Professional Documents
Culture Documents
Overview of BPfA - Women and Health - C
Uploaded by
European Institute for Gender EqualityOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Overview of BPfA - Women and Health - C
Uploaded by
European Institute for Gender EqualityCopyright:
Available Formats
Women and Health (C)
Women and Health (C)
In the Beijing Declaration and Platform for Action for Equality, Development and Peace (BPfA) 19951, health is defined as a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. Womens health involves their emotional, social and physical wellbeing and is determined by the social, political and economic context of their lives, as well as by biology. A major barrier for women to the achievement of the highest attainable standard of health is inequality, both between men and women and among women in different geographical regions, social classes and indigenous and ethnic groups. Women have different and unequal access to and use of basic health resources. Furthermore, women are subject to particular health risks due to inadequate responsiveness and lack of services to meet health needs related to sexuality and reproduction. Women are affected by many of the same health conditions as men, but women experience them differently. The prevalence among women of poverty and economic dependence, their experience of violence, negative attitudes towards women and girls, racial and other forms of discrimination, the limited power many women have over their sexual and reproductive lives and lack of influence in decision-making are social realities which have an adverse impact on their health. Sexual and gender-based violence, including physical and psychological abuse, trafficking in women and girls and other forms of abuse and sexual exploitation place girls and women at high risk of physical and mental trauma, disease and unwanted pregnancy. HIV/AIDS and other sexually transmitted diseases, the transmission of which is sometimes a consequence of sexual violence, are having a devastating effect on womens health, particularly the health of adolescent girls and young women. With the increase in life expectancy and the growing number of older women, their health concerns require particular attention. Statistical data on health are often not systematically collected, disaggregated and analysed by age, sex and socio-economic status and by established demographic criteria used to serve the interests and solve the problems of subgroups, with particular emphasis on the vulnerable and marginalised and other relevant variables. Relatively little is known about how social and economic factors affect the health of girls and women of all ages, about the provision of health services to girls and women and the patterns of their use of such services, and about the value of disease prevention and health promotion programmes for women. In order to address these problems, the following strategic objectives were set and agreed to be implemented by the national governments.
The strategic objectives
C.1 Increase womens access throughout the life cycle to appropriate, affordable and quality health care, information and related services C.2 Strengthen preventive programmes that promote womens health C.3 Undertake gender-sensitive initiatives that address sexually transmitted diseases, HIV/AIDS, and sexual and reproductive health issues C.4 Promote research and disseminate information on womens health C.5 Increase resources and monitor followup for womens health
Beijing: an overview of the Beijing Indicators
Women and Health (C)
Indicators
In 2006, the Austrian Presidency undertook to focus on indicators for measuring progress on womens health since gender-based data are the prerequisite for gender-related health policies and prepared a report2 to propose indicators concerning womens health. In developing the indicators for womens health, the Austrian Presidency considered the communication from the Commission A Roadmap for equality between women and men, 200620103 which established that Women and men are confronted with specific health risks, diseases, issues and practices impacting their health. Medical research and many safety and health standards relate more to men and male-dominated work areas. Knowledge in this field should be improved and statistics and indicators further developed. Social, health and care services should be modernised with a view to improving their accessibility, quality and responsiveness to the new and specific needs of women and men. The number of indicators was restricted to three. The indicators on womens health proposed by the Austrian Presidency and adopted4 by the Council of the European Union in 2006 are: healthy life years; access to healthcare; and cardiovascular diseases.
