Professional Documents
Culture Documents
Market Engineering For Electronic Health Services
Uploaded by
mamatnamaku0 ratings0% found this document useful (0 votes)
22 views10 pagesThis paper conducts a case study on telemonitoring, which has significant positive impact on patients with chronic heart failure. The presented solution can be built upon the emerging German infrastructure for telemedicine and be extended to further regions later.
Original Description:
Original Title
4525a952
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis paper conducts a case study on telemonitoring, which has significant positive impact on patients with chronic heart failure. The presented solution can be built upon the emerging German infrastructure for telemedicine and be extended to further regions later.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
22 views10 pagesMarket Engineering For Electronic Health Services
Uploaded by
mamatnamakuThis paper conducts a case study on telemonitoring, which has significant positive impact on patients with chronic heart failure. The presented solution can be built upon the emerging German infrastructure for telemedicine and be extended to further regions later.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 10
Market Engineering for
Electronic Health Services
Sebastian Dnnebeil
1
, Ali Sunyaev
2
, Jan Marco Leimeister
3
, Helmut Krcmar
1
1
Department of Informatics
1
Technische Universitt Mnchen
Germany
{duennebe |krcmar}@in.tum.de
2
Faculty of Management and Social Sciences
2
University of Cologne
Germany
sunyaev@wiso.uni-koeln.de
3
Research Center for IT Design (ITeG)
3
University of Kassel
Germany
leimeister@uni-kassel.de
Abstract
Various studies have proven the positive impact of e-
health solutions on treatment success and health care
spending. Utilization of e-health is therefore urgently
recommended by German health authorities. However,
the diffusion of such technologies is currently very low,
despite the availability of the underlying technology. A
market failure is a likely reason for the unsatisfying
situation, as there are currently hardly regular
business models for electronic health services. This
paper conducts a case study on telemonitoring, which
has significant positive impact on patients with chronic
heart failure, to illustrate a market engineering
approach for e-health applications. The introduced
case study is located in a southern German region,
where health insurances and a physician network want
to establish a telemonitoring solution. We investigate
the socioeconomic, technical and legal environment in
order to derive a transaction object and build a
transaction service. Patients will transfer vital
parameters to physicians on a daily base. Caregivers
observe patients health status and compile quarterly
reports for the e-health provider. The provider
distributes the funds of the health insurances according
to the compliance among the stakeholders and adjusts
the model on an annual base according to the realized
savings. The presented solution can be built upon the
emerging German infrastructure for telemedicine and
be extended to further regions later.
1. Introduction
In 2008 the German public health system was the
biggest national service industry, responsible for total
revenue of 263.2 billion. Healthcare spending
amounted for about 10.5% of the German gross
domestic product (GDP) [21]. According to estimates
the spending will rise to 453 billion in 2020, which
will represent approximately 15.5% of the national
GDP by then [18]. Healthcare spending can be divided
into public and private funds. The public spending
represents the mayor proportion, with about 75% [28].
In Germany citizens and employers pay solidary funds
to public and private health insurances. The funds are
distributed quarterly by physicians associations to
registered caregivers, according to the recorded
treatment of the last quarter. All allowable treatments
are fixed in a treatment or medication catalogue ex
ante, in order to be refundable [23]. Health systems
around the world have seen multiple innovations in the
field of electronic health (e-health). The benefits of
these applications are proven in many cases [29, 10].
Despite the positive evidence, IT services are currently
not part of the German treatment catalogue and can
therefore not be billed by caregivers in the regular
allowance process. Advantages of e-health in terms of
efficiency and treatment quality have been investigated
in the applications such as:
2012 45th Hawaii International Conference on System Sciences
978-0-7695-4525-7/12 $26.00 2012 IEEE
DOI 10.1109/HICSS.2012.423
952
Telemonitoring, which has strong evidence of
being beneficial in various aspects of healthcare.
Hospitalization, mortality rate, lack of work, and
the overall treatment costs can be reduced
tremendously by this e-health application [15, 19].
Prevention of adverse events (medical errors),
which cause more casualties than breast cancer,
traffic accidents, and AIDS combined, and can be
limited significantly by the usage of e-health
application [1, 10].
Applications managing the accurate discharge of
prescriptions, which show advantages, compared to
the traditional medication handling. These help to
decrease the rate in unadjusted absolute death rate
by 27% for cardio-vascular patients after one year
[22]. Considering the fact that wrong medication in
the united States cost $4.4 Billion in 2006 [17] and
37.4% of all adverse events are caused by wrong
medication [1], the potential is significant.
Hence, the utilization of such supporting information
systems (IS) is urgently recommended by German and
European authorities and the diffusion of such
technologies is subject of major efforts [10]. However,
the diffusion speed of the listed applications is, despite
the enormous potential for fund saving, currently very
low [9]. The unsatisfying adoption rate of e-health,
especially for telemonitoring, indicates a market
failure. As the underlying technology is available and
the benefits have been proven, a working market to
organize and accelerate distribution and adoption is a
key element for diffusion. Therefore, the intention of
this paper is the development of a sustainable market
model for telemonitoring, involving both, consumers
and providers of e-health applications. The overall goal
is to enable the utilization of e-health technology to
improve the overall treatment quality.
We conducted a case study, based on a region in
southern Germany with 452,000 inhabitants on 2,847
square kilometers. The region is geographically well
definable because of its heterogeneous structure, which
makes the region suitable for field testing since it
represents the structure of Germany very accurately
[32]. The caregivers of the region, their physician
network, as well as the health insurance are willing to
establish telemonitoring. Therefore, the health
insurances want to allocate funds to create a market for
telemonitoring in order to encourage companies to
supply solutions. The market setup is embedded in the
roll-out process of the national electronic health card
(eHC) system. German health authorities are currently
building a nationwide telematics infrastructure (TI) to
connect care providers IS via a common network [11].
On the basis of the proposed TI, telemedicine services
will offer communication, cooperation, and
documentation features implemented as web services
to ensure pervasive availability and integrity of
medical data among the German public health system.
In the case of the proposed infrastructure, medical
patient data is either stored on central servers or
portable carriers (i.e., smart phones and tablet devices)
or eHC. The secure infrastructure is considered as a
major enabler of electronic health services, e.g., for
telemonitoring.
2. Methodology
The exploratory nature of this research within the
context of a physician network was related to the
national roll-out of the eHC and guided the authors to
adopt a qualitative and interpretive approach to the
inquiry. The empirical part of this research follows an
exploratory research design with the intention of
generating an empirically motivated market model; it is
not the intention to test a given research model (for
methodological aspects of explorative research designs
see e.g. [4] or [3]). Case study research itself is widely
used in IS research (for an approach on how to build
theories from case study research see e.g., [8]). Four
semi standardized oral interviews were conducted: two
with board members of the physician network (the
business manager and the chairman who additionally
works as a general practitioner) and a further two board
members of a health insurance, which insures 80,000
people in the region. Additionally, data from two
general practitioners health information systems were
analyzed. The literature on previously conducted
research was (where available) also included. The
study is still on-going, but the main interviews were
conducted in a 2-month period in 2010 as part of the
introductory project of the eHC.
