Professional Documents
Culture Documents
Measurement of The Axial Length of Cataract Eyes by Laser Doppler Interferometry
Uploaded by
ribesnigrum82Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Measurement of The Axial Length of Cataract Eyes by Laser Doppler Interferometry
Uploaded by
ribesnigrum82Copyright:
Available Formats
Articles
Measurement of the Axial Length of Cataract Eyes by Laser Doppler Interferometry
C. K. Hitzenberger,* W. Drexler* C. Dolezal* F. Skorpik,\ M. Juchem,f A. F. Fercher* and H. D. Gnadf
Purpose. To examine the applicability of the recently developed laser Doppler interferometry technique for measuring the axial length of cataract eyes in a realistic clinical situation. To determine the performance of the instrument as a function of cataract grade. To compare the results to those of ultrasound methods. Methods. A total of 196 cataract eyes of 100 patients were examined. The axial eye length was determined by laser Doppler interferometry and by two different ultrasound techniques, the applanation technique and the immersion technique. The cataract grade was determined by a commercial instrument that measures backscattered light. Results. Laser Doppler interferometry worked very well except in the cases of the highest cataract grades (4% of the eyes of this study were not measurable because of a too-high lens density). Only 3.5% of the other eyes were not measurable because of fixation problems of the patients. The precision of laser Doppler interferometry is not influenced by the cataract grade (except the highest grade). The standard deviation of the geometric eye length is approximately 20 fim. Linear regression analysis revealed a very good correlation of laser Doppler interferometry and ultrasonic measurements, but a systematic difference was found. The eye lengths measured by laser Doppler interferometry were about 0.18 mm longer than those measured by the immersion technique and about 0.47 mm longer than those measured by the applanation technique. Conclusion. These differences are attributed to the laser Doppler interferometry results including the retinal thickness and indentation of the cornea by the applanation technique. The main advantages of the laser Doppler interferometry technique are high precision, high accuracy, and more comfort for the patient because it is a noncontact method, anesthesia is unnecessary, and the risk of corneal infection is avoided. Invest Ophthalmol Vis Sci 1993; 34:1886-1893.
An modern ophthalmology the precise knowledge of intraocular distances is very important. The axial length of the eye is one of the main parameters for all
From the *inslitut fur Medizhiische Phy.silt, Universittit Wien, Vienna, and the ^Department of Ophthalmology, Lahiz Hospital, Vienna, Austria. Supported by grant P 7300 MED from the Austrian Fonds zur Fordennig der luissenschaft lichen Forschuiig (FWF). Submitted for publication,: February 10, 1992; accepted June 29, 1992. Proprietary Interest Category: P. Reprint requests: Christoph K. Hitzenberger, Institut fur Medizhiische Physik, Wa'hringer Strafie 13, A-1090 Vienna, Austria.
intraocular lens power calculation formulae. Today the common method for measuring intraocular distances is the ultrasonic echo-impulse technique (US technique). Since the first measurements in 1956,1 this technique has been steadily improved and is now of clinical standard. The US technique enables the measurement of the axial eye length as well as any other intraocular distance, independent of the clarity of the crystalline lens, but because of the necessary mechanical contact between instrument and eye topical anesthesia is needed and the risk of local infections exists.
1886
Investigative Ophthalmology & Visual Science, May 1993, Vol. 34, No. 6 Copyright Association for Research in Vision and Ophthalmology
Interferometric Measurement of Cataract Eye Length Another drawback is the limited resolution attained by the US technique. During the past few years, new optical methods for measuring intraocular distances were reported. The femtosecond optical ranging technique was used to determine the corneal thickness of anesthetized rabbit eyes in vivo.2 A modification of the slit lamp technology was proposed to measure the thickness of the human retina.3 The axial length of the human eye was measured by interferometry with partially coherent light.4 An improved version of this technique, laser Doppler interferometry (LDI), reduced the measuring time to 3 seconds,56 and, with a modified instrument, enabled the measurement of the corneal thickness.7 First measurements of the axial eye length, carried out by the LDI technique on healthy eyes of volunteer subjects, were in good agreement with US results, with the added advantage of much greater precision.5 The main remaining question, from a clinical point of view, is whether the LDI technique can be applied also to cataract eyes, since light scattering by cataract lenses might limit the use of an interferometric technique. To answer this question, an extensive study on the applicability of the LDI technique for measuring the axial length of cataract eyes was conducted. The purpose of this study was to clarify the following questions: Is the technique feasible for measurements on elderly patients? To which quantitative degree of cataract is the technique applicable? How do the results of LDI compare to those of the US technique? The results are reported here.
