Professional Documents
Culture Documents
Nephrotic Syndrome
Uploaded by
Anjhiene CambaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nephrotic Syndrome
Uploaded by
Anjhiene CambaCopyright:
Available Formats
Nephrotic syndrome is a nonspecific disorder in which the kidneys are damaged, causing them to leak large amounts of protein
(proteinuria at least 3.5 grams per day per 1.73m body surface area) the urine. Kidneys affected by nephrotic syndrome have small pores in the podocytes, large enough to permit proteinuria (and subsequently hypoalbuminemia, because some of the proteinalbumin has gone from the blood to the urine) but not large enough to allow cells through (hence no hematuria). By contrast, in nephritic syndrome, RBCs pass through the pores, causing hematuria.
2 [2]
from the blood into
Presentation
It is characterized by proteinuria (>3.5g/day), hypoalbuminemia, hyperlipidemia and edema which is generalized & also known as anasarca or dropsy.Common among 2-6 years old boys. The edema begins in the face. Lipiduria (lipids in urine) can also occur, but is not essential for the diagnosis of nephrotic syndrome. Hyperlipidemia is caused by two factors:
Hypoproteinemia stimulates protein synthesis in the liver, resulting in the overproduction of lipoproteins. Lipid catabolism is decreased due to lower levels of lipoprotein lipase, the main enzyme involved in lipoprotein breakdown.
A few other characteristics seen in nephrotic syndrome are:
The most common sign is excess fluid in the body due to the serum hypoalbuminemia. Lower serum oncotic pressure causes fluid to accumulate in the interstitial tissues. Sodium and water retention aggravate the edema. This may take several forms:
Puffiness around the eyes, characteristically in the morning. Pitting edema over the legs. Fluid in the pleural cavity causing pleural effusion. More commonly associated with excess fluid is pulmonary edema.
Fluid in the peritoneal cavity causing ascites. Generalized edema throughout the body known as anasarca.
Most of the patients are normotensive but hypertension (rarely) may also occur. Anemia (iron resistant microcytic hypochromic type) maybe present due to transferrin loss. Dyspnea maybe present due to pleural effusion or due to diaphragmatic compression with ascites. Erythrocyte sedimentation rate is increased due to increased fibrinogen & other plasma contents. Some patients may notice foamy or frothy urine, due to a lowering of the surface tension by the severe proteinuria. Actual urinary complaints such as hematuria or oliguria are uncommon, though these are seen commonly in nephritic syndrome.
May have features of the underlying cause, such as the rash associated with systemic lupus erythematosus, or the neuropathyassociated with diabetes.
Examination
should
also
exclude
other
causes
of
gross
edemaespecially
the cardiovascular and hepatic system.
Investigations
The following are baseline, essential investigations:
24 hour bedside urinary total protein estimation.
2
Urine sample shows proteinuria (>3.5 g per 1.73 m per 24 hours). It is also examined for urinary casts, which are more a feature of active nephritis.
Comprehensive metabolic panel (CMP) shows hypoalbuminemia: albumin level 2.5 g/dL (normal=3.5-5 g/dL). Lipid profile. levels of cholesterol (hypercholesterolemia), specifically elevated LDL, usually with concomitantly
High
elevated VLDL is typical.
Electrolytes, urea and creatinine (EUCs): to evaluate renal function.
Further investigations are indicated if the cause is not clear:
Biopsy of kidney (in case of adult patients only). Auto-immune markers (ANA, ASOT, C3, cryoglobulins, serum electrophoresis). Ultrasound of the whole abdomen.
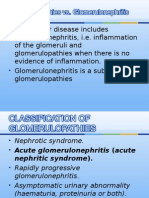
Classification and causes
Nephrotic syndrome has many causes and may either be the result of a disease limited to the kidney, called primary nephrotic syndrome, or a condition that affects the kidney and other parts of the body, called secondary nephrotic syndrome.