2.1 Market Engineering
The paper aims to create a market for telemonitoring.
Therefore, we use a market engineering approach [31]
to achieve the desired market result in the given
socioeconomic, technical and legal environment. The
desired market result is the best possible monitoring of
patients with heart failure, in order to reduce the rate of
hospitalization, lack of work and the costs caused by
the disease. The possible savings, resulting from
prevention of hospital treatments should be distributed
to the involved stakeholders. Hence, secure transaction
objects, (the monitoring documentation) are designed,
the transaction service created for the given micro-,
infra- and microstructure of the market. Later
evaluation can be done in analysis of the market
results. Satisfying market results are achieved, when
953
telemonitoring solutions report equal results in the field
as clinical studies reported for research projects. The
output parameters are set accordingly to be able to
judge the market result after setup of the e-health
applications.
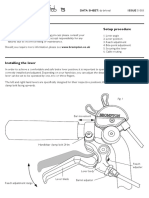
Figure 1 Market Engineering Framework according
to [31]
3. Case Study
3.1. Chronic Heart Failure Medical
background
Heart failure is one of the most widespread chronic
diseases in Germany [27]. The patients hearts are not
able to supply the organism with sufficient blood flow
and oxygen to ensure that the human metabolism is
working well. In case of chronic heart failure (CHF)
the metabolism compensates the low oxygen supply by
higher heart rate, vascular stenosis, thickening the
myocardial muscle or an increase in blood volume.
This can temporarily stabilize the oxygen delivery to
the end organs. Patients with compensated CHF
temporarily do not show any symptoms of the disease
[20]. Decompensation of CHF, caused e.g., by heart
attack or pneumonia, leads to fluid retention and
uncontrolled hypertension, during rest or light
exposure. Medical guidelines provided by the German
Medical Association therefore advise daily monitoring
of patients blood pressure, heart frequency and weight
[2]. A significant increase in a patients weight during
a short period is e.g. a strong indicator of fluid
retention, caused by a decompensation in the case of a
heart attack. Also low hypotension (systolic blood
pressure) can indicate a decompensation. Early
identification of a decompensation allows caregivers to
take counteractive measures as early as possible,
before the patients hospitalization because of dyspnea
(breathlessness), pulmonary edema or acroedema
(water retention in lungs or legs) is inevitable. The
application for telemonitoring should support this
monitoring action in the best possible manner. Sensors
record the vital parameters and transmit them to
physicians for monitoring [15].
3.2. Organizational Setup
The region in southern Germany counts 452,000
inhabitants. 500 of the 600 ambulatory physicians
treating the patients of the region, are organized in a
physician network [32]. The physician network has the
organizational setup of a GmbH: a private company
limited by shares (the German equivalent to a Limited
Company). The network is thereby able to generate
revenue, which can then be distributed to the
shareholders. All physicians have equal shares in the
physician network, and the earnings of such a network
are either distributed equally or according to dedicated
contracts. The physician network can negotiate
treatment contracts with the health insurances of the
region directly. This enables physicians to earn money
beyond the fixed allowance catalogue of the German
ambulatory health system. Two health insurances were
contacted by the physician network and asked whether
they were willing to set up a market for telemonitoring.
Each of the two health insurances has approximately
80,000 insurants. Including the co-insured family
members, about half of the inhabitants of the region are
insured by either of the two health insurances. Both
health insurances, -one a dominant German health
insurance and the other the health insurance of a
globally operating company with headquarters in the
region, are willing to allocate funds in order to enable
the market for telemonitoring.
The current legal conditions of the German public
health system, which hinder the adoption of e-health,
are briefly described in section 4.3.
4. Environment Studies
4.1. Socioeconomic Environment
In 2006 317,000 patients with a diagnosis of CHF lived
in Germany. The treatment cost in the same year
summed up to 2.9 billion, which represented about
1.1% of all national health expenses [21]. CHF
furthermore caused the highest number of
hospitalizations, reported to be caused a single disease.
Market Results
(allocation and prices)
Behavior of the market
participants
Transaction Object
Socioeconomic, Technical
and legal environment
Transaction Services
(Market Structure)
Infrastructure Micro-
structure
Business-
structure
Market Quality
(Interpretation of the results,
considering the environment)
954
60% of all CHF related costs were caused by hospital
stays. In 2008 CHF caused 48,918 cases of death,
representing a share of 5.8% of the annual German
death rate [27].
Cascading the number of 317,000 Patients with CHF
down to the case study, the region is likely to have
about 1700 patients suffering CHF, as the region is
representative for Germany. Hence, the physician
network is responsible for the treatment of about 1500
patients. 750 of those patients are insured by one of the
two health insurances that want to set up a market for
telemonitoring. The case study employs estimations, as
no detailed data was available during the research. The
physician network has 250 general practitioners, which
are responsible for monitoring of CHF [2]. Hence, each
physician treats approximately three patients with
CHF. The numbers from taken from the IS of two
caregivers indicated a higher number. Over a period of
five years 53 respectively 45 patients with Diagnoses
were recorded in the health information system.
Despite the variation, the calculation bases on the
estimation that three patients with CHF are monitored
in average by one physician.
According to a study on telemonitoring [15], the
average annual financial benefit of telemonitoring for
one patient with CHF is at least 3,000 Euros.
Considering the total cost of approximately 9,000
Euros per year, a treatment cost reduction of one third
can be achieved. Hence, the health insurances try to
save money by the avoidance of hospital treatment,
which means redirecting funds from hospitalization to
prevention by using telemonitoring solutions. If the
underlying studies prove to be accurate, which is a
basic assumption of this paper, utilization of
telemonitoring is more efficient for health insurances
than hospitalization. Furthermore, the savings achieved
by telemonitoring should be sufficient to cover the
additional treatment cost of the physician and the
market price of a telemonitoring solution, and thus the
health insurances will save money. Initially, a share of
one third of the estimated total cost reduction was the
saving target of the health insurances when initiating
the market. Two thirds should be set up as funds for
the provider of the telemonitoring solution. The
solution provider will need to partly use the funds as an
incentive for patients and caregivers to regularly
participate in the monitoring. The payment should
depend on the compliance of patients and caregivers.
An incentive of one Euro per transaction per patient is
suggested here and an incentive of maximal 225 Euros
for a caregiver per quarter. This was reported in an
interview to be a sufficient amount for a monthly time
effort of one hour. As Figure 2 indicates, when
monitoring at least three patients with CHF, the
additional annual income totals 2,700 Euros. Figure 2
illustrates the financial flow and names the most
important stakeholders beside the health insurance:
service providers, patients and caregivers.
Figure 2 Financial Environment.