1887 be maintained within approximately 0.5 mm during the measurement time of roughly 3 sec. This accuracy ensures that the width of the interference fringes, which cause the LDI signal, is not less than the width of the photodetector, so the measurement can be made. Longitudinal eye motions (ie, parallel to the optical axis) occurring during the measurement time do not affect the results in any way. This is achieved by the special interferometric setup, which uses reflections from both the cornea and the retina simultaneously for the path length matching and therefore does not depend on the distance between eye and interferometer. The precision of LDI was shown to be approximately 30 /urn standard deviation (SD) for the optical length (OL) of the eye. This value includes eye length changes due to blood pulsations, which are of the order of a few /um.9 OL is converted to the geometric length (GL) by a method that is based on Gullstrand's schematic eye10 and uses the group refractive indices of the eye media:5 GL; = GLS + (OL; - O L s ) / i V (GLJ: individual GL, GLS: schematic GL, OL;: individual OL, OLS: schematic OL, n^,: group refractive index of the vitreous). The following constants were used:5 GLS = 24 mm, OLS = 32.518 mm, n^ = 1.3445. The precision of the GL values was shown to be better than 25 /um.5 Usually 8-12 measurements were carried out on each eye by LDI to ensure that at least five evaluable results were obtained. A measurement is called evaluable if a visual check of the measurement curve on the computer monitor showed a sufficient separation of signal and noise. In some cases with excellent signalto-noise ratio, fewer measurements were carried out.
MATERIALS AND METHODS Laser Doppler Interferometry
The method of measuring the axial eye length by LDI has been described elsewhere.56 The measurements reported here were made with an improved instrument initially used for measuring the corneal thickness.7 The laser power was shown to be well within the safety limits.5'7'8 An important point with in vivo measurements is the alignment of the subject's eye with the laser beam. In this work, the axial eye length is measured parallel to the vision axis. This is achieved by asking the patient to look at the beam (the wavelength X = 780 nm is just visible and the beam appears to the patient as a weak red spot). The alignment of the eye with the center of the beam is achieved by a head rest of the type that is commonly used with slit lamps, which is mounted on an x-y translation stage. In case of patients experiencing strong tremors, the fixation of the head can be assisted by adjustable temple supports; a head fixation by a bite board is no longer necessary. With this system, the alignment of vision axis and beam center can
Ultrasound Measurements
US measurements were performed using two different techniques: Each eye was measured once with a DBR 310 (Sonometrics, NY), employing the easy to use applanation technique (A-US technique). The instrument uses a mean sound velocity of 1550 m/s for axial eye length measurements; a separate measurement of individual intraocular distances was not performed. These measurements were carried out routinely by hospital staff members on all patients undergoing cataract surgery. During the study a systematic difference between LDI and A-US results was observed, so we decided to measure 50 eyes additionally by the more accurate but also more complicated water-immersion technique (IUS technique). A Kretztechnik 7200 MA Hochfrequenz Echograph (Kretztechnik, A-4871, Zipf, Aus-
1888
Investigative Ophthalmology & Visual Science, May 1993, Vol. 34, No. 6
tria) was used, employing a transducer with 5 mm diameter and a frequency of 10 MHz. The sound velocities were taken 1532 m/s for the aqueous and vitreous humor and 1641 m/s for the lens, respectively." The calibration of the instrument was checked by measuring a phantom (a trough consisting of plane parallel plates of acryl glass, filled with distilled water) of known dimensions and sound velocity. The results were equal (within the accuracy limits of this technique) to those of the LDI technique. The lengths of the individual intraocular distances (aqueous, lens, vitreous) were determined from Polaroid photographs of the screen of the I-US instrument and added to obtain the total GL of the eye. Two measurements were performed on each of the 50 eyes by this technique and the mean value of both measurements was taken as final result. Cataract Grading Cataract grading was performed by use of the Opacity Lensmeter 701 from Interzeag company (CH-8952, Schlieren-Ziirich, Switzerland). This instrument measures backscattered light from the eye lens, which is illuminated by a light beam of 1.5 mm diameter.12 The measurement is thus restricted to the central area of the lens. The result of the measurement is a dimensionless number between 0 and 99, which we will refer to as lens meter unit (LMU). Higher LMU values indicate higher lens densities. According to the manufacturer, normal lenses give values between 0 and 20 LMU, while higher values indicate cataract lenses. The instrument was used strictly according to the user's manual. Five measurements were performed on each eye after checking that the pupil diameter was at least 4 mm; mean values and SD were calculated by the instrument automatically. The reproducibility of the measurements was usually very good (SD about 1 LMU). For the purposes of this study, the eyes were classified according to their LMU values into groups of width 5 LMU, ranging from 15 to 20 LMU, 20 to 25 LMU, and so on. Values above 90 LMU were combined into one group. Patients The study group consisted of patients undergoing cataract surgery at the Department of Ophthalmology of the Lainz Hospital, Vienna, Austria, during the first 6 months of the year 1991. No special selection of patients was made, so they resemble a typical collective of cataract grades. One hundred patients participated in the study; ages ranged 43-97 yr, mean value SD were 74 10 yr. Thirty-six patients were men and 64 were women. One hundred ninety-six cataract eyes were investigated by LDI, A-US, and Lensmeter, fifty of these eyes were measured additionally by I-US.