Etiologic classification
A broad classification of nephrotic syndrome based on etiology: Nephrotic syndrome Primary Secondary
Histologic classification
Nephrotic syndrome is often classified histologically: Nephrotic syndrome MCD FSGS MN MPGN
Primary causes
Primary causes of nephrotic syndrome are usually described by the histology, i.e. minimal change disease (MCD) like minimal change nephropathy which is the most common cause of nephrotic syndrome in children, focal segmental glomerulosclerosis (FSGS) andmembranous nephropathy (MN) like membranous glomerulonephritis which is the main cause of nephrotic syndrome in adult. They are considered to be "diagnoses of exclusion", i.e. they are diagnosed only after secondary causes have been excluded.
Secondary causes
Secondary causes of nephrotic syndrome have the same histologic patterns as the primary causes, though may exhibit some differences suggesting a secondary cause, such as inclusion bodies. They are usually described by the underlying cause.
Secondary causes by histologic pattern:
Hepatitis B & Hepatitis C Sjgren's syndrome Systemic lupus erythematosus(SLE) Diabetes mellitus Sarcoidosis Amyloidosis Drugs (such as corticosteroids, gold, intravenous heroin) Malignancy (cancer) Bacterial infections, e.g. leprosy & syphilis Protozoal infections, e.g. malaria
Focal segmental glomerulosclerosis (FSGS) Hypertensive nephrosclerosis
Human immunodeficiency virus (HIV)*Obesity Kidney loss
Minimal change disease (MCD) Drugs, especially NSAIDs in the elderly
Malignancy, especially Hodgkin's lymphoma Leukemia
Allergy
Bee sting
Differential diagnosis of gross edema
When someone presents with generalized edema, the following causes should be excluded:
1. Heart failure: The patient is older, with a history of heart disease. Jugular venous pressure is elevated on examination, might hear heart murmurs. An echocardiogram is the gold standard investigation. 2. Liver failure: History suggestive of hepatitis/ cirrhosis: alcoholism, IV drug use, some hereditary causes. Signs of liver disease are seen: jaundice (yellow skin and eyes), dilated veins over umbilicus (caput medusae), scratch marks (due to widespread itching, known as pruritus), enlarged spleen, spider angiomata, encephalopathy, bruising, nodular liver. 3. Acute fluid overload in someone with kidney failure: These people are known to have kidney failure, and have either drunk too much or missed their dialysis. 4. Metastatic cancer: when cancer spreads to the lungs or abdomen it causes effusions and fluid accumulation due to obstruction of lymphatics and veins, as well as serous exudation.
Diagnosis
The gold standard in diagnosis of nephrotic syndrome is 24 hour urine protein measurement. Aiding in diagnosis are blood tests and sometimes imaging of the kidneys (for structure and presence of two kidneys), and/or a biopsy of the kidneys.
Treatment
Treatment includes:
General measures (supportive)
Monitoring and maintaining euvolemia (the correct amount of fluid in the body):
Monitoring urine output, BP regularly. Fluid restrict to 1 L. Diuretics (IV furosemide).
Monitoring kidney function:
do EUCs daily and calculating GFR.
Treat hyperlipidemia to prevent further atherosclerosis.
Prevent and treat any complications [see below]
Albumin infusions are generally not used because their effect lasts only transiently.
[5]
Prophylactic anticoagulation may be appropriate in some circumstances.
Specific treatment of underlying cause
Immunosuppression for the glomerulonephritides (corticosteroids , ciclosporin).
2 [6]
Standard ISKDC regime for first episode: prednisolone -60 mg/m /day in 3 divided doses for 4 weeks followed by 40 mg/m /day in a single dose on every alternate day for 4 weeks.
2
Relapses by prednisolone 2 mg/kg/day till urine becomes negative for protein. Then, 1.5 mg/kg/day for 4 weeks.
Frequent relapses treated by: cyclophosphamide or nitrogen mustard or ciclosporin or levamisole.
Achieving better blood glucose level control if the patient is diabetic.
Blood pressure control. ACE inhibitors are the drug of choice. Independent of their blood pressure lowering effect, they have been shown to decrease protein loss.
Dietary recommendations
Reduce sodium intake to 10002000 mg daily. Foods high in sodium include salt used in cooking and at the table, seasoning blends (garlic salt, Adobo, season salt, etc.) canned soups, canned vegetables containing salt, luncheon meats including turkey, ham, bologna, and salami, prepared foods, fast foods, soy sauce, ketchup, and salad dressings. On food labels, compare milligrams of sodium to calories per serving. Sodium should be less than or equal to calories per serving.
