Professional Documents
Culture Documents
Gastrointestinal System and Nutrition Drug Charts
Uploaded by
NursingSchoolNotesOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gastrointestinal System and Nutrition Drug Charts
Uploaded by
NursingSchoolNotesCopyright:
Available Formats
Gastrointestinal System and Nutrition
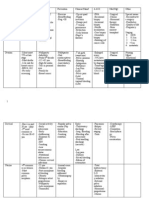
Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs Histamine-Receptor Antagonists Suppress action of gastric acid by blocking H2 receptors in parietal cells in stomach Gastric and peptic ulcers, GERD, hypersecretory conditions May decrease libido, CNS effects such as lethargy, depression, confusion Can increase levels of warfarin, dilantin, theophylline, lidocaine Advise clients to eat small meals, avoid ASA and NSAIDS, Cimetridine (Tagamet), ranitidine hydrochloride (Zantac), famotidine (Pepcid)
Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Mucosal Protectant Protects ulcer from further injury by changing sucralfate into a thick substance that covers ulcers Duodenal ulcers, maintenance therapy Constipation Sucralfate may interfere with absorption of phenytoin, digoxin, warfarin, cipro Must increase dietary fiber intake to reduce constipation Sucralfate (Carafate)
Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Antacids Neutralize gastric acid and inactivate pepsin Peptic ulcer disease, promoting and relieving pain, GERD Constipation, (magnesium compounds cause diarrhea), Aluminum compounds bind to wafarin and tetracycline and interfere with absorption Medications at least 1 hour before or after antacid use Alumnum hydroxide (Amphojel), magnesium hydroxide (milk of magnesia)
Name Mechanism of Action
Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Prostaglandin Analog Acts as endogenous prostaglandin in GI tract to decrease acid secretion, increase bicarbonate and protective mucus, promote vasodilation to maintain submucosal blood flow For clients on long term NSAID therapy to prevent ulcers, cervical ripening to induce labor Diarrhea, dysmenorrhea Take at bedtime. Misoprostol (Cytotec)
Name Types/Mechanism of Action
Antiemetics, many different types. Glucocorticoids: unknown mechanism ( dexamethason) Substance P/neurokinin antagonists: inhibits aprepitant (Emend) Serotonin antagonists: prevents emesis by blocking the serotonin receptors in chemoreceptors zone (Zofran) Dopamine antagonists: blockade of dopamine (Reglan) Cannabinoids: unknown mechanism (Marinol) Antihistamine (Dramamine) Benzodiazepines (Ativan) (Valium)
Name Mechanism of Action
Therapeutic Uses
Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Laxatives Bulk forming: soften fecal mass and increase bulk (identical to fiber) Surfactant laxatives: lower surface tension of stool Stimulant Laxatives: stimulation of intestinal peristalsis Osmotic laxatives: draw water into intestine, results in peristalsis Bulk forming: decrease diarrhea in cases of diverticulosis or IBS Surfactant: for constipation, prevention of hemorrhoids/straining Stimulant: preparation for specific surgeries, short term treatment for constipation Osmotic: prevent painful elimination, surgery, rapid evacuation if poison is ingested . GI upset, rectal burning, accumulation of magnesium, fluid retention, or dehydration depending on type used Milk and antacids can destroy enteric coating of bisacodyl Maintain adequate hydration Metamucil, Colace, Dulcolax, Milk of Magneisa
Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Antidiarrheals Activate opioid receptors in GI tract to decrease intestinal motility specific uses such as diarrhea caused by bacteria or nonspecific for symptoms CNS effects can be present at high doses (euphoria or CNS depression) Alcohol/ CNS depressants may enhance CNS depression Fluid intake to maintain electrolytes, Caffeine exacerbates diarrhea by increasing GI motility Loperamide (Imodium), difenoxin (Motofen)
Medication for Irritable Bowel Syndrome with diarrhea: alosetron (Lotronex), selective blockade of 5-HT3 receptors, result is increase firmness in stool and decrease urgency. Medication for Irritable Bowel Syndrome with constipation: lubiprostone (Amitiza), increases fluid secretion in the intestine to promote motility Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs 5 Aminosalicylates Decrease inflammation by inhibiting prostaglandin synthesis Inflammatory bowel disease such as Crohns disease or ulcerative colitis Agranulocytosis, anemia None 4 does divided throughout the day Sulfasalazine (Axulfidine) Glucocorticoids Immunosuppresants such as Imuran Immunomodulators such as Remicade Antibiotics such as metronidazole (Flagyl)
Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Iron Provide iron needed for RBC development and oxygen transport Iron deficiency anemia GI distress (constipation), teeth staining, anaphylaxis risk, hypotension Antacids and tetracyclines reduces absorption of iron Iron is poorly absorbed by body, so large amounts are needed. Increase in hemoglobin of 2 g/dl expected one month after beginning therapy Ferrous sulfate (Feosol)
Name Mechanism of Action
Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Vit B 12 Necessary to convert folic acid in inactive form to its active form. Loss of intrinsic factor within cells of stomach causes inability to absorb vit B12 so supplementation is necessary in high doses Vitamin B12 deficiency, megaloblastic anemia Hypokalemia secondary to increased RBC production Concurrent administration of folic acid may mask symptoms of deficiency of B12 Signs of B12 deficiency: beefy red tongue, pallor, neuropathy B12
Name Mechanism of Action Therapeutic Uses Side Effects/Precautions Interactions Nursing/Patient Teaching Common Drugs
Folic acid Essential in production of DNA and erythropoiesis (RBC, WBC, platelets) Treatment of megaloblastic anemia, prevention of neural tube defects Indiscriminate use of folic acid is not appropriate because it mask the symptoms of B12 deficiency Decreased levels with use of sulfonamides, sulfasalazine, methotrexate Green leafy veg and liver are high in folic acids, Folate level should be between 6 15 mcg/ml Folic acid
You might also like
- ECG StripsDocument5 pagesECG StripsNursingSchoolNotes100% (1)
- Pain Med ChartsDocument4 pagesPain Med ChartsNursingSchoolNotesNo ratings yet
- Adult III Cardiac Study GuideDocument15 pagesAdult III Cardiac Study GuideNursingSchoolNotes100% (6)
- Neuro Study GuideDocument7 pagesNeuro Study GuideNursingSchoolNotes100% (2)
- Cardiac Med ChartsDocument6 pagesCardiac Med ChartsNursingSchoolNotes100% (15)
- Resp Lecture NotesDocument17 pagesResp Lecture NotesNursingSchoolNotes100% (3)
- Common Drugs ChartDocument