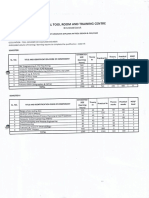
The study followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients after the nature and possible consequences of the study were explained. Approval by the institutional human experimentation committee was obtained. Statistics In a summary statistics, the distribution of cataract grades was determined. The total percentage of eyes measurable by LDI, the percentage of evaluable single LDI scans, and the repeatability (the SD) of the LDI results were determined as a function of cataract grade. Linear regression analysis was used to test for correlations between the following parameters: GL(LDI) vs GL(A-US); GL(LDI) vs GL(I-US); GL(LDI) vs DA; GL(LDI) vs DI; LMU vs DA; LMU vs DI(GL(LDI; A-US; I-US): geometrical length determined by LDI, A-US, and I-US, respectively; DA: difference between GL(LDI) and GL(A-US); DI: difference between GL(LDI) and GL(I-US); LMU: lens meter units (cataract grade)). Finally, the eye length results obtained by the different measurement techniques were compared by a paired Student's t test after checking for normal distribution of the differences by the x2 test. RESULTS Influence of Cataract Grade on LDI Results Figure 1 shows the frequency distribution of cataract grades of the eyes of this study. The number of eyes in each class is shown at each histobar. The number in parentheses indicates the number of eyes that were measurable by LDI. Most of the eyes are graded in low to intermediate classes. Only a relative small amount of eyes is graded in classes higher than 60 LMU. Nine eyes had values higher than 90 LMU. Seven of them were out of the measuring range of the instrument (ie, > 100 LMU). These eyes were judged as completely opaque by an ophthalmologist. LDI was able to measure 90.5% of the eyes. Only 12 eyes in classes below 90 LMU were not measurable: computer problems prevented the measurements in four cases, fixation problems of the patients in seven cases, and high lens opacity in one case. Only two of the nine eyes in the class > 90 LMU could be measured by LDI. Figure 2 shows the evaluability of single measurements as a function of cataract grade. The cataracts classified higher than 55 LMU were combined in three groups: 55-65 LMU, 65-90 LMU, and > 90 LMU, respectively, for statistical purposes (each class contains at least 5 eyes). The abscissa shows the cataract classes and the ordinate the percentage of evaluable
Interferometric Measurement of Cataract Eye Length
1889
S IS S !8 V S IS S CATARACT GRADE (LMU)
e s
FIGURE l. Frequency distribution of cataract grades. The number of eyes graded in each cataract class is plotted vs the cataract grade (in lens meter units: LMU). The number printed in each histobar equals the number of eyes graded in this class. Where the number of eyes that were measurable by LDI differs from the total number of eyes, the number of evaluable eyes is shown in parentheses.