Eat a moderate amount of high protein animal food: 3-5 oz per meal (preferably lean cuts of meat, fish, and poultry) Avoid saturated fats such as butter, cheese, fried foods, fatty cuts of red meat, egg yolks, and poultry skin. Increase unsaturated fat intake, including olive oil, canola oil, peanut butter, avocadoes, fish and nuts. Eat low-fat desserts. Increase intake of fruits and vegetables. No potassium or phosphorus restriction necessary. Monitor fluid intake, which includes all fluids and foods that are liquid at room temperature. Fluid management in nephrotic syndrome is tenuous, especially during an acute flare.
Complications
Venous thrombosis: due to leak of anti-thrombin 3, which helps prevent thrombosis. This often occurs in the renal veins. Treatment is with oral anticoagulants (not heparin as heparin acts via anti-thrombin 3 which is lost in the proteinuria so it will be ineffective.)
Infection:
due
to
leakage
of
immunoglobulins,
encapsulated
bacteria
such
as Haemophilus
influenzae and Streptococcus pneumoniae can cause infection.
Acute renal failure is due to hypovolemia. Despite the excess of fluid in the tissues, there is less fluid in the vasculature. Decreased blood flow to the kidneys causes them to shutdown. Thus it is a tricky task to get rid of excess fluid in the body while maintaining circulatory euvolemia.
Pulmonary edema: again due to fluid leak, sometimes it leaks into lungs causing hypoxia and dyspnoea.
Growth retardation: does not occur in MCNS.It occurs in cases of relapses or resistance to therapy. Causes of growth retardation are protein deficiency from the loss of protein in urine, anorexia (reduced protein intake), and steroid therapy (catabolism).
Vitamin D deficiency can occur. Thyroxine is reduced due to decreased thyroid binding globulin.
Microcytic hypochromic anaemia is typical. It is iron-therapy resistant.
Hypocalcemia can occur as a result of nephrotic syndrome. It may be significant enough to cause tetany.
Cushing Syndrome
Prognosis
The prognosis depends on the cause of nephrotic syndrome. It is usually good in children, because minimal change disease responds very well to steroids and does not cause chronic renal failure. However other causes such as focal segmental glomerulosclerosisfrequently lead to end stage renal disease. Factors associated with a poorer prognosis in these cases include level of proteinuria, blood pressure control and kidney function (GFR)
You might also like
- OSCE in PediatricsDocument267 pagesOSCE in PediatricsKhiladi86% (7)
- Assessment of The Critically Ill PatientDocument5 pagesAssessment of The Critically Ill PatientCris John RicoNo ratings yet
- Rutger's PANRE and PANCE Practice Questions 2 of 2Document38 pagesRutger's PANRE and PANCE Practice Questions 2 of 2nubianlocks100% (3)
- Food Science & NutritionDocument18 pagesFood Science & NutritionShelly0% (1)
- Gastro Intestinal Bleeding DR - muayAD ABASSDocument59 pagesGastro Intestinal Bleeding DR - muayAD ABASSMAFADHELNo ratings yet
- Nephrotic SyndromeDocument34 pagesNephrotic SyndromeksanjdsaNo ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- Acute and Chronic Renal FailureDocument7 pagesAcute and Chronic Renal FailureSuliman GarallehNo ratings yet