For health insurances, even a zero saving is considered
a success, as the treatment quality can be increased
when reducing the hospitalization rate. Further the
current calculation considers only the actual treatment
costs; however, the adjusted expenses for CHF are
much higher. Including the indirect costs, caused by
lack of work, the adjusted annual advantage of
telemonitoring totals 6,300 Euros per patient [15]. The
distribution of the funds to the stakeholders aims to
maximize the savings of the annual treatment costs.
The total market volume for CHF-telemonitoring in
Germany adds up to approximately 230 million per
year. In the region the market volume is only 500,000
Euros, however, the character of a pilot project can
justify higher investments.
4.2. Technical Environment
In Germany the Telematics Infrastructure (TI) is
used as the backbone for the mandatory eHC system.
The infrastructure connects existing IS of care
providers via a common network [25]. Within the
service-oriented architecture (SOA) of the TI,
centralized servers or decentralized components
provide services, e.g., the encryption, digital signature
and authorization of medical data. The primary
systems of the TI, i.e., information systems of medical
institutions can utilize these services to communicate
or collaborate with other care providers to maintain,
review or share medical data objects. A local connector
component encapsulates all local services as
encryption or card access and establishes a secure
virtual private network (VPN) connection to the central
servers if needed [12]. All individual-related medical
Revenue for Providers: 735
Incentive for Caregivers : 900
CHF
Annual Cost: 9,000
per patient
Potential
Savings:
3,000
Incentive for Patients : 365
Net Savings: 1000
33%
1/3
2/3
Incentive
Ratio
Utilizationof
Telemonitoring
955
and administrative data that is uploaded to central
servers have to be encrypted, using a hybrid encryption
method [13]. The private keys are located on the smart
card chip of the eHC and cannot be extracted from
there. Hence, they can be used for digital signatures
and the encryption of medical data. Decryption of the
access key happens within the microchip of the smart
card after authorization with a Personal Identity
Number (PIN). Patients can use public keys of health
care institutions to encrypt the data for the receiver in
order to grant them access to their personal medical
data. Given, that the receiver of the medical data is a
specific physician, the patient needs to access the
physicians certificate, either located on the so-called
health professional card (HPC), or available via a
public key infrastructure. To encrypt the medical data
for larger groups of caregivers, e.g., emergency
physicians, institutional smart cards, called Smart
Media Card hold private keys of institutions [12].
The patient related requirements for the
development of the TI are derived from legal
conditions in the German code of social law [6].
Following the political goals of achieving high patient
involvement in medical processes, patients are required
to be in full control of their data. They have to agree on
collection, usage and processing of their medical data
for each service and care provider ex ante. In order to
warrant this requirement, the medical data need to be
encrypted with the public key of the source patient and
is therefore solely accessible with the private key
stored on the patients smart card [13]. It is thus a
mandatory requirement for the TI that patients can
view all their data and the record of its usage. To
ensure that patients could exercise these legally granted
rights, patient interfaces were suggested. An internet-
based front end for home usage was announced in the
initial architecture [11]. A citizen frontend for the new
German ID-Cards was already released that was
compatible with the eHC. This software can be
employed to transfer data from patients locations to
caregivers. Available also are sensors that can transmit
data of weight, blood pressure and heart rate to
caregivers.
4.3. Legal Environment
Markets organize the flows of materials and
services in between individuals and institutions
according to demand, supply and external mechanisms.
Market forces determine design, price, quality and
delivery time of products and services. The buyers
demand goods and services according to these
parameters and their personal requirements and
therewith implicitly regulate markets [24]. Health
systems in contrary are characterized by an organized
flow of funds from citizens and companies to various
caregivers. The flow is regulated by various public
mechanisms and institutions [23]. Public Health
Systems therewith differ from normal markets as: (1)
they normally offer unlimited access to the services
offered in the public health system, (2) show
information asymmetries between the suppliers
(caregivers) and consumer (patients) of health services
and (3) the future personal health status of their
customers is uncertain, and subject to random
fluctuations. These characteristics in sum lead to
market failure [30].
In Germany authorities established a public health
fund, which is equally financed by employees,
employers and receives a tax money subvention. The
fund pays a standard amount to health insurances for
each insured citizen. Treatment and medication are part
of a fixed service portfolio, which has to be reimbursed
by all health insurances according to a standardized
point value, called Einheitlicher Bewertungsmastab
(EBM). There are further direct contracts between
health insurances and caregivers that allow the funding
of additional health services and treatments. The health
insurance can collect an extra amount of money from
their insurants and distribute financial surpluses in
order to achieve some competitive advantages and
diversification [23].
5. Transaction Objects
Medical information is highly confidential data, which
must, according to the regulation in the German law,
not be processed without the patients agreement.
Furthermore, health insurance must not be in control of
all transaction objects, even though they finance the
information object [5]. The interviewers therefore
recommends splitting the information object in three
different objects, each processed in between two of the
major stakeholders.
The first transaction object is derived from the medical
recommendation settled in medical guidelines in order
to achieve the best possible monitoring of patients with
CHF [2]. The transaction object directly follows a
paper based recommendation developed by the Heart
Failure Association of the European Society of
Cardiology [16]. It consists of a daily recording of
weight, heart rate, and blood pressure (diastolic and
systolic). It is compiled at the patients side during the
monitoring and transmitted to the general practitioner
for pure medical purposes (Figure 3). Goal is an
automated handling of this transaction object to
improve acceptance and compliance of the technology
in the daily routines of the patients with CHF.
956
Figure 3 - Telemonitoring transaction object (own illustration)
Precondition is the patients registration to the
program, which is not mandatory. Patients agree on the
financial benefits and the processing of anonymous
measures to the health insurance and the service
provider. Caregivers receive the monitoring record
once a day. The caregivers compile the data
continuously into a diagram which helps to supervise
patients status of health. At the end of each quarter,
caregivers create a report for each patient. Lack of
work, monitoring compliance, hospitalization and the
CHF related treatments are added to the report, which
is the second transaction object and processed to the
service provider. The data enables providers to
organize the accounting and integrate global measures.
The global measures contain overall data of all patients
with CHF and enable the health insurance to monitor
the success of the market and adjust the incentive
structures accordingly.
6. Transaction Services
6.1. Microstructure and Infrastructure
Due to the introduction of the eHC in Germany and
the regions character as a testbed, the implementation
of the application should be based on the German TI.
The following use case was the suggested
microstructure for the telemonitoring solution. Figure 4
shows its integration into the TI:
Nr. Activity
1.
Patients monitor of weight, heart rate, and
blood pressure daily.
2.
Sensors transfer the vital parameters to the
patients computer.
3.
Patients encrypt the data for their caregiver
and transfer it to the medical server.
4.
The medical service flags the data for the
caregiver and sends a notification.
5.
The physician checks the medical service
and downloads the monitoring record.
6.