single measurements in each class. This is the mean value (in percent) of the ratio evaluable/total number of measurements carried out on each eye and is a measure of the number of times an eye has to be scanned to get a certain number of evaluable results. This evaluability must not be confused with the percentage of eyes measurable in each class (this was nearly 100% in all of the classes below 80 LMU). The evaluability decreases gradually from approximately 75% in the case of the lowest cataract class to approximately 40% in the classes ranging 55-90 LMU. The sudden drop to
below 15% in the class above 90 LMU reflects the large number of eyes in this class that were not measurable. These evaluability percentages, however, are only crude figures. A strong variability between the individual eyes within the cataract classes is observed. Especially in the cases of the higher cataract classes, the evaluability can vary from about 20 to 90% (the immeasurable eyes excluded), strongly depending on the individual patient's fixation capability. The mean SD of GL of all 177 eyes is 19 /tun. The value of the SD is roughly constant for the cataract
.*. 60-
CATARACT GRADE (LMU)
FIGURE 2. Evaluability of single LDI scans. The percentage of single LDI scans that were evaluable is plotted vs the cataract grade. This is a measure of the number of times (at average) a single eye has to be scanned to get a certain number of evaluable results and is correlated with the mean signal-to-noise ratio. It must not be mixed up with the total percentage of evaluable eyes in each class.
1890
Investigative Ophthalmology & Visual Science, May 1993, Vol. 34, No. 6
grades between 15 and 90 LMU. It is approximately 30 /im above 90 LMU, but in this class only two eyes were measurable. Comparison of LDI and US Measurements Figure 3 shows a plot of GL values measured by LDI and by US, respectively. The values obtained by US are plotted as a function of the LDI results. In Figures 3a and 3b, the A-US values and the I-US values, respectively, are shown. A linear regression analysis was performed in each case. The solid line in each figure is the corresponding regression line, the dotted lines at each side of the regression line show the 95% prediction limits (ie, 95% of the data are located between these
lines). The correlation is excellent in both cases with correlation coefficient r = 0.97 and 0.99 in Figures 3a and 3b, respectively. The slopes of the regression lines and their standard errors are 0.99 0.02 (Fig. 3a) and 1.02 0.02 (Fig. 3b). The vertical width of the 95% prediction interval is approximately 1 mm (Fig. 3a) and 0.5 mm (Fig. 3b) for the range of GL values covered by these figures. A systematic difference between LDI and US values was observed. The mean value of DA (GL(A-US) - GL(LDI)) SD is -0.47 0.25 mm (n = 179), the mean value of DI (GL(I-US) - GL(LDI)) SD is 0.18 0.12 mm (n = 50). These values are highly significant. A paired Student's t test showed signifi-
28
,
, .
26
-
, i ,
24
'its0
.
a 22
i i
'
"yon
5 "
| , i ,
28 28 22
. 24 GL OBTAINED BY LDI (MM) 26 28
28
26
^T'
suQas 24
?,' *
22
?*
i QL OBTAINED BY LDI (MM)
26
FIGURE 3. Comparison of LDI and US results. The geometric eye length (GL) obtained by US, is plotted vs the GL obtained by LDI. Solid line: regression line. Dashed lines: 95% prediction limits. (A) US values measured by applanation technique (A-US). (B) US values measured by immersion technique (I-US). Very good correlations are observed.
Interferometric Measurement of Cataract Eye Length cance values of P < 2 X 10 15 in both cases (it should be mentioned that only the DI, but not the DA values passed the x 2 t e s t f r normal distribution (DI: P = 0.55, DA: P= 2 X 10"7)). Linear regression analysis revealed no correlation of GL and the differences DA and DI (the respective correlation coefficients are 0.05 and 0.14). No correlation was found for cataract grade and DA and DI, either (r = - 0 . 0 9 and - 0 . 0 4, respectively).