Indicator C1
Name: Healthy Life Years Concept: This indicator, the Healthy Life Years (also called disability-free life expectancy) measures the number of remaining years that a person of a certain age is still expected to live without disability. Healthy Life Years (HLY) is a solid indicator to monitor health as a productivity/economic factor. HLY introduces the concept of quality of life into life expectancy. It is used to distinguish between
years of life free of any activity limitation and years experienced with at least one activity limitation. The emphasis is not exclusively on the length of life, as is the case for life expectancy, but also on the quality of life. HLY is a functional health status measurement increasingly used to complement the conventional life expectancy measures. Chronic disease, frailty, and disability tend to become more prevalent at older ages, so that a population with a higher life expectancy may not be healthier. Indeed, a major question within an ageing population is whether increases in life expectancy will be associated with a greater or lesser proportion of the future population spending their years living with disability. If HLY is increasing more rapidly than life expectancy in a population, then not only people are living longer, they are also living a greater portion of their lives free of disability. The two components of the calculation of the HLY in the EU are the mortality tables and the self-perceived disability assessed by health surveys. Life tables which give mortality data for calculating life expectancy are fully available as a demographic long-term series based on the standard procedures of causes of death registration harmonised at EU level. To provide an overview of the situation, the following two HLY indicators were used in the report by the Austrian Presidency: healthylifeyearsinabsolutevalueatbirth percentageoflifeexpectancy Data source: The calculation of the indicator is based on two data sources5: Eurostat demographic data on mortality and the European Union Statistics on Income and Living Conditions (EU-SILC). The self-perceived disability is based on the EU-SILC survey, where an unhealthy condition is defined by the limitation in the activities people usually do because of health problems at least for the last six months and this assessment is based on the question: For at least the past six
Beijing: an overview of the Beijing Indicators
Women and Health (C)
months, to what extent have you been limited because of a health problem in activities people usually do? Would you say you have been: strongly limited/limited/not limited at all?. Published: Data are available in the Eurostat online database (hlth_hlye: Structural indicators on health6). Notes: The data cover all EU Member States: the oldest data are available from 1995 and for all Member States since 2005. The data are updated annually. The HLY indicator is calculated using the same method7 (Sullivans) for all countries. However, the comparability of the data across countries may be limited since the question on the existence of disabilities can be interpreted differently between countries. Moreover, breaks in series, caused by the change in the data source for calculating the prevalence of disability in 2004, limits comparability. From 1995 to 2001, the EU-ECHP (European Community Household Panel) results were used and since 2004 the EU-SILC (Statistics on Income and Living Conditions) results have been used. The way this question was implemented by the Member States, however, hampers cross-country comparisons for the data up to 2008. Therefore, before 2008, the results should be used with caution and only the evolution in time for each country should be considered. The overall accuracy of HLY is considered good. However, the fact that institutional households are not covered by the EU-SILC raises a potential problem of representativeness especially because these persons are particularly exposed to health problems.
Indicator C2
Name: Access to health care (unmet demand) Concept: The access to healthcare indicator measures the share of women and men in the
total population aged 16 and over who needed medical examination or treatment during the last 12 months but did not receive it, and the reasons for this unmet need. Social protection systems must ensure that people who need medical or social care can get it regardless of their income or wealth and that the cost of such care does not cause poverty to the care recipients or their relatives. Access to healthcare implies that ability to pay is not a precondition to receiving care and that the need for care does not lead to impoverishment. Consistent increases in expenditure, coupled with increasing population coverage over the years, have allowed Member States to generally ensure all residents have access to basic healthcare as well as ensuring that the need for healthcare is not a major cause of poverty and financial dependence of patients and their relatives. Despite that, there remain important access inequities to address. Access barriers include lack of coverage of certain types of care, high individual financial costs of care, geographical disparities of supply, waiting times and lack of information. Limiting access can save costs but if too high can result in belated and more costly treatment. Moreover, countries identify different experiences of care use across socio-economic groups (e.g. richer households make more use of preventive and specialist care than poorer households who make more use of emergency hospital care). During the preparation of the Austrian Presidency report in 2006, data were not available. Data source: The calculation of the indicator is based on the European Union Statistics on Income and Living Conditions (EU-SILC) survey health module8. The questions on unmet needs of healthcare refer to the situation during the 12 months preceding the survey and are based on the respondents own assessment of whether he or she needed a medical
Beijing: an overview of the Beijing Indicators
Women and Health (C)
examination or treatment, but did not have one and main reason for not having a medical examination or treatment, while needed. The main reasons are the following: 1. Could not afford to (too expensive); 2. Waiting list; 3. Could not take time because of work, care for children or for others; 4. Too far to travel/no means of transportation; 5. Fear of doctor/hospitals/examination/ treatment; 6. Wanted to wait and see if problem got better on its own; 7. Did not know any good doctor; 8. Other reasons. Published: Data are available in the Eurostat online database (hlth_silc_08: People with unmet needs for medical examination by sex, age, reason and income quintile (%)9). Notes: The data cover all EU Member States: the oldest data are available from 2004 and for all Member States since 2007. The data are updated annually. The indicator relies on self-assessment of the need for care and, therefore, has a subjective dimension. Until 2008, the implementation of health questions in EU-SILC was not fully harmonised and, thus, the comparability of the results is limited. New guidelines should improve comparability between countries from 2008.