The physician decrypts the data each
working day and transfers it to his IS.
7.
The physician validates the data within his
IS and judges the patients health status.
8.
The physician consults the patient
personally, in case it is required due to
monitoring data.
9.
The physician compiles a report and submits
it to the accounting service each quarter.
10.
The service provider downloads all reports
and inserts measures in the overall
monitoring sheet.
11.
The service provider compiles a report and
transfers it to the health insurance.
Table 1 Telemonitoring Use Case
Physician
Max Mustermann (Q1 2011)
Compliance 92%
Hospitalisierung 2 Tage
Arbeitsausflle 3 Tage
HI-Behandlungen 13 EBM
Service Provider
Patient
750 Patients (Q1/2011)
Compliance 87 %
Hozpitalization 347 Days
Lack of Work 473 Days
CHF-Treatment 5742 EBM
Max Mustermann (Q1 2011)
Compliance 92%
Hozpitalization 2 Days
Lack of Work 3 Days
CHF-Treatment 13 EBM
50
70
90
110
130
150
Herzfrequenz (S/Min) Gewicht (KG)
Blutdruck(Dias, mmHg) Blutdruck (Sys, mmHg)
Max. 750
Datasets per
Quarter
Max. 31 Data
sets monthly
Health Insurance
Participant
Max Mustermann
n
One Report
per Quarter
Max Mustermann
Datum 01.01.2011
Gewicht 92 kg
Herzfrequenz 60 Schlge/Min.
Blutdruck (Sys) 123 mmHg
Blutdruck (Dia) 87 mmHg
Registration
once a year
Max Mustermann
Date 01/01/2011
Weight 92 kg
Heart Rate 60 bpm
Blood Pressure (Sys) 123 mmHg
Blood Pressure (Dia) 87 mmHg
957
Figure 4 Communication structur
The implementation is based on
centralized web services. These are
physician network due to caregivers di
institutions and health insurances conce
health related data [7]. The health
encrypted communication between
physicians, while the accounting servi
communication between the service p
caregivers. Service-oriented device
sensors is possible [26], as the data is e
eHC and decrypted with the physicians
to the description in section 4.2.
6.2. Business Structure
The business structure was a
described in section 4.1 and reflects th
fees to regulate the market in order
desired outcomes [31]. In our case, the
an adverse flow of the transaction objec
the previous chapter. Monitoring info
are paid within this structure by the h
encouraging physicians and patients
document the CHF prevention t
prevention is potentially more efficien
of CHF, the health insurances wa
treatment funds of CHF to th
telemonitoring. A contract betwee
providers and the health insurance i
adjusted to support this objective in th
manner. In the first year of the telemon
(period t
1
) the health insurance is not
the savings to be achieved by telemon
however, the cost of CHF for the
re
SOA, with two
hosted by the
istrust of private
erning storage of
service allows
patients and
ice supports the
provider and the
integration of
encrypted by the
s HPC according
already roughly
he payments and
to achieve the
financial flow is
cts, developed in
ormation objects
health insurance,
to perform and
thoroughly. As
nt than treatment
ant to redirect
he market for
en the service
is designed and
he best possible
nitoring contract
able to estimate
nitoring exactly,
preceding year
(period t
0
) can be quantified by
spending for CHF treatment
ambulatory care. To allocate funds
and initiate the market, the potenti
in the studies are taken as the calc
following year. The initial fund fo
allocate one third of all CHF-relate
approximately reflects the estim
Generally, annual readjustments
ensure that the savings achieved in
(t
n-1
) are distributed to the stakeho
period (t
n
). The annual spending f
the total treatment costs in ambula
in EBM, and the hospital cases rela
In Germany health insurances p
hospital cases based on a diagno
different hospital cases priced b
4242 [14] covering all hospital
exceptions [23]. Furthermore, cer
medication in ambulatory care can
CHF and quantified in an EBM-
Savings in the later periods result
of treatments in the actual period i
reference period before the
telemonitoring (Formula 1).
Saving t
n
= CostCHF
to
-
(EBN
to
- EBN
(Bospital Cases
t0
- Bos
Formula 1 Calculation of sav
Lack of work and medication re
included into the savings gained b
market. The items are neglected
inclusion of employers would
medication data was not availabl
Additionally, an adjustment factor
of CHF in period t
0
might be ne
cost for CHF increases continu
demographic shift in Germany.
Service providers will pay parts
calculated in formula 1 to caregive
distribution of the savings among t
agreed to be 30% for physicians an
The allowance for physicians (for
the sum of all savings achieved f
telemonitoring. Each summand con
of their gain sharing (0.3), their co
the savings, divided by the paymen
agreed. In our case the allowance in
times (each quarter) and will be
which was estimated to be 3,0
reviewing the past
in hospitals and
for the first year (t
1
)
ial savings measured
culation base for the
for the period t
1
will
ed costs in t
0
, as this
mated saving [15].
of the market will
n the previous period
olders in the current
for CHF result from
atory care, measured
ated caused by CHF.
pay allowances for
osis. CHF has three
between 2382 and
expenses with little
rtain treatments and
n be associated with
-value directly [15].
from the difference
in comparison to the
establishment of
CostCHF
tn
=
N
tn
) +
spital Cases
tn
)
ings in t
n
elated to CHF can be
y the telemonitoring
for now, since an
be necessary and
le during the study.
r for the initial costs
cessary because the
uously due to the
s of the total savings
ers and patients. The
the stakeholders was
nd 12% for patients.
rmula 2) is therefore
for their patients by
nsists of the product
ompliance factor and
nt division, which is
n t
1
will be paid four
30% of the saving,
000. In case of full
958
compliance (> 80%), the compliance factor is agreed to
be 1. This would lead to a quarterly amount of 225
per patient and 900 over the whole year. With the
estimated treatment of three patients, a total amount of
2700 could be earned, if all patients of the region
subscribed to telemonitoring and participated with high
compliance.
Formula 2 Allowance caregivers in t
1
The allowance for the first transaction object, the
vital parameters transferred from patients to their
physicians, is paid on a monthly basis to the patients by
deducting it from the monthly insurance premium or
the extra premium (formula 3). Patients are paid 12%
of initial savings (gain sharing = 0.3) in t
1
if they reach
a compliance factor of one.
Formula 3 Allowance patients in t
1
In period t
2
the whole process will be adjusted
according to the market results. These are determined
by the behavior of the market participants [31].
Currently the market model expects that the saving
potential is high enough to ensure a sustainable
telemonitoring of CHF without extra funds from the
health insurance. Other cased might require extra
funds, but the medical use could justify the allocation
also in such cases.
7. Conclusion
The German health system has currently no regular
market model for e-health. The paper illustrated how
health insurances and physician networks can create a
market for electronic health services, to harvest the
benefits identified in clinical studies. Allocating funds
for e-health solutions within a market engineering
approach can create a well defined market, including
secure transaction objects and predefined transaction
services. Medical studies can be employed at first to
estimate the initial efforts and long term saving
potentials, which can be achieved by e-health
applications. In case of CHF existing studies indicate
that potential fund savings are sufficient to finance a
new market just by the increase in treatment efficiency.