1891 reproducibility. The fact that only lens opacities near the vision axis are taken into account is a great advantage for the purpose of this study, because only these opacities are located within the light path of the LDI instrument and are therefore able to deteriorate the instrument performance by light scattering. Consequently, a useful correlation between instrument performance and cataract grade is enabled. Influence of Cataract Grade on LDI Measurements
DISCUSSION
In this study, the LDI technique, which was recently developed for the measurement of intraocular distances, was used for the first time to examine a large number of cataract eyes. In most cases, no major problems associated with the instrument and its measurement principle occurred. 196 cataract eyes were examined, 177 (ie, 90.5%) were measurable by LDI. In four cases (2%), the instrument failed because of computer problems. This malfunction can be attributed to the instrument being a prototype; it was not caused by the measurement principle. The measurement relies on the fixation ability of the patient. In some cases, the patients had fixation problems. This can be observed by the instrument operator during the alignment and measurement process, because in this case, the reflected beam will move erratically across (and even beyond) the visual field of the infrared scope of the detection unit. In this case, it is difficult or even impossible to align the detector with the center of the reflected beam (or the center of the interference fringes, which give rise to the LDI signal), and no signal will occur. However, most of the patients who had fixation problems were able to fixate the beam for the 3 sec needed for a single scan. The whole measurement session for acquiring approximately five evaluable scans took longer (up to 10 min) than in the cases of no fixation problems (about 2-3 min). In seven cases only (3.5%) the fixation problems were so severe that no measurement could be carried out successfully. This percentage can probably be further reduced by increasing the speed of the stepper motor that drives the scanning mirror, which decreases measurement times to 1 sec or even less. Cataract Grading Cataract grading was performed with a commercial instrument that measures backscattered light from the central part of the lens.12 The lens density is given as a dimensionless number. No calibration to real physical units is available. Compared to other, more common methods (based on slit lamp photography), 1314 the instrument is easier to use and yields a higher resolution and better
The results of this study show that LDI works very well with low to intermediate cataracts (up to 55 LMU). Even with higher cataract grades (up to 90 LMU) LDI worked well. The reason for this good performance is probably the use of the rather long wavelength of 780 nm, which is much less scattered than light of shorter wavelength. There was only one failure of LDI in this range of cataract grades which could be attributed to lens opacities (the respective lens density was 85 LMU). In all other cases, only the signal-to-noise ratio decreases with increasing lens density, which can be deduced from the gradual decrease of evaluable single measurement scans with increasing lens density (Fig. 2). In some cases (about 5% of all measurable eyes), where high lens density and fixation problems occurred for the same eye, the evaluation of single scans became difficult because of the poor signal quality. However, the comparison of several successive scans yielded reliable results even in these cases. (It should be mentioned that only six patients (3%) had cataract grades in the range 65-90 LMU, so the statistics of this range are poor.) No effect of cataract grade on the precision of the LDI results was observed in the range up to 90 LMU. The mean SD of GL of 19 /xm compares well to the value of <25 /zm reported for healthy volunteer subjects. 5 However, 90 LMU seems to be the limit up to which LDI can be used at present. Seven of the nine eyes (3.5% of the total number of eyes) graded higher than 90 LMU were not measurable. That most patients now apply for cataract surgery in early stages of reduced visual acuity is very favorable for the LDI technique. If, however, a light source with the required coherence properties emitting at a wavelength X = 1.1 nm becomes available, the current limit of 90 LMU might be extended. Comparison of LDI and US Measurements A very good correlation between LDI measurements and US measurements was found by linear regression analysis. The slopes of the regression lines equal 1 within the standard error of the analysis. The halfwidth of the 95% prediction interval is about 0.5 and
1892
Investigative Ophthalmology & Visual Science, May 1993, Vol. 34, No. 6 In conclusion, the advantages of the LDI technique are summarized. Its precision of about 20 pm is unrivalled by the US technique. The total accuracy is better (< 50 /xm compared to 120 to 200 nm) even in the present state, where only the total axial length, but not the individual intraocular distances are measured (these measurements are possible in principle). The LDI technique is easy to use and very comfortable for the patient. It is a noncontact technique that requires no anesthesia and avoids the risk of corneal infection. There are still many possibilities for further development of this method. The feasibility of fundus profile measurements 5 and measurements of the retinal thickness 517 have already been demonstrated and the possibility of further improvement of the resolution by use of a light source of shorter coherence length was shown.17 By increasing the speed of the stepper motor, the time required for a single scan could be reduced to one second or less. This might reduce the number of eyes that are not measurable because of fixation problems. Therefore, the LDI technique has a great potential for future applications. Key Words biometry, eye length measurement, cataract, laser Doppler interferometry, interferometry Acknowledgments The authors thank Mr. H. Sattmann for the construction of the electronics and the software of the LDI instrument. References 1. Mundt GH, Hughes WF. Ultrasonics in ocular diagnosis. Am] Ophthalmol. 