- Science, Technology, and SocietyDocument27 pagesScience, Technology, and SocietyAnjhiene CambaNo ratings yet
- General Biology I M6Document19 pagesGeneral Biology I M6Anjhiene CambaNo ratings yet
- Nephrotic Syndrome Msn-3Document12 pagesNephrotic Syndrome Msn-3Bibi Renu100% (3)
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Congestive Cardiac Failure by NeetaDocument26 pagesCongestive Cardiac Failure by NeetaNeeta AnandaNo ratings yet
- Gen Bio1 Module 9Document23 pagesGen Bio1 Module 9Anjhiene Camba100% (2)
- Mitral Stenosis PresentationDocument84 pagesMitral Stenosis PresentationStawan Chougule100% (2)
- 16 Martie - Curs BPOC - SlideDocument95 pages16 Martie - Curs BPOC - Slidejonah1024No ratings yet
- Acute Renal FailureDocument17 pagesAcute Renal FailureDina Rasmita100% (1)
- What Is NeuropathyDocument4 pagesWhat Is NeuropathyLord Pozak MillerNo ratings yet
- Epidemiology of Non Communicable DiseaseDocument16 pagesEpidemiology of Non Communicable DiseaseAparna AbyNo ratings yet
- 100MCQsinTropicalMedicine (PDF Library)Document76 pages100MCQsinTropicalMedicine (PDF Library)Abdalla ShibailiNo ratings yet
- Acute Tubular NecrosisDocument15 pagesAcute Tubular NecrosisDeepak patelNo ratings yet
- General Biology I M4Document24 pagesGeneral Biology I M4Anjhiene CambaNo ratings yet
- Care Plan On Nephrotic SyndromeDocument31 pagesCare Plan On Nephrotic Syndromepriyanka bhavsar100% (1)
- Kahoots 8 - Renal Physiology PDFDocument3 pagesKahoots 8 - Renal Physiology PDFJoshua LanzonNo ratings yet
- Guillan Barre Syndrome FinalDocument16 pagesGuillan Barre Syndrome FinalAswathy RCNo ratings yet
- Teaching Arts in The Elemntary Module 1Document31 pagesTeaching Arts in The Elemntary Module 1Anjhiene Camba100% (1)
- Gen Bio1 - Module 13Document19 pagesGen Bio1 - Module 13Anjhiene CambaNo ratings yet
- Cirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDocument21 pagesCirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDan ChicinasNo ratings yet
- Geriatric MCQDocument9 pagesGeriatric MCQVinit Choudhary100% (1)
- Hemodiafiltration Kuhlmann PDFDocument31 pagesHemodiafiltration Kuhlmann PDFDavid SantosoNo ratings yet
- Menigitis EncephalitisDocument63 pagesMenigitis EncephalitisHussain AzharNo ratings yet
- Adrenal CrisisDocument6 pagesAdrenal CrisisSteven SetioNo ratings yet
- Soal Kidney CompiledDocument28 pagesSoal Kidney Compiledstella pangestika100% (1)
- General Biology I M7Document19 pagesGeneral Biology I M7Anjhiene CambaNo ratings yet
- GlomerulonephritisDocument58 pagesGlomerulonephritisJosa Anggi Pratama0% (1)
- Gen Bio1 Module 10Document20 pagesGen Bio1 Module 10Anjhiene CambaNo ratings yet
- Semi-Detailed Lesson Plan in Physical Science: Schools Division of Alaminos CityDocument27 pagesSemi-Detailed Lesson Plan in Physical Science: Schools Division of Alaminos CityAnjhiene CambaNo ratings yet
- Disseminated Intravascular CoagulationDocument2 pagesDisseminated Intravascular CoagulationVince100% (1)
- Proteinuria in Adults - A Diagnostic Approach - September 15, 2000 - American Family PhysicianDocument7 pagesProteinuria in Adults - A Diagnostic Approach - September 15, 2000 - American Family PhysicianSi vis pacem...100% (1)
