of the biparietal diameter of the fetal head to within the pelvic inlet. FLEXION placenta. The technique is coiling the umbilical cord through forcep. (up, down and side technique.) 3. MODIFIED CREDES MANEUVER is a manual technique to help facilitate the delivery of the placenta. Gentle pressure on the contracted uterine fundus by the Physician/midwife.
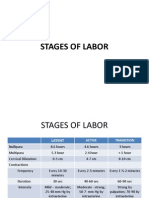
STAGES OF LABOR FIRST SECOND THIRD FOURTH : CERVICAL DILATATION STAGE : EXPULSIVE STAGE : PLACENTAL STAGE : RECOVERY STAGE
2. EXPULSIVE STAGE
Begins with full dilation and cervical effacement to delivery of an infant. Contraction change from characteristic crescendo to decresendo pattern to an overwhelming uncontrolable urge to push or bear down with each contraction as if to move her bowels. May experience nausea and vomiting because pressure is no longer exerted on her stomach as fetus descends in pelvis. Begins with birth of the infant and ends with separation and expulsion of the placenta. Usually 5 minutes after the birth of an infant. (to 30mins)
1. CERVICAL DILATATION STAGE
Begins with the labor contraction and ends with complete dilation of the cervix. (10cm)
3 PHASES
3. PLACENTAL STAGE
LATENT (0-4 cm) ACTIVE (4-8 cm) TRANSITIONAL (8-10 cm)
1.
2.
LATENT (0-4 cm) Contractions are MILD and SHORT 5 10 minutes interval Phases last approximately 6 hrs Nullipara 4.5 hrs Multipara ACTIVE (4-8 cm) Cervical dilation occur more RAPIDLY, increase in duration If BOW not yet ruptured: Woman can take a bath/ void. Begin to cause true discomfort. Exciting time for woman. Abdominal breathing (Advice) Intensity: Moderate to strong Phases last approximately 3 hrs Nullipara 2hrs Multipara
SIGNS OF PLACENTAL SEPARATION 1) Lengthening of the umbilical cord 2) Uterus become firm an globular 3) Sudden gush of blood from the vagina 4) Firm contraction of uterus 5) Appearance of placenta from the vaginal opening. SIGNS OF PLACENTAL EXPULSION The placenta is delivered: Natural bearing effort of the mother or Gentle presure on the contacted uterine fundus by Physician/ OB. (Modified Credes Maneuver)
3.
TRANSITIONAL (8-10 cm) Maximum dilation of 8-10cm. Mood of the mother suddenly changes and the nature of contraction intensified.
4. RECOVERY STAGE
Begins from expulsion of the placenta to 2 hours after delivery.
SECOND LETTER: Denotes fetal landmark O for occiput M for mentum S for sacrum A for acromium LAST LETTER: Whether the landmark points anteriorly (A), posteriorly (P), or transversely (T).
FETAL ASSESSMENTS
FETAL LIE Relationship of fetal long axis to maternal long axis (spine). a. Transverse Shoulder presents b. Longitudinal Vertex or breech. PRESENTATION Fetal part entering the pelvic inlet first. a. Cephalic (Vertex/ Brow/ Face) b. Breech (Complete/ Frank/ Footling) ATTITUDE Relationship of fetal parts to one another. (degree of flexion) A. Complete flexion. B. Moderate flexion. C. Poor flexion. D. Hyperextension STATION Relationship of the presenting part of a fetus to the level of the ischial spine.
Each presenting part has the possibility of six positions. They are normally recognized for each position--using "occiput" as the reference point.
1. 2. 3. 4. 5. 6.
Left occiput anterior (LOA). Left occiput posterior (LOP). Left occiput transverse (LOT). Right occiput anterior (ROA). Right occiput posterior (ROP). Right occiput transverse (ROT).
POSITION Relationship of presenting fetal part to the quadrants of maternal pelvis. FOUR QUADRANTS: a. Right Anterior b. Left Anterior c. Right Posterior d. Left Posterior e. Right Transverse f. Left Transverse
POSITION is indicated by an abbreviation of 3 letters:
OBSERVATIONS ABOUT POSITIONS (a) LOA and ROA positions are the most common and permit relatively easy delivery. (b) LOP and ROP positions usually indicate labor may be longer and harder, and the mother will experience severe backache. KNOWING POSITIONS WILL HELP YOU TO IDENTIFY WHERE TO LOOK FOR FHT's. 1. BREECH. This will be upper R or L quad, above the umbilicus. 2. VERTEX. This will be lower R or L quad, below the umbilicus.