1956;41:488-498. 2. Fujimoto JG, De Silvestri S, lppen EP, Puliafito CA, Margolis R, Oseroff A. Femtosecond optical ranging in biological systems. Optics Letters. 1986; 11:150-152. 3. Zeimer RC, Mori MT, Khoobehi B. Feasibility test of a new method to measure retinal thickness noninvasively. Invest Ophthalmol Vis Sci. 1989;30:2099-2105. 4. Fercher AF, Mengedoht K, Werner W. Eye length measurement by interferometry with partially coherent light. Optics Letters. 1988; 13:186-188. 5. Hitzenberger CK. Optical measurement of the axial eye length by laser Doppler interferometry. Invest Ophthalmol Vis Sci. 1991;32:616-624. 6. Fercher AF, Hitzenberger C, Juchem M. Measurement of intraocular optical distances using partially coherent laser light. ) Mod Optics. 1991; 38:13271333. 7. Hitzenberger CK, Drexler W, Fercher AF. Measurement of corneal thickness by laser Doppler interferometry. Invest Ophthalmol Vis Sci. 1992; 33:98-103. 8. American National Standards Institute. Safe Use of Lasers. New York: American National Standards Institute; 1986. ANSI publication Z 136.1. 9. Fercher AF. In vivo measurement of fundus pulsa-
0.25 mm in the case of A-US and I-US measurements, respectively. A systematic deviation with high significance was observed for the three measurement techniques. The LDI technique yields the highest GL values, the A-US technique the lowest. No correlation between length and differences is observed. Therefore, the systematic deviations are not caused by errors in the sound velocities or in the refractive indices of the eye media (in this case, a linear relationship of length and difference should be observed). Also, the lack of correlation between cataract grade and differences indicates that the lens opacities have no influence on sound velocity and refractive index, at least within the accuracy of measurement (or these influences balance each other). The smaller GL values of the A-US technique can be attributed to its coupling technique: because of the direct contact between transducer and eye the cornea is indented and the eye shortened. The larger GL values of the LDI technique can be explained by a reflection of sound and light at different layers of the fundus. The LDI signal was shown to originate from a reflection at the retinal pigment epithelium. 5 A weaker LDI signal, which occurs occasionally at optical distances of approximately 250 jiim in front of the main signal, was attributed to a reflection at the internal limiting membrane. 5 Using the mean group refractive index n g = 1.35495 of the schematic eye, this corresponds to a geometric distance of 185 ium. This is approximately equal to the mean GL difference between LDI and I-US results. Therefore, we conclude that the US technique measures the distance cornea-internal limiting membrane. This agrees with some intraocular lens formulae that are based on US measurements and take an additional retinal thickness of 0.2 mm15 into account. (These recent results contradict the preliminary results reported earlier, 5 where no systematic difference was observed. However, the earlier US results were based on single measurements. Furthermore, the instrument was not calibrated with a phantom, so they were probably less accurate than the results reported here.) The last point to be discussed concerns the accuracy of the methods. Since the A-US technique is less accurate than the I-US technique, it will not be discussed here. The SD of the differences DI (LDI I-US) is approximately 120 /xm. Because this value corresponds to the lower limit of accuracy ranges (120-200 /JIII) reported in literature for the US technique, 1615 the deviations of US and LDI techniques are mainly caused by inaccuracies of the US technique. This is in agreement with theoretical considerations, 5 which predicted that the errors caused by the approximations made in the OL to GL conversion of the LDI technique will be less than approximately 50 urn.
Interferometric Measurement of Cataract Eye Length tions by laser interferometry. IEEE J of Quantum Electronics. 1984; QE-20:1469-1471. Obstfeld H. Optics in Vision. London: Butterworth; 1982:28-42. Jansson F, Kock E. Determination of the velocity of ultrasound in the human lens and vitreous. Ada Ophthalmol. ]962;40:420-433. Flammer J, Bebie H. Lens opacity meter: A new instrument to quantify lens opacity. Ophthalmologica. 1987; 195:69-72. Chylack LTJr, Leske MC, McCarthy D, Khu P, Kashinagi T, Sperduto R. Lens opacities classification system II (LOCS II). Arch Ophlhalmol. 1989; 107:991997.
1893 14. Taylor HR, Lee JA, Wang F, Munoz B. A comparison of two photographic systems for grading cataract. Invest Ophthalmol VisSci. 1991; 32:529-532. 15. Boerrigter RMM, ThijssenJM, Verbeek AM. Intraocular lens power calculations: The optimal approach. Ophthalmologica. 1985; 191:89-94. 16. Binkhorst RD. The accuracy of ultrasonic measurement of the axial length of the eye. Ophthalmic Surg. 1981; 12:363-365. 17. Hitzenberger CK, Fercher AF, Juchem M. Measurement of the axial eye length and retinal thickness by laser Doppler interferometry. In: Puliafito CA, ed. Ophthalmic Technologies. Proc SPIE. 1991; 1423:4650.