Indicator C3
Name: Cardio-vascular diseases Concept: Cardiovascular diseases indicator measures the share of deaths of women and men caused by cardiovascular diseases (CVD) (coronary heart disease (CHD), stroke, and other CVD). According to the Austrian Presidency report, diseases of the heart and circulatory system
(cardiovascular disease or CVD) are the main cause of death in the European Union and the main forms of CVD are coronary heart disease (CHD) and stroke. Furthermore, the CVD is the main cause of death for women. The incidence of coronary heart disease in women increases dramatically in middle age, which has led to the speculation that menopause marks the end of a protective effect of ovarian hormones on cardiovascular disease. CHD results in many premature deaths and since clinical care in CVDs is costly and prolonged, it is also a major economic burden in Europe. Factors that have been identified as contributors to coronary heart disease for women include cholesterol, smoking, high blood pressure, obesity, physical inactivity, hormonal changes and diabetes mellitus. To these classical risk factors we can add others if we incorporate the gender perspective to analyse the risk factors, such as socio-economic condition, links with health services, subjective construction of the illness, insertion to the labour market or interconnection among the different areas of work, personal interests and family life. Data source: The calculation of this indicator is based on the Causes of death data10 coordinated by Eurostat. Causes of death are classified by the 65 causes on the European shortlist11 of causes of death. This shortlist is based on the International Statistical Classification of Diseases and Related Health Problems (ICD)12. According to the Austrian Presidency report, the causes of death because of cardiovascular diseases should be defined as the following: coronaryheartdisease(CHD):ischaemic heart diseases according to European shortlist (indicator I20I25 in the table); stroke:cerebrovasculardiseasesaccording to European shortlist (indicator I60 I69 in the table);
Beijing: an overview of the Beijing Indicators
Women and Health (C)
otherCVDsuchasrheumaticfeverand rheumatic heart disease, diseases of the circulatory system, ischemic heart diseases, arterial hypertension: diseases of the circulatory system (indicator I in the table) minus CHD and stroke (indicator I20I25 and indicator I60I69 in the table). Published: Data are available in the Eurostat online database (hlth_cd_anr: Causes of death Absolute number (Annual data)13). Notes: The data cover all EU Member States: the oldest data are available from 1994 (but not for all Member States). The data are updated annually. Inaccuracies may be due to errors with the issue of the death certificate, errors in the medical diagnosis, in the selection of the main cause of death or in the coding of the cause of death. Sometimes there is ambiguity in the cause of death. Indeed, there is criticism that the coding of only one illness as a cause of death appears more and more unrealistic. For the majority of the deceased of 65 years and older, the selection of just one cause of death may be somewhat misleading as they often have had several chronic diseases that concurrently led to death. For this reason, some Member States have started to consider multiple-cause coding. Although definitions are harmonised, the statistics may not be fully comparable as classifications may vary when the cause of death is multiple or difficult to evaluate and because of different notification procedures. The coverage of residents dying abroad can also affect the comparability among countries (national practices concerning the registration of residents dying abroad and domestic deaths of non-residents are far from harmonised across Member States).
More information
Policy documents
Beijing Declaration and Platform for Action 1995 (http://www.un.org/womenwatch/daw/beijing/ pdf/BDPfA%20E.pdf ). Council of the European Union, Draft Council conclusions Review of the implementation by Member States and the EU institutions of the Beijing Platform for Action Beijing + 15: A review of progress, Brussels, 10 November 2009 (http:// register.consilium.europa.eu/pdf/en/09/st15/ st15487-ad01.en09.pdf ). Council of the European Union, Draft Council conclusions on the review of the implementation by the Member States and the EU institutions of the Beijing Platform for Action, Brussels, 18 May 2006 (http://register.consilium.europa.eu/pdf/en/06/ st09/st09468.en06.pdf ). Council of the European Union, Review of the implementation by the Member States and the EU institutions of the Beijing Platform for Action, Report by the Austrian Presidency Indicators concerning womens health, Brussels, 18 May 2006 (http://register.consilium.europa.eu/pdf/en/06/ st09/st09468-ad01.en06.pdf ). Council of the European Union, Press release, 2733rd Council meeting, Luxembourg, 1 and 2 June 2006 (http://www.consilium.europa.eu/uedocs/cms_ data/docs/pressdata/en/lsa/89830.pdf ). The European Commissions Strategy for equality between women and men 20102015 (COM(2010) 491 final of 21 September 2010) (http://eur-lex.europa.eu/LexUriServ/LexUriServ. do?uri=CELEX:52010DC0491:EN:PDF). European Commission, Communication from the Commission Europe 2020 A strategy for smart, sustainable and inclusive growth, Brussels, 3 March 2010 (http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2010:2020:FIN:EN:PDF). European Commission, Communication from the Commission A Strengthened Commitment to
Beijing: an overview of the Beijing Indicators
Women and Health (C)
Equality between Women and Men A Womens Charter, Brussels, 5 March 2010 (http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2010: 0078:FIN:EN:PDF).