FIRST LETTER: Whether the landmark is pointing to the mothers right (R) or left (L).
You might also like
- Intrapartum QuizletDocument15 pagesIntrapartum Quizletanon_616227840100% (3)
- Stages of LaborDocument30 pagesStages of LaborPerrilyn Perey100% (1)
- Maternal and Child Nursing Module 1: Obstetric Nursing OverviewDocument18 pagesMaternal and Child Nursing Module 1: Obstetric Nursing Overviewjanina myka100% (1)
- Stages of Labor and DeliveryDocument7 pagesStages of Labor and DeliveryAijem Ryan86% (7)
- Handout OB MidtermsDocument3 pagesHandout OB Midtermsaidan valin100% (7)
- MCN PartographDocument2 pagesMCN PartographAlec AnonNo ratings yet
- AntepartumDocument32 pagesAntepartumphoenix180100% (1)
- Maternal NursingDocument37 pagesMaternal NursingCai Velasco DecenaNo ratings yet
- Assessment of NewbornDocument26 pagesAssessment of Newbornaybee_14No ratings yet
- New Born CareDocument17 pagesNew Born CareHarrison Tallod100% (1)
- Labor and DeliveryDocument6 pagesLabor and Deliveryjenryl91% (11)
- Delivery Definitions and StagesDocument29 pagesDelivery Definitions and StagesTrisha100% (1)
- Labor and DeliveryDocument14 pagesLabor and Deliverydexter100% (15)
- Complications of LaborDocument54 pagesComplications of Laborallie-jones-6489100% (2)
- Complications of PregnancyDocument40 pagesComplications of PregnancyNatalie Pemberton100% (1)
- Intrapartum CareDocument14 pagesIntrapartum CareChristian80% (5)
- Topic # 2 PartographDocument42 pagesTopic # 2 PartographJayrelle D. Safran100% (1)
- Stages of LaborDocument11 pagesStages of LaborWindelyn Gamaro100% (1)
- OB RNSG 2208 Mid-term OutlineDocument23 pagesOB RNSG 2208 Mid-term OutlineAnnissaLarnardNo ratings yet
- A Premature Infant Is An Infant Born Before 37 WK GestationDocument5 pagesA Premature Infant Is An Infant Born Before 37 WK GestationKamila KawaiiNo ratings yet
- OB MedsDocument19 pagesOB Medsohsnapitslei100% (2)
- Gravida - The Number of Pregnancies That o Progesterone Deprivation TheoryDocument27 pagesGravida - The Number of Pregnancies That o Progesterone Deprivation TheoryRoshin Tejero100% (1)
- Components of LaborDocument5 pagesComponents of LaborJeraldine Lindo100% (4)
- Amniotic Fluid EmbolismDocument8 pagesAmniotic Fluid EmbolismjNo ratings yet
- Gynecology Test QuestionsDocument6 pagesGynecology Test Questionsdhodejun lizhaldeNo ratings yet
- Maternity NursingDocument6 pagesMaternity Nursingrhenier_ilado0% (1)
- Care of The NewbornDocument5 pagesCare of The Newbornbuzz Q100% (2)
- High - Risk PregnancyDocument110 pagesHigh - Risk PregnancyAndre DityaNo ratings yet
- Complications of Labor and DeliveryDocument5 pagesComplications of Labor and DeliveryJill Hill100% (1)
- Labor and DeliveryDocument7 pagesLabor and Deliveryplethoraldork100% (20)
- Labor and Birth: Theories, Signs, and ContractionsDocument15 pagesLabor and Birth: Theories, Signs, and ContractionsMARIA PEARLITA TANNo ratings yet
- Principles of Postpartum Nursing CareDocument2 pagesPrinciples of Postpartum Nursing CareZaire DylanNo ratings yet
- Labor & Delivery Nursing Physical ExamDocument72 pagesLabor & Delivery Nursing Physical ExamJay Depakakibo Gallardo100% (1)
- Complications in PregnancyDocument81 pagesComplications in PregnancyTia TahniaNo ratings yet
- NCM107 - Chapter 04-Lesson 3 Postpartal CareDocument22 pagesNCM107 - Chapter 04-Lesson 3 Postpartal CareJosephine LoriaNo ratings yet
- Stages of LaborDocument23 pagesStages of LaborPortia Dulce Toquero100% (5)
- ObstetricsDocument19 pagesObstetricsMoon Boo ChanNo ratings yet
- CPM16TH Essential Newborn CareDocument11 pagesCPM16TH Essential Newborn CareKevin AgbonesNo ratings yet