JO. 11. 12. 13.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Planar Stages 2022 - RemovedDocument26 pagesPlanar Stages 2022 - Removedakbar raizoNo ratings yet
- CVI Optical SpecificationsDocument8 pagesCVI Optical SpecificationsAmir MolazecirovicNo ratings yet
- Bath Interferometer English High ResDocument5 pagesBath Interferometer English High ResMarcelo GomesNo ratings yet
- 1996 IET AirWedgeInterferometer PDFDocument6 pages1996 IET AirWedgeInterferometer PDFSriNo ratings yet
- I Inteference Diffraction MCQDocument24 pagesI Inteference Diffraction MCQPuneet Kumar Trivedi0% (2)
- John Bedini - My Work On Rife - HeterodyningDocument15 pagesJohn Bedini - My Work On Rife - HeterodyningoveryounityNo ratings yet
- Dual Degree Sylabus Chemistry - 200916Document87 pagesDual Degree Sylabus Chemistry - 200916hp pavilionNo ratings yet
- Ptical Oherence Omography: Revealing Inner Space Like You Have Never Seen BeforeDocument20 pagesPtical Oherence Omography: Revealing Inner Space Like You Have Never Seen Beforeymyip2001No ratings yet
- OpticsDocument2 pagesOpticssheriff98100% (2)
- 2a - Precision-Interferometer-Experiment 1Document27 pages2a - Precision-Interferometer-Experiment 1Brenda CruzNo ratings yet
- Metrology and Measurements - Lecture Notes, Study Material and Important Questions, AnswersDocument7 pagesMetrology and Measurements - Lecture Notes, Study Material and Important Questions, AnswersM.V. TVNo ratings yet
- Applsci 02 00602Document27 pagesApplsci 02 00602Marcelo CostaNo ratings yet
- Radius of A StarDocument6 pagesRadius of A Starishaan yadavNo ratings yet
- Deformation Measurement and Monitoring With GBSAR PDFDocument119 pagesDeformation Measurement and Monitoring With GBSAR PDFIvanaNo ratings yet
- Straightness MeasurementDocument6 pagesStraightness Measurementlakku12No ratings yet
- Soller 2005Document9 pagesSoller 2005YojikNo ratings yet
- Question Bank 03062016Document7 pagesQuestion Bank 03062016Babu NarayananNo ratings yet
- Lab Report Interferometer....Document14 pagesLab Report Interferometer....musabNo ratings yet
- Nondestructive Active Testing TechniquesDocument50 pagesNondestructive Active Testing TechniquesJack OuyangNo ratings yet
- Photonics 09 00590 v2Document9 pagesPhotonics 09 00590 v2J. M. M.No ratings yet
- Anand K. Bewoor - Vinay A. Kulkarni - Metrology & measurement-McGraw-Hill Education (2009) PDFDocument599 pagesAnand K. Bewoor - Vinay A. Kulkarni - Metrology & measurement-McGraw-Hill Education (2009) PDFMahmud RezaNo ratings yet
- Qualification of IRDocument28 pagesQualification of IRRavi KantNo ratings yet
- Coursecontent PDFDocument29 pagesCoursecontent PDFSree Vasthava RamichettyNo ratings yet
- Fourier Transforms by R.C. JENNISONDocument126 pagesFourier Transforms by R.C. JENNISONThe Negative AngleNo ratings yet
- A Project On Michaelson InterferometerDocument28 pagesA Project On Michaelson InterferometerMitanshu ThakoreNo ratings yet
- Synthetic Aperture Radar: Navigation Search Improve This Article CitationsDocument11 pagesSynthetic Aperture Radar: Navigation Search Improve This Article CitationsshafeeulahmedNo ratings yet
- Shimadzu FTIR 8400s ManualDocument16 pagesShimadzu FTIR 8400s ManualMohammed HamzahNo ratings yet
- Me2304 - Engineering Metrology and Measurements Question Bank For Regulation 2008Document29 pagesMe2304 - Engineering Metrology and Measurements Question Bank For Regulation 2008Ashok Kumar Rajendran75% (4)
- THEME - Dutch Society For Precision EngineeringDocument7 pagesTHEME - Dutch Society For Precision EngineeringGary Ryan DonovanNo ratings yet
- MPR Seminar Report 1Document22 pagesMPR Seminar Report 1abhiramks222No ratings yet