The case study has a facilitating environment, as a big
physician network could encourage the caregivers of a
region to participate in a pilot project. Further, they can
sign contracts for multiple caregivers, which is difficult
to achieve for single physicians or small physician
networks. Since close contact already existed between
health insurances and the physician network, there was
an organized exchange between the important
stakeholders. The approach is not necessarily limited to
telemonitoring, as market engineering needs to
consider several specific aspects and is therefore
difficult to generalize. In any case, market engineering
approaches seem to be an approach to create
sustainable business models for e-health applications
and overcome the low adoption of information
technology in healthcare. Successful pilots can move
successful e-health applications to the regular
allowance portfolio of the health insurance.
7.1. Limitations
The current state of the German TI does not yet
allow for a setup according to the microstructure
suggested in this paper for all caregivers in Germany.
Therefore, an extended roll-out of the TI must be
ensured in order to enable such a setup on a regular
base. It must be further ensured that necessary
treatments, medications or hospitalizations are not
neglected due to the financial incentive mechanism.
Lack of work could not be included in the market, as
companies were not yet asked to support the utilization
of e-health solutions. Also it is currently legally
difficult to pay allowance directly to patients with
chronic diseases, a benefit which healthy patients do
not receive.
7.2. Further research
Within the research project specification, set up and
evaluation of the market for telemonitoring is the
upcoming target. Furthermore it is necessary to fix the
catalogue of CHF-related treatments and medication to
specify the model in detail. As the region will be a
testbed for the eHC in 2012, the solution can be piloted
before a possible roll-out in other parts of Germany.
The effect of the market on the adoption of
telemonitoring solutions will be an interesting subject
of research as well as the adjustment of the market
parameters after the first evaluation of the market
results.
7.3. Contribution to Theory
The case of telemonitoring illustrates how a regular
incentive model for the development and diffusion of
e-health solutions can be achieved within a public
health system. The presented case study illustrates a
process on how to translate promising clinical studies
959
for e-health applications into transaction objects and
allocate funds to stimulate the transmission of this
information. The creation of the market for information
objects requires initial funds in period t
1
; these can be
derived from clinical studies and economical
information. The evaluation on the information objects
in period t
n
leads to a readjustment of the technology.
Hence, the method adopts a general market
engineering approach to the case of e-health in
ambulatory care.
8. Acknowledgment
The market engineering case study was conducted
in the context of the research project Nutzen und
Sicherheit der elektronischen Gesundheitskarte in der
Baymatik (NuSiB) in cooperation with the physician
network GO IN located in the region of Ingolstadt. The
project is funded by the Bavarian Ministry of
Environment and Health.
9. References
[1] J. M. Aranaz-Andrs, C. Aibar-Remn and J. Vitaller-
Murillo, "Incidence of adverse events related to health care in
Spain: results of the Spanish National Study of Adverse
Events", Journal of Epidemiology and Community Health,
62: (2008), pp. 1022-1029.
[2] rztliches Zentrum fr Qualitt in der Medizin, Nationale
VersorgungsLeitlinie Chronische Herzinsuffizienz,
Bundesrztekammer, Kassenrztliche Bundesvereinigung,
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen
Fachgesellschaften, Berlin, 2009.
[3] F. Becker, "Explorative Forschung mittels Bezugsrahmen
- ein Beitrrag zur Methodologie des
Entdeckungszusammenhangs", Empirische
Personalforschung: Methoden und Beispiele, 111-127
(1993).
[4] J. Bortz and N. Dring, Forschungsmethoden und
Evaluation fr Human- und Sozialwissenschaftler, Springer,
Berlin, 2002.
[5] Bundesministerium fr Gesundheit, The German eHealth
Strategy (Target and strategy, concept, legal framework,
activities/roll-out plan, costs and return of investment,
European perspective), Berlin/Bonn, 2005.
[6] Bundesrepublik Deutschland, Sozialgesetzbuch (SGB)
Fnftes Buch, Gesetzliche Krankenversicherung, 1988.
[7] S. Dnnebeil, A. Sunyaev, J. M. Leimeister and H.
Krcmar, Strategies for development and adoption of EHR in
German ambulatory care, 4th International Conference on
Pervasive Computing Technologies for Healthcare
(PervasiveHealth), IEEE, Munich, 2010, pp. 1-8.
[8] K. M. Eisenhardt, "Building Theories from Case Study
Research", Academy of Management Research, 14 (1989),
pp. 532-550.
[9] European Comission, Business Models for eHealth, in I.
f. H. Unit, ed., European Commission DGINFSO ICT for
Health, Luxembourg, 2010, pp. 44-47.
[10] European Comission, EuropischeUnion (2007) -
eHealth for Safety Report, in O. f. O. P. o. t. E. Communities,
ed., Luxembourg, 2007.
[11] Fraunhofer Institut, Spezifikation der Lsungsarchitektur
zur Umsetzung der Awendungen der elektronischen
Gesundheitskarte, Fraunhofer, Projektgruppe FuE-Projekt,
2005.
[12] gematik, Einfhrung der Gesundheitskarte -
Gesamtarchitektur, gematik GmbH, 2008.
[13] gematik, bergreifendes Sicherheitskonzept der
Telematikinfrastruktur, Specification, 2008.
[14] W. Hellmann and S. Eble, Ambulante und Sektoren
bergreifende Behandlungspfade: Konzepte / Umsetzung /
Praxisbeispiele, 2009.
[15] T. Helms, J. Pelleter and D. Ronneberger,
"Telemedizinische Betreuung chronisch herzinsuffizienter
Patienten am Beispiel des telemedizinischen
Patientenbetreuungs- und -schulungsprogramms
Telemedizin frs Herz", Herz, 32 (2007), pp. 623-629.
[16] HFA, berwachung der Herzinsuffizienz Tabelle fr
die Kontrolle der Krankheitszeichen, Heart Failure
Association of the European Society of Cardiology, 2010.
[17] IOM, Identifying and Preventing Medication Errors -
Institute of Medicine, in INSTITUTE OF MEDICINE OF
THE NATIONAL ACADEMIES, ed., THE NATIONAL
ACADEMIES PRESS, Washington D.C., 2006.
[18] J. Karette, K. Neumann, F. Kainzinger and K. Henke,
Innovation und Wachstum im Gesundheitswesen, in R.
Berger, ed., Mnchen, 2005.
[19] K. Kempf and C. Schulz, Telemedizin bei Diabetes:
Hhere Therapiezufriedenheit, verbesserte
Stoffwechselparameter, DiabetivaR Studie Monika Dienstle,
WDGZ, 2008.
[20] H. Krum and W. T. Abraham, "Heart failure", The
Lancet, 373 (2009), pp. 941-955.