Reports
Eurostat, The Social Situation in the European Union 2009, European Commission. DirectorateGeneral for Employment, Social Affairs and Equal Opportunities Unit E.1., Eurostat Unit F.4. European Union, 2010 (http://epp.eurostat. ec.europa.eu/cache/ITY_OFFPUB/KE-AG-10-001/ EN/KE-AG-10-001-EN.PDF). Eurostat Statistical books, Measuring progress towards a more sustainable Europe 2007 monitoring report of the EU sustainable development strategy, European Communities, 2007 (http://ec.europa.eu/sustainable/docs/ estat_2007_sds_en.pdf ). OECD (2010), Health at a Glance Europe 2010, OECD Publishing (http://ec.europa.eu/health/ reports/docs/health_glance_en.pdf ). Baert, K., de Norre, B., Perception of health and access to health care in the EU-25 in 2007, Eurostat, Statistics in Focus, 24/2009 (http://epp.eurostat.
ec.europa.eu/cache/ITY_OFFPUB/KS-SF-09-024/ EN/KS-SF-09-024-EN.PDF). Faculty of Medicine Carl Gustav Carus Research Association, Public Health Saxony and Saxony-Anhalt, Data and information on womens health in the European Union, Directorate-General for Health & Consumers, Technische Universitt Dresden, Dresden, Germany, European Communities, 2009 (http://ec.europa.eu/health/population_groups/ docs/women_report_en.pdf ). Eurostat Statistical books, Health statistics Atlas on mortality in the European Union, European Communities, 2009 (http://epp.eurostat. ec.europa.eu/cache/ITY_OFFPUB/KS-30-08-357/ EN/KS-30-08-357-EN.PDF). The State of Mens Health in Europe 2011, European Commission,Directorate-GeneralforHealth&Consumers (http://ec.europa.eu/health/population_groups/ docs/men_health_extended_en.pdf ). Engender, Improving gender equality in health (http://engender.eurohealth.ie). Access to healthcare and long-term care Equal for Women and Men?, European Commission, Directorate-General for Employment, Social Affair and Equal Opportunities (http://ec.europa.eu/ social/BlobServlet?docId=5590&langId=en).
Notes
1. Beijing Declaration and Platform for Action 1995, p. 34 (http://www.un.org/womenwatch/ daw/beijing/pdf/BDPfA%20E.pdf ). The report prepared by Austrian EU Presidency is available online (http://register.consilium.europa. eu/pdf/en/06/st09/st09468-ad01.en06.pdf ). Communication from the Commission A Roadmap for equality between women and men 20062010 (COM (2006) 92 final) (http:// eur-lex.europa.eu/LexUriServ/LexUriServ.do?u ri=COM:2006:0092:FIN:EN:PDF). Council of the European Union, Press release, 2733rd Council Meeting, Luxembourg, 1 and 2 June 2006 (http://www.consilium.europa.eu/uedocs/ cms_data/docs/pressdata/en/lsa/89830.pdf ). 5. Structural indicators on health, Eurostat metadata (http://epp.eurostat.ec.europa.eu/ cache/ITY_SDDS/EN/hlth_hlye_esms.htm). Table hlth_hlye: Structural indicators on health is available online (http://appsso.eurostat.ec.europa. eu/nui/show.do?dataset=hlth_hlye&lang=en). Healthy Life Years Expectancy disability-free life expectancy DFLE Method (http:// epp.eurostat.ec.europa.eu/cache/ITY_SDDS/ Annexes/hlth_hlye_esms_an1.pdf ). SILC variables on healthcare (http://epp.eurostat. ec.europa.eu/cache/ITY_SDDS/Annexes/hlth_ care_silc_esms_an1.pdf ). Table hlth_silc_08: People with unmet needs for medical examination by sex, age, reason
2.