- Essential Newborn CareDocument104 pagesEssential Newborn CareNacel Celeste100% (11)
- Labor and Delivery Lecture NotesDocument14 pagesLabor and Delivery Lecture Notescolek22100% (22)
- Stages of Labor Nursing ConsiderationsDocument5 pagesStages of Labor Nursing Considerationsneleh gray100% (2)
- Newborn AssessmentDocument3 pagesNewborn AssessmentValerie Ybañez Peñalber100% (2)
- Chapter 8 Nursing Care During Labor and Pain ManagementDocument34 pagesChapter 8 Nursing Care During Labor and Pain ManagementMatthew Ryan100% (1)
- Nursing OB Exam Q & ADocument173 pagesNursing OB Exam Q & Ajoerobinson8889323100% (8)
- Postpartum Period HandoutsDocument8 pagesPostpartum Period HandoutsChared LumbaNo ratings yet
- Care of The Woman During PregnancyDocument99 pagesCare of The Woman During PregnancyFrancr ToledanoNo ratings yet
- 15 Nursing Care of A Family During Labor and BirthDocument14 pages15 Nursing Care of A Family During Labor and BirthNurse UtopiaNo ratings yet
- Perineal CareDocument7 pagesPerineal CareAna Maria Teresa H RollanNo ratings yet
- NURS 3337 Day1 WorkbookDocument18 pagesNURS 3337 Day1 WorkbookEmerald Holly TagoNo ratings yet
- 6 Antepartum Care PDFDocument24 pages6 Antepartum Care PDFmohammed farajiNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- MATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideFrom EverandMATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Maternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideFrom EverandMaternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideNo ratings yet
- NEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideFrom EverandNEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideNo ratings yet
- Inflamed Trachea, (Tracheitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandInflamed Trachea, (Tracheitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Drug Therapy During PregnancyFrom EverandDrug Therapy During PregnancyTom K. A. B. EskesRating: 5 out of 5 stars5/5 (1)
- 10 Rights in Giving MedicationDocument11 pages10 Rights in Giving MedicationJinky TenezaNo ratings yet
- DOH Maternal Health ProgramDocument6 pagesDOH Maternal Health ProgramJinky TenezaNo ratings yet
- Survey The Scene: (Check ABC) LLF Position, Check For 10 SecondsDocument1 pageSurvey The Scene: (Check ABC) LLF Position, Check For 10 SecondsJinky TenezaNo ratings yet
- Glucose-6-Phosphate Dehydrogenase Deficiency - Overview: Symptom Treatment Prevention All InformationDocument2 pagesGlucose-6-Phosphate Dehydrogenase Deficiency - Overview: Symptom Treatment Prevention All InformationJinky TenezaNo ratings yet
- HBMRDocument3 pagesHBMRJinky TenezaNo ratings yet
- Glucose-6-Phosphate Dehydrogenase Deficiency - Overview: Symptom Treatment Prevention All InformationDocument2 pagesGlucose-6-Phosphate Dehydrogenase Deficiency - Overview: Symptom Treatment Prevention All InformationJinky TenezaNo ratings yet
- Group Activity Case StudyDocument1 pageGroup Activity Case StudyJinky TenezaNo ratings yet
- DOH releases 2 new vaccines to protect childrenDocument4 pagesDOH releases 2 new vaccines to protect childrenJinky TenezaNo ratings yet
- Medical PrefixesDocument74 pagesMedical PrefixesJinky TenezaNo ratings yet
- PositionsDocument12 pagesPositionsJinky TenezaNo ratings yet
- PositionsDocument12 pagesPositionsJinky TenezaNo ratings yet
- Magna Carta of Public Health Workers ActDocument6 pagesMagna Carta of Public Health Workers ActJinky TenezaNo ratings yet
- Common AbbreviationsDocument14 pagesCommon AbbreviationsJinky TenezaNo ratings yet
- Breast Self ExamDocument35 pagesBreast Self ExamJinky TenezaNo ratings yet