[21] KVB, Grunddaten zur vertragsrztlichen Versorgung in
Deutschland, in K. Bundesvereinigung, ed., Berlin, 2008.
[22] J. M. Lapp, J. B. Muhlestein, D. L. Lapp, R. S.
Badger, T. L. Bair, R. Brockman, T. K. French, L. C.
Hofmann, B. D. Horne, S. Kralick-Goldberg, N. Nicponski,
J. A. Orton, R. R. Pearson, D. G. Renlund, H. Rimmasch, C.
Roberts and J. L. Anderson, "Improvements in 1-Year
Cardiovascular Clinical Outcomes Associated with a
Hospital-Based Discharge Medication Program", Annals of
Internal Medicine, 141 (2004), pp. 446-453.
[23] M. Lisac, L. Reimers, K.-D. Henke and S. Schlette,
"Access and choice - competition under the roof of solidarity
960
in German health care: an analysis of health policy reforms
since 2004", Health Economics, Policy and Law, 5 (2010),
pp. 31-52.
[24] T. W. Malone, J. Yates and R. I. Benjamin, "Electronic
markets and electronic hierarchies", Commun. ACM, 30
(1987), pp. 484-497.
[25] M. Marschollek and E. Demirbilek, "Providing
longitudinal health care information with the new German
Health Card - a pilot system to track patient pathways",
Computer Methods and Programs in Biomedicine, 81 (2006),
pp. 266-271.
[26] C. Mauro, A. Sunyaev, J. M. Leimeister and H. Krcmar,
Service-orientierte Integration medizinischer Gerte- eine
State of the Art Analyse, Wirtschaftsinformatik, Vienna,
2009, pp. 119-128.
[27] T. Neumann, J. Biermann, A. Neumann, J. Wasem, G.
Ertl, R. Dietz and R. Erbel, "Herzinsuffizienz: Hufigster
Grund fr Krankenhausaufenthalte", Deutsches rzteblatt,
106 (2009), pp. 269-275.
[28] OECD, OECD Health Data 2010: Statistics and
Indicators, in Directorate for Employment Labour and Social
Affairs, ed., 2010.
[29] P. Shekelle, S. C. Morton and E. B. Keeler, Costs and
Benefits of Health Information Technology, Evidence Report
- Technology Assessment, 2006, pp. 1-71.
[30] P. C. Smith, A. Stepan, V. Valdmanis and P. Verheyen,
"Principal-agent problems in health care systems: an
international perspective", Health Policy, 41 (1997), pp. 37-
60.
[31] C. Weinhardt, B. Schnizler and S. Luckner, "Market
Engineering", WIRTSCHAFTSINFORMATIK, 45 (2003),
pp. 635-640.
[32] ZTG, Testregionen in Deutschland, Zentrum fr
Telematik im Gesundheitswesen GmbH, 2009.
961
You might also like
- Digital MedicineFrom EverandDigital MedicineArthur AndréNo ratings yet
- Principles Based Medical Informatics For Success NTDocument4 pagesPrinciples Based Medical Informatics For Success NTSvlader Reitef VanquisherNo ratings yet
- Information Technology Will Save Health Care: Institute of MedicineDocument7 pagesInformation Technology Will Save Health Care: Institute of MedicineKelvin Kurt B. AgwilangNo ratings yet
- TEMPEST: An Integrative Model For Health Technology AssessmentDocument15 pagesTEMPEST: An Integrative Model For Health Technology AssessmentRui AlmeidaNo ratings yet
- Tecnology 1Document7 pagesTecnology 1Anwaar JamalNo ratings yet
- ICT+in+healtcare OrangeDocument4 pagesICT+in+healtcare OrangeshubhamshklNo ratings yet
- Etelemed 2015 6 50 40284Document6 pagesEtelemed 2015 6 50 40284Martijn VeronNo ratings yet
- User Needs and Requirements Analysis For Big Data Healthcare ApplicationsDocument5 pagesUser Needs and Requirements Analysis For Big Data Healthcare Applicationsপ্রজ্ঞা লাবনীNo ratings yet
- Hgrid: An Economical Model For Mass-Health Care System Using Latest Technology (Grid Computing)Document5 pagesHgrid: An Economical Model For Mass-Health Care System Using Latest Technology (Grid Computing)IJMERNo ratings yet
- EPA02461 Acta Polytechnica 2019 02 163-181Document19 pagesEPA02461 Acta Polytechnica 2019 02 163-181liyun19981234No ratings yet
- ADAPT@AGENT - HOSPITAL: Agent-Based Optimization and Management of Clinical ProcessesDocument23 pagesADAPT@AGENT - HOSPITAL: Agent-Based Optimization and Management of Clinical Processeswalaba06No ratings yet
- Exercise 1Document2 pagesExercise 1TRISHA ISOBELLE ARBOLEDANo ratings yet
- Health Information Technology (HIT) Is "The Application of InformationDocument12 pagesHealth Information Technology (HIT) Is "The Application of InformationRahul GargNo ratings yet
- The Hospital Data Project: Comparing Hospital Activity Within EuropeDocument7 pagesThe Hospital Data Project: Comparing Hospital Activity Within EuropeDamian AlexandraNo ratings yet
- Proposal For An Implementation Framework For DigitDocument18 pagesProposal For An Implementation Framework For DigitAndréNo ratings yet
- ABSTRACT: The Emerging Proliferation of Fragmented: Temitayo - Fagbola@fuoye - Edu.ngDocument21 pagesABSTRACT: The Emerging Proliferation of Fragmented: Temitayo - Fagbola@fuoye - Edu.ngAnonymous jF8rU5No ratings yet
- Improving Sustainable Mobile Health Care Promotion - A Novel HybridDocument29 pagesImproving Sustainable Mobile Health Care Promotion - A Novel HybridojuNo ratings yet
- Moroccan Electronic Health Record System: Houssam BENBRAHIM, Hanaâ HACHIMI and Aouatif AMINEDocument8 pagesMoroccan Electronic Health Record System: Houssam BENBRAHIM, Hanaâ HACHIMI and Aouatif AMINESouhaïla MOUMOUNo ratings yet
- Artificial Intelligence in Medical Application: Electrical and Electronic Engineering DepartmentDocument18 pagesArtificial Intelligence in Medical Application: Electrical and Electronic Engineering Departmentمهيمن الابراهيميNo ratings yet
- Remote Health Monitoring of Elderly Through Wearable SensorsDocument26 pagesRemote Health Monitoring of Elderly Through Wearable SensorsAkansha SinghNo ratings yet
- 5 FuscoDocument10 pages5 FuscoZarah Alifani DzulhijjahNo ratings yet
- Doh2011 2013isspDocument191 pagesDoh2011 2013isspJay Pee CruzNo ratings yet