6.
3.
7.
8.
4.
9.
Beijing: an overview of the Beijing Indicators
Women and Health (C)
10.
11.
and income quintile (%) is available online (http://appsso.eurostat.ec.europa.eu/nui/show. do?dataset=hlth_silc_08&lang=en). Causes of death, Eurostat metadata (http://epp. eurostat.ec.europa.eu/cache/ITY_SDDS/EN/ hlth_cdeath_esms.htm). Metadata, European Shortlist for Causes of Death, 1998 (http://ec.europa.eu/ eurostat/ramon/nomenclatures/index.
12. 13.
cfm?TargetUrl=LST_NOM_DTL&StrNom=COD_1 998&StrLanguageCode=EN&IntPcKey=&StrLayo utCode=HIERARCHIC). International Classification of Diseases (ICD) (http://www.who.int/classifications/icd/en/). Table hlth_cd_anr: Causes of death Absolute number (Annual data) is available online (http://appsso.eurostat.ec.europa.eu/nui/show. do?dataset=hlth_cd_anr&lang=en).
Beijing: an overview of the Beijing Indicators
You might also like
- JTN - Articles On Gender Gap in Pensions in The European Union PDFDocument28 pagesJTN - Articles On Gender Gap in Pensions in The European Union PDFEuropean Institute for Gender EqualityNo ratings yet
- Gender Equality Index 2015Document194 pagesGender Equality Index 2015Marcello D'AmicoNo ratings yet
- Mh0215178enn PDFDocument128 pagesMh0215178enn PDFEuropean Institute for Gender EqualityNo ratings yet
- Mh0215178enn PDFDocument128 pagesMh0215178enn PDFEuropean Institute for Gender EqualityNo ratings yet
- Gender Equality Index 2015Document194 pagesGender Equality Index 2015Marcello D'AmicoNo ratings yet
- Mh0215178enn PDFDocument128 pagesMh0215178enn PDFEuropean Institute for Gender EqualityNo ratings yet
- JTN - Articles On Gender Gap in Pensions in The European Union PDFDocument28 pagesJTN - Articles On Gender Gap in Pensions in The European Union PDFEuropean Institute for Gender EqualityNo ratings yet
- Mh0215178enn PDFDocument128 pagesMh0215178enn PDFEuropean Institute for Gender EqualityNo ratings yet
- Eige - Caar 2014-Final - 15062015 PDFDocument85 pagesEige - Caar 2014-Final - 15062015 PDFEuropean Institute for Gender EqualityNo ratings yet
- K Mh0415022enc PDFDocument4 pagesK Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- Gender Equality Index 2015Document194 pagesGender Equality Index 2015Marcello D'AmicoNo ratings yet
- Mh0214932enn PDFDocument4 pagesMh0214932enn PDFEuropean Institute for Gender EqualityNo ratings yet
- Gender Equality Index 2015Document194 pagesGender Equality Index 2015Marcello D'AmicoNo ratings yet
- I Mh0415022enc PDFDocument4 pagesI Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- C Mh0415022enc PDFDocument4 pagesC Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- J Mh0415022enc PDFDocument4 pagesJ Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- G Mh0415022enc PDFDocument4 pagesG Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- F Mh0415022enc PDFDocument4 pagesF Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- MH0215093ENN Web PDFDocument113 pagesMH0215093ENN Web PDFEuropean Institute for Gender EqualityNo ratings yet
- H Mh0415022enc PDFDocument4 pagesH Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- E Mh0415022enc PDFDocument4 pagesE Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- B Mh0415022enc PDFDocument4 pagesB Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- D Mh0415022enc PDFDocument4 pagesD Mh0415022enc PDFEuropean Institute for Gender EqualityNo ratings yet
- Mh0115110enn PDFDocument12 pagesMh0115110enn PDFEuropean Institute for Gender EqualityNo ratings yet