- Glomerulonephritis: Nameesha Natasha Naidu 20130105Document26 pagesGlomerulonephritis: Nameesha Natasha Naidu 20130105AliMalikNo ratings yet
- Nephrotic SyndromeeDocument28 pagesNephrotic SyndromeeRiteka SinghNo ratings yet
- Nursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIDocument10 pagesNursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIanamika sharmaNo ratings yet
- A Case Report of Classical Hodgkin's Lymphoma Presented With Anemia of Chronic Disease As Microcytic Hypochromic TypeDocument3 pagesA Case Report of Classical Hodgkin's Lymphoma Presented With Anemia of Chronic Disease As Microcytic Hypochromic TypeIOSRjournalNo ratings yet
- Definition of HypertentionDocument10 pagesDefinition of HypertentionTSetiawan TSetiawanNo ratings yet
- Case Presentation: by Michael ArmstrongDocument21 pagesCase Presentation: by Michael ArmstrongWirawan Amirul BahriNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryAtif Gazali100% (1)
- Exudative Pleural Effusions - UpToDateDocument2 pagesExudative Pleural Effusions - UpToDateAsif IqbalNo ratings yet
- Pathological Changes of DM - 2023Document53 pagesPathological Changes of DM - 2023Visura PrabodNo ratings yet
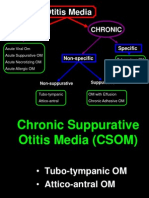
- CSOM TreatmentDocument21 pagesCSOM TreatmentSarwinder SinghNo ratings yet
- Nephrotic and Nephritic SyndromesDocument27 pagesNephrotic and Nephritic SyndromesJoshua Smith100% (1)
- Case Presentation On MalariaDocument13 pagesCase Presentation On Malarialavate amol bhimraoNo ratings yet
- Case Presentation On Peptic UlcerDocument62 pagesCase Presentation On Peptic Ulcernot your medz duran100% (1)
- Addison's DiseaseDocument9 pagesAddison's Diseaseash ashNo ratings yet
- Case Presentation - GASTRODocument46 pagesCase Presentation - GASTROalidudeNo ratings yet
- GLOMERULONEPHRITIS (Bright's Disease)Document8 pagesGLOMERULONEPHRITIS (Bright's Disease)Anjitha K. JNo ratings yet
- Cva Case PDFDocument39 pagesCva Case PDFEmsy Ni ThelayNo ratings yet
- Chest Pain.Document53 pagesChest Pain.Shimmering MoonNo ratings yet
- Leg UlcersDocument22 pagesLeg UlcersMarera DomnicNo ratings yet
- Acute Renal Failure & Chronic Renal FailureDocument38 pagesAcute Renal Failure & Chronic Renal FailureArti GondNo ratings yet
- Crystal Induced Arthropathies: BY: DR Mehrunnisa Umar Assisstant Profesor Department of MedicineDocument25 pagesCrystal Induced Arthropathies: BY: DR Mehrunnisa Umar Assisstant Profesor Department of MedicinedrusmanjamilhcmdNo ratings yet
- AnaemiaDocument4 pagesAnaemiaHarinash RaoNo ratings yet
- NephritisDocument21 pagesNephritisruchikaNo ratings yet
- Hypertensive NephrosclerosissDocument38 pagesHypertensive NephrosclerosissDhanya RaghuNo ratings yet
- Nephrotic SyndromeDocument31 pagesNephrotic Syndromedrhananfathy100% (1)
- NIV Fs 9108147 e 1911 1 PDFDocument4 pagesNIV Fs 9108147 e 1911 1 PDFliuchenshitaoNo ratings yet
- Case Presentation: DR - Anbalagan II ND Year MEMDocument20 pagesCase Presentation: DR - Anbalagan II ND Year MEMDr mahi sNo ratings yet
- Case Presentation - Cholecystitis - DR - RikiDocument14 pagesCase Presentation - Cholecystitis - DR - RikiLevina AudreyNo ratings yet
- Goitre: Dr. Sandhya Gupta Assistant Professor General SurgeryDocument59 pagesGoitre: Dr. Sandhya Gupta Assistant Professor General SurgerySandhya guptaNo ratings yet