- Mhealth ReportDocument101 pagesMhealth ReportSteveEpsteinNo ratings yet
- E-Procurement in Hospital Pharmacies: An Exploratory Multi-Case Study From SwitzerlandDocument16 pagesE-Procurement in Hospital Pharmacies: An Exploratory Multi-Case Study From SwitzerlandPrudhvinadh KopparapuNo ratings yet
- HIS Implementation GuideDocument11 pagesHIS Implementation GuideJohn stevensonNo ratings yet
- P.kierkegaarde PrescriptionacrossEuropeDocument16 pagesP.kierkegaarde PrescriptionacrossEuropeseptiman zebuaNo ratings yet
- Digital HealthDocument5 pagesDigital HealthGloheal Test5No ratings yet
- E-Prescription Across Europe: Health and Technology September 2013Document16 pagesE-Prescription Across Europe: Health and Technology September 2013ifrahNo ratings yet
- Overview of ReportsDocument4 pagesOverview of ReportsMuhammad UmerNo ratings yet
- Role of ICT For HealthcareDocument13 pagesRole of ICT For HealthcareDejen AgaziuNo ratings yet
- 10 1 1 199Document10 pages10 1 1 199Pavel TudorNo ratings yet
- Covid + Digital TechDocument8 pagesCovid + Digital TechgraceNo ratings yet
- Implementation of EMRs, NigeriaDocument17 pagesImplementation of EMRs, NigeriaAsmamaw K.No ratings yet
- 1 PBDocument15 pages1 PBYat SonNo ratings yet
- Review Paper On Healthcare Monitoring SystemDocument9 pagesReview Paper On Healthcare Monitoring SystemEditor IJRITCCNo ratings yet
- HIMSS E-Health SIG White Paper: Access, Efficiency, Effectiveness, and Quality Improve The Health Status of PatientsDocument23 pagesHIMSS E-Health SIG White Paper: Access, Efficiency, Effectiveness, and Quality Improve The Health Status of PatientsSyed NasrullahNo ratings yet
- Design and Customization of Telemedicine SystemsDocument16 pagesDesign and Customization of Telemedicine SystemsNg Yi XuanNo ratings yet
- Research Article: Design and Customization of Telemedicine SystemsDocument17 pagesResearch Article: Design and Customization of Telemedicine SystemsBayu PrabuNo ratings yet
- Thesis Electronic Medical RecordsDocument6 pagesThesis Electronic Medical Recordscarmenmartinezmcallen100% (1)
- Official Lecture#4 - Overview of Health InformaticsDocument3 pagesOfficial Lecture#4 - Overview of Health InformaticsLYKA ANTONETTE ABREGANANo ratings yet
- DichDocument4 pagesDichngocphh.35No ratings yet
- Medicine of The Future Digital Technologies in HeaDocument10 pagesMedicine of The Future Digital Technologies in Heaeva kacanjaNo ratings yet
- Redp 4691Document34 pagesRedp 4691tonocovarruNo ratings yet
- Articulo en InglesDocument34 pagesArticulo en InglesJESUS GABRIEL VILLARREAL CUELLONo ratings yet
- Patient Information Systems in The LiteratureDocument6 pagesPatient Information Systems in The LiteratureJohn MunaonyediNo ratings yet
- AmirLatif2020 Article ARemixIDESmartContract-basedFrDocument24 pagesAmirLatif2020 Article ARemixIDESmartContract-basedFrDivya KandpalNo ratings yet
- Discussion Paper On Semantic and Technical InteroperabilityDocument7 pagesDiscussion Paper On Semantic and Technical InteroperabilityΜΙΚΕNo ratings yet
- Role of ICT in HealthcareDocument19 pagesRole of ICT in HealthcareRama VenugopalNo ratings yet
- Ecommerce's Important Role in The Medical Sector: Luzanna Fung Lok Chee and Rashad YazdanifardDocument8 pagesEcommerce's Important Role in The Medical Sector: Luzanna Fung Lok Chee and Rashad YazdanifardAsora Yasmin snehaNo ratings yet
- LIMBAH MEDIS klmpk5Document9 pagesLIMBAH MEDIS klmpk5Hesti FinoNo ratings yet
- Software Engineering in HealthcareDocument5 pagesSoftware Engineering in HealthcareIJRASETPublicationsNo ratings yet
- Implementing Telemedicine in Afghanistan-Challenges and Issue1Document6 pagesImplementing Telemedicine in Afghanistan-Challenges and Issue1Muhibullah AmanNo ratings yet
- Potsdam ConferenceDocument21 pagesPotsdam ConferenceheeducationalservicesNo ratings yet
- Project ProposalDocument9 pagesProject ProposalMike Mwesh BernardNo ratings yet
- It in Health CareDocument8 pagesIt in Health CareAnnonymous963258No ratings yet
- Cybersecurity Match Supply and Demand in Portuguese HealthCare Sector Industry Collaboration - Reviewed FinalDocument13 pagesCybersecurity Match Supply and Demand in Portuguese HealthCare Sector Industry Collaboration - Reviewed FinalRui GomesNo ratings yet
- Bluemine - Applying Analytics in HealthcareDocument16 pagesBluemine - Applying Analytics in HealthcareRaam MkNo ratings yet
- TelemedicineDocument6 pagesTelemedicineMarcNo ratings yet
- Proposed System Using Iot and Gis To Generate Electronic Medical RecordsDocument11 pagesProposed System Using Iot and Gis To Generate Electronic Medical Recordsindex PubNo ratings yet
- Suspension Block AssemblyDocument1 pageSuspension Block AssemblymamatnamakuNo ratings yet
- Derailleur Chain Tensioner Idlers Etc.: Fig CT4Document1 pageDerailleur Chain Tensioner Idlers Etc.: Fig CT4mamatnamakuNo ratings yet
- Toolkit Included in The Toolkit: DATA SHEET: Ds-Toolkit ISSUE S1001Document2 pagesToolkit Included in The Toolkit: DATA SHEET: Ds-Toolkit ISSUE S1001mamatnamakuNo ratings yet
- Retro-Fitting L-Type Mudguards:: Aug-10 Mglret DsDocument4 pagesRetro-Fitting L-Type Mudguards:: Aug-10 Mglret DsmamatnamakuNo ratings yet
- Wheels Rims and Spokes Important Information: DATA SHEET: Ds-Wheel ISSUE S1004Document1 pageWheels Rims and Spokes Important Information: DATA SHEET: Ds-Wheel ISSUE S1004mamatnamakuNo ratings yet
- Brake Lever Setup Important Information Setup Procedure: DATA SHEET: Ds-Brleval ISSUE S1003Document2 pagesBrake Lever Setup Important Information Setup Procedure: DATA SHEET: Ds-Brleval ISSUE S1003mamatnamakuNo ratings yet