- HDPS 1303 - 930425105424Document6 pagesHDPS 1303 - 930425105424Cheryl LimNo ratings yet
- Mimw With CoverDocument13 pagesMimw With Coverank123qwerNo ratings yet
- Syllabus of BS English (Language & Literature) Implemented From 1 Semester Fall 2021Document95 pagesSyllabus of BS English (Language & Literature) Implemented From 1 Semester Fall 2021Lahore PunjabNo ratings yet
- Ore Pass Design and Placement Koivisto Mikko PDFDocument105 pagesOre Pass Design and Placement Koivisto Mikko PDFasepdayat100% (1)
- Past Simple - Present PerfectDocument5 pagesPast Simple - Present PerfectAnonymous MCobwixNo ratings yet
- 7 Day Diet AnalysisDocument5 pages7 Day Diet AnalysislipakevinNo ratings yet
- The Directors Six SensesDocument31 pagesThe Directors Six SensesMichael Wiese Productions93% (14)
- Philo 12Document2 pagesPhilo 12Rachel LaganNo ratings yet
- Case Study For Engineering ProblemDocument37 pagesCase Study For Engineering ProblemAfiq AfifeNo ratings yet
- Winning Market Through Market Oriented Strategic PlanningDocument25 pagesWinning Market Through Market Oriented Strategic PlanningKafi Mahmood NahinNo ratings yet
- English - Vocabulary - in - Use - Pre - Intermediate - and - Intermediate - Book 2Document2 pagesEnglish - Vocabulary - in - Use - Pre - Intermediate - and - Intermediate - Book 2Наталия БруслинецNo ratings yet
- List of As... SimilesDocument3 pagesList of As... SimilesFara ZahariNo ratings yet
- Oracle Induction - Introduction Foot Print and Instances For Perfect ExecutionDocument11 pagesOracle Induction - Introduction Foot Print and Instances For Perfect Executioneuge_prime2001No ratings yet
- History E XDocument13 pagesHistory E XTamboli Shaikh Muaavvir AkbarNo ratings yet
- The Experiences and Challenges Faced of The Public School Teachers Amidst The COVID-19 Pandemic: A Phenomenological Study in The PhilippinesDocument21 pagesThe Experiences and Challenges Faced of The Public School Teachers Amidst The COVID-19 Pandemic: A Phenomenological Study in The PhilippinesDE LOS REYES MARY ZEALANo ratings yet
- Petitioner Respondent: Civil Service Commission, - Engr. Ali P. DaranginaDocument4 pagesPetitioner Respondent: Civil Service Commission, - Engr. Ali P. Daranginaanika fierroNo ratings yet
- Set-2 Answer? Std10 EnglishDocument13 pagesSet-2 Answer? Std10 EnglishSaiyam JainNo ratings yet
- A Study on Student Budgeting HabitsDocument41 pagesA Study on Student Budgeting Habitsbornak BonalasNo ratings yet
- Activity 13Document13 pagesActivity 13Lielannie CarasiNo ratings yet
- ABC Pre School: (Please Refer Advertisement in This Section)Document5 pagesABC Pre School: (Please Refer Advertisement in This Section)hemacrcNo ratings yet
- Signals SyllabusDocument1 pageSignals SyllabusproNo ratings yet
- G11 F2F ScheduleDocument3 pagesG11 F2F ScheduleQueenie Marie Obial AlasNo ratings yet
- Arrest of Leila de Lima (Tweets)Document74 pagesArrest of Leila de Lima (Tweets)Edwin MartinezNo ratings yet
- Noon and Tanween RulesDocument56 pagesNoon and Tanween RulesReadRead100% (2)
- SkipTheFlip Physical PDFDocument230 pagesSkipTheFlip Physical PDFSebi100% (4)
- Civet CoffeeDocument8 pagesCivet CoffeeAn NhiênNo ratings yet
- Prambanan Temple LegendDocument1 pagePrambanan Temple LegendClara NadaNo ratings yet
- English Language (1122)Document26 pagesEnglish Language (1122)TD X Mzinda100% (1)
- Preventive MaintenanceDocument19 pagesPreventive Maintenancefaizan9970% (1)
- A Review of The Book That Made Your World. by Vishal MangalwadiDocument6 pagesA Review of The Book That Made Your World. by Vishal Mangalwadigaylerob100% (1)