- Nursing Process 3Document10 pagesNursing Process 3Shubhra Sheoran100% (1)
- Ugib &lgibDocument41 pagesUgib &lgibDawex IsraelNo ratings yet
- Pooja FinalDocument35 pagesPooja FinalSagar ChiplunkarNo ratings yet
- Practice Teaching On Anemia: Presented By: Mr. Hari Singh Nagar M. SC Nursing 1 YearDocument44 pagesPractice Teaching On Anemia: Presented By: Mr. Hari Singh Nagar M. SC Nursing 1 YearSundarNo ratings yet
- Anatomy of The KidneysDocument7 pagesAnatomy of The KidneysSanthu SuNo ratings yet
- An Introduction To AnaemiaDocument27 pagesAn Introduction To Anaemiaمجاهد إسماعيل حسن حسينNo ratings yet
- Mitral RegurgitationDocument9 pagesMitral RegurgitationNefvi Desqi AndrianiNo ratings yet
- Bone Marrow AspirationDocument7 pagesBone Marrow Aspirationश्रीकृष्ण हेङ्गजूNo ratings yet
- Nephrotic SyndromeDocument23 pagesNephrotic SyndromeDivina Francia JovenNo ratings yet
- Nephrotic SyndromeDocument8 pagesNephrotic SyndromeKanmani AniNo ratings yet
- GlomerulonephritisDocument4 pagesGlomerulonephritisEmilene ZaragozaNo ratings yet
- Q3 - WEEK 3 - LAS-3-Timeline of Evolution ThoughtDocument1 pageQ3 - WEEK 3 - LAS-3-Timeline of Evolution ThoughtAnjhiene CambaNo ratings yet
- Q3 WEEK 3 LAS-1-Reproductive IsolationDocument1 pageQ3 WEEK 3 LAS-1-Reproductive IsolationAnjhiene CambaNo ratings yet
- Q3 - WEEK 8 - LAS-2-Cladistics-Shared Derived CharacterDocument2 pagesQ3 - WEEK 8 - LAS-2-Cladistics-Shared Derived CharacterAnjhiene CambaNo ratings yet
- Q3 - WEEK 8 - LAS-3-Cladogram-Infer Evolutionary RelatednessDocument1 pageQ3 - WEEK 8 - LAS-3-Cladogram-Infer Evolutionary RelatednessAnjhiene CambaNo ratings yet
- Q3 - WEEK 7 - LAS-1-The Linnean System of ClassificationDocument1 pageQ3 - WEEK 7 - LAS-1-The Linnean System of ClassificationAnjhiene CambaNo ratings yet
- Q3 - WEEK 7 - LAS-3-Dichotomous Keys For IdentificationDocument1 pageQ3 - WEEK 7 - LAS-3-Dichotomous Keys For IdentificationAnjhiene CambaNo ratings yet
- Q3 - WEEK 3 - LAS-2-SpeciationDocument1 pageQ3 - WEEK 3 - LAS-2-SpeciationAnjhiene CambaNo ratings yet
- Q3 - WEEK 2 - LAS-3-Mechanism-of-change-in-populationsDocument2 pagesQ3 - WEEK 2 - LAS-3-Mechanism-of-change-in-populationsAnjhiene CambaNo ratings yet
- Teaching Profession Module 1Document15 pagesTeaching Profession Module 1Anjhiene CambaNo ratings yet
- Q3 - WEEK 5 - LAS-3-Infering Relationships From Evidences of Evolution-FossilsDocument2 pagesQ3 - WEEK 5 - LAS-3-Infering Relationships From Evidences of Evolution-FossilsAnjhiene CambaNo ratings yet
- Gen Bio Quiz 3Document3 pagesGen Bio Quiz 3Anjhiene CambaNo ratings yet
- Q3 - WEEK 7 - LAS-2-Classification of Organism Using Hierarchal SystemDocument2 pagesQ3 - WEEK 7 - LAS-2-Classification of Organism Using Hierarchal SystemAnjhiene CambaNo ratings yet
- Assessment of Student Learning Ii: Beed Module 2Document7 pagesAssessment of Student Learning Ii: Beed Module 2Anjhiene CambaNo ratings yet
- Q3 - WEEK 6 - LAS-1-Multiple Lines of EvidenceDocument2 pagesQ3 - WEEK 6 - LAS-1-Multiple Lines of EvidenceAnjhiene CambaNo ratings yet
- Social Dimensions Module 1Document14 pagesSocial Dimensions Module 1Anjhiene CambaNo ratings yet