- This Luggage Item Is NOT Suitable For Use With A Brompton S-Type ModelDocument2 pagesThis Luggage Item Is NOT Suitable For Use With A Brompton S-Type ModelmamatnamakuNo ratings yet
- These Notes Relate Mainly To Fitting A New Pillar, But They May Also Be Helpful When Exchanging Certain PartsDocument2 pagesThese Notes Relate Mainly To Fitting A New Pillar, But They May Also Be Helpful When Exchanging Certain PartsmamatnamakuNo ratings yet
- Fig GTR1: Aug-10 Gtrigb3 DsDocument3 pagesFig GTR1: Aug-10 Gtrigb3 DsmamatnamakuNo ratings yet
- Lamp Brackets / Battery Lights.: Jan-12 Batlam DsDocument4 pagesLamp Brackets / Battery Lights.: Jan-12 Batlam DsmamatnamakuNo ratings yet
- DJI Spark DesignDocument1 pageDJI Spark DesignmamatnamakuNo ratings yet
- Fibrous JointDocument5 pagesFibrous JointmamatnamakuNo ratings yet
- Derailleur Chain Tensioner Idlers Etc.: Fig CT4Document1 pageDerailleur Chain Tensioner Idlers Etc.: Fig CT4mamatnamakuNo ratings yet
- BS en 14885-2015Document64 pagesBS en 14885-2015mamatnamaku100% (3)
- Xtrail t32Document113 pagesXtrail t32mamatnamakuNo ratings yet
- BS en 16615-2015Document44 pagesBS en 16615-2015mamatnamaku100% (7)
- BS en 16616-2015Document40 pagesBS en 16616-2015mamatnamaku100% (3)
- INTR - Indonesia National Trade Repository PDFDocument4 pagesINTR - Indonesia National Trade Repository PDFmamatnamakuNo ratings yet
- Computer Science: From Wikipedia, The Free EncyclopediaDocument15 pagesComputer Science: From Wikipedia, The Free EncyclopediamamatnamakuNo ratings yet
- Validation EtoDocument8 pagesValidation EtomamatnamakuNo ratings yet
- Virtualization: Old Technology Offers Huge New Potential: Greg GothDocument4 pagesVirtualization: Old Technology Offers Huge New Potential: Greg GothmamatnamakuNo ratings yet
- 1-A Business Model Framework For The Design and Evaluation of Business Models in The Internet of ServicesDocument13 pages1-A Business Model Framework For The Design and Evaluation of Business Models in The Internet of ServicesmamatnamakuNo ratings yet
- Downey L, Lloyd H - Bed Bathing Patients in Hospital - ArticleDocument6 pagesDowney L, Lloyd H - Bed Bathing Patients in Hospital - Articlemamatnamaku100% (1)
- M750 Service ManualDocument78 pagesM750 Service ManualcciprainNo ratings yet
- Oracle HCM Cloud OverviewDocument35 pagesOracle HCM Cloud OverviewAngelVillalobosNo ratings yet
- Element Description Team CharterDocument2 pagesElement Description Team CharterPRASHANT GUPTANo ratings yet
- CMPE 011 Reviewer MidtermsDocument5 pagesCMPE 011 Reviewer MidtermsJohn Rave Manuel GonzalesNo ratings yet
- Module 2 - Physical Presentation of Reports LettersDocument14 pagesModule 2 - Physical Presentation of Reports Lettersashutoshsk5120% (1)
- SMI983Document8 pagesSMI983ade.achielNo ratings yet
- Sunlight StyleGuide DataViz PDFDocument13 pagesSunlight StyleGuide DataViz PDFSai Kiran AdepuNo ratings yet
- Lecture1Document51 pagesLecture1Kimberley Oh100% (1)
- Jual Sokkia SET 350X Total Station - Harga, Spesifikasi Dan ReviewDocument5 pagesJual Sokkia SET 350X Total Station - Harga, Spesifikasi Dan Reviewbramsalwa2676No ratings yet
- Samsung Group: By: Ethel Herna C. PabitoDocument13 pagesSamsung Group: By: Ethel Herna C. PabitoEthel PabitoNo ratings yet
- Buku Standarisasi Spek Mtu PLN - SK Dir 216 (Bus VT)Document1 pageBuku Standarisasi Spek Mtu PLN - SK Dir 216 (Bus VT)PontasNo ratings yet
- Energy Modeling GuidelinesDocument32 pagesEnergy Modeling GuidelinesBrian MayNo ratings yet
- Deep Learning For Audio Signal ProcessingDocument14 pagesDeep Learning For Audio Signal Processingsantoshmore439No ratings yet
- HP Mouse TestDocument8 pagesHP Mouse Testradiophon666No ratings yet
- EpayDocument17 pagesEpayShrinivas PrabhuneNo ratings yet
- Guide: Performance Optimization For The Galileo 10 Runtime SystemDocument15 pagesGuide: Performance Optimization For The Galileo 10 Runtime Systemvaldemir huculakNo ratings yet
- Evault MAX 80128223 UL 9540A Test ReportDocument38 pagesEvault MAX 80128223 UL 9540A Test Reportjaikp56No ratings yet
- Solar SystemsDocument23 pagesSolar SystemsRaghavendra RaghavNo ratings yet
- BS 6349-2Document64 pagesBS 6349-2medianna100% (6)
- NEXYGENPlus Spec SheetDocument3 pagesNEXYGENPlus Spec Sheetrossifam777No ratings yet
- Forza XADV 750 - 2021 Program SmartkeyDocument8 pagesForza XADV 750 - 2021 Program SmartkeyAny TimNo ratings yet
- Brochure Liebert ITA Series (5-20KVA)Document4 pagesBrochure Liebert ITA Series (5-20KVA)kimxoNo ratings yet
- Migrate MySQL Database To Azure Database For Mysql OnlineDocument11 pagesMigrate MySQL Database To Azure Database For Mysql Onlinethecoinmaniac hodlNo ratings yet
- Lab Report No 10ADCDocument4 pagesLab Report No 10ADCIhsan ul HaqNo ratings yet
- Machine Learning Lab Manual 8Document12 pagesMachine Learning Lab Manual 8Raheel AslamNo ratings yet
- Non Volatile MemoryDocument16 pagesNon Volatile MemoryvinutkumarNo ratings yet
- 190-01499-00 - F - Pilot GuideDocument34 pages190-01499-00 - F - Pilot GuideFordiNo ratings yet
- Section 1 - Paperi-General Knowledge and Current Affairs: Set Id: 53449 - 6Document19 pagesSection 1 - Paperi-General Knowledge and Current Affairs: Set Id: 53449 - 6babluNo ratings yet
- Mihai Nicusor: Curriculum Vitae Replace With First Name(s) Surname(s)Document2 pagesMihai Nicusor: Curriculum Vitae Replace With First Name(s) Surname(s)Nicusor MihaiNo ratings yet
- 3bhs212794 E01 Revn User Manual Acs6000Document266 pages3bhs212794 E01 Revn User Manual Acs6000Fernando RamirezNo ratings yet