- Mh0614061enn PDFDocument204 pagesMh0614061enn PDFEuropean Institute for Gender EqualityNo ratings yet
- EIGE Annual Report 2013 PDFDocument74 pagesEIGE Annual Report 2013 PDFEuropean Institute for Gender EqualityNo ratings yet
- MH0214669ENC Web PDFDocument26 pagesMH0214669ENC Web PDFEuropean Institute for Gender EqualityNo ratings yet
- MH0415087ENN Web PDFDocument75 pagesMH0415087ENN Web PDFEuropean Institute for Gender EqualityNo ratings yet
- Mh0114678enn Web PDFDocument93 pagesMh0114678enn Web PDFEuropean Institute for Gender EqualityNo ratings yet
- Mh0414886enn PDFDocument144 pagesMh0414886enn PDFEuropean Institute for Gender EqualityNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 12 Business Combination Pt2 PDFDocument1 page12 Business Combination Pt2 PDFRiselle Ann SanchezNo ratings yet
- RMD IntroDocument11 pagesRMD IntroFaiz Ismadi50% (2)
- Our American HeritageDocument18 pagesOur American HeritageJeremiah Nayosan0% (1)
- Lorax Truax QuestionsDocument2 pagesLorax Truax Questionsapi-264150929No ratings yet
- (U) Daily Activity Report: Marshall DistrictDocument5 pages(U) Daily Activity Report: Marshall DistrictFauquier NowNo ratings yet
- Morton/Boyer HyposubjectsDocument96 pagesMorton/Boyer HyposubjectsBen ZuckerNo ratings yet
- Near Miss ReportingDocument14 pagesNear Miss ReportingMuflihMuhammadNo ratings yet
- History One Marks Questions With AnswerDocument49 pagesHistory One Marks Questions With AnsweryasvanthmNo ratings yet
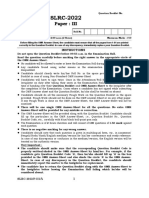
- SLRC InstPage Paper IIIDocument5 pagesSLRC InstPage Paper IIIgoviNo ratings yet
- Mẫu Kế Hoạch Digital Marketing File ExcelDocument14 pagesMẫu Kế Hoạch Digital Marketing File ExcelTrangNo ratings yet
- State of Cyber-Security in IndonesiaDocument32 pagesState of Cyber-Security in IndonesiaharisNo ratings yet
- The Game of KevukDocument8 pagesThe Game of KevukTselin NyaiNo ratings yet
- Armenia Its Present Crisis and Past History (1896)Document196 pagesArmenia Its Present Crisis and Past History (1896)George DermatisNo ratings yet
- Company Loan PolicyDocument2 pagesCompany Loan PolicyKaleem60% (5)
- 154 - 2 - Passive Voice ExercisesDocument9 pages154 - 2 - Passive Voice ExercisesSerbescuNo ratings yet
- Kickstart RequirementsDocument4 pagesKickstart Requirements9466524546No ratings yet
- Cost of Preferred Stock and Common StockDocument20 pagesCost of Preferred Stock and Common StockPrincess Marie BaldoNo ratings yet
- Safe Hospitals ManualDocument43 pagesSafe Hospitals ManualMaeDaphneYapNo ratings yet
- Regulus Astrology, Physiognomy - History and SourcesDocument85 pagesRegulus Astrology, Physiognomy - History and SourcesAntaresdeSuenios100% (3)
- Aac04 2017Document153 pagesAac04 2017Panneer SelvamNo ratings yet
- Ancient History Dot Point SummaryDocument16 pagesAncient History Dot Point SummaryBert HaplinNo ratings yet
- The Earliest Hospitals EstablishedDocument3 pagesThe Earliest Hospitals EstablishedJonnessa Marie MangilaNo ratings yet
- Enterprise Risk ManagementDocument59 pagesEnterprise Risk Managementdarshani sandamaliNo ratings yet
- Elizabeth Stevens ResumeDocument3 pagesElizabeth Stevens Resumeapi-296217953No ratings yet
- IFRS3: Business CombinationDocument56 pagesIFRS3: Business Combinationmesfin yemerNo ratings yet
- 02-7 QCS 2014Document5 pages02-7 QCS 2014Raja Ahmed Hassan0% (1)
- 03 - UndercityDocument28 pages03 - UndercityJames Bayhylle100% (1)
- BC-105 Praise & WorshipDocument41 pagesBC-105 Praise & Worshiproshan jonasNo ratings yet
- Letter ODocument17 pagesLetter ObontalampasNo ratings yet