- General Biology 1 First QuarterDocument10 pagesGeneral Biology 1 First QuarterAnjhiene CambaNo ratings yet
- Assessment of Student Learning Ii: Beed Module 2Document8 pagesAssessment of Student Learning Ii: Beed Module 2Anjhiene CambaNo ratings yet
- Letter of Application GPC 1111111Document4 pagesLetter of Application GPC 1111111Anjhiene CambaNo ratings yet
- PDF Module 2Document8 pagesPDF Module 2Anjhiene CambaNo ratings yet
- Minimal Change Disease Following The P Fizer-Biontech Covid-19 VaccineDocument4 pagesMinimal Change Disease Following The P Fizer-Biontech Covid-19 VaccineGerardo de Gyves AvilaNo ratings yet
- 1 Childhood Nephrotic Syndrome - Diagnosis and ManagementDocument52 pages1 Childhood Nephrotic Syndrome - Diagnosis and ManagementThana Balan100% (1)
- Nephritis NephrosisDocument43 pagesNephritis NephrosisE=MC2No ratings yet
- 04 NephrologyDocument19 pages04 NephrologyeuncieNo ratings yet
- Nephrotic Syndrome PathophysiologyDocument1 pageNephrotic Syndrome PathophysiologyKrisianne Mae Lorenzo FranciscoNo ratings yet
- A Treatise On Advance Acupressure/Acupuncture (Part Xiii) - Kidney & Urinary Tract Disorders Efje Eùeeveg EâceefcekeâeDocument19 pagesA Treatise On Advance Acupressure/Acupuncture (Part Xiii) - Kidney & Urinary Tract Disorders Efje Eùeeveg EâceefcekeâeParvathy ShekharNo ratings yet
- Case Presentation: Muhammad Ali Bin Abdul Razak Wan Ahmad Syazani Bin Mohamed Nadiah Mohd NasirDocument63 pagesCase Presentation: Muhammad Ali Bin Abdul Razak Wan Ahmad Syazani Bin Mohamed Nadiah Mohd NasirarbyjamesNo ratings yet
- Mediated Disorders: (Type Icrgn) Anti-Glomerular Basement Membrane Antibody Ular Basement Membrane AntibodyDocument1 pageMediated Disorders: (Type Icrgn) Anti-Glomerular Basement Membrane Antibody Ular Basement Membrane AntibodyDian Putri NingsihNo ratings yet
- Astra-Module-38 Pedia NephroDocument20 pagesAstra-Module-38 Pedia NephroenzocruzinNo ratings yet
- C5. Renal Disorders (Nephrotic S. - Renal F.)Document44 pagesC5. Renal Disorders (Nephrotic S. - Renal F.)coco brillqnteNo ratings yet
- 419 FullDocument6 pages419 Fullmarkwat21No ratings yet
- Nephrotic Syndrome: By: Yeni Ayu Prihastuti Moderator: DR. Dr. Hani Susianti, SP - PK (K)Document42 pagesNephrotic Syndrome: By: Yeni Ayu Prihastuti Moderator: DR. Dr. Hani Susianti, SP - PK (K)yeniNo ratings yet
- Nephrotic Syndrome in AdultDocument53 pagesNephrotic Syndrome in AdultAnna Althafunnisa100% (1)
- Urinalysis OSCE GuideDocument5 pagesUrinalysis OSCE GuideSSNo ratings yet
- Paper 2 Mbbs NtruhsDocument28 pagesPaper 2 Mbbs NtruhsImhotep AsclepiusNo ratings yet
- Proteinuria in Adults - A Diagnostic Approach - AAFPDocument12 pagesProteinuria in Adults - A Diagnostic Approach - AAFPXeric CedoNo ratings yet
- NSAIDs - Acute Kidney Injury (Acute Renal Failure) - UpToDateDocument14 pagesNSAIDs - Acute Kidney Injury (Acute Renal Failure) - UpToDateLucía Aldhaiz Lazo CusihuallpaNo ratings yet
- Glomerular Diseases in Pregnancy - Kidney (2023)Document18 pagesGlomerular Diseases in Pregnancy - Kidney (2023)cheve glzNo ratings yet
- Nephrotic SyndromeDocument49 pagesNephrotic SyndromeAMA237No ratings yet
- Renal Pathology - 012) Nephrotic Syndrome (Notes)Document10 pagesRenal Pathology - 012) Nephrotic Syndrome (Notes)hasanatiya41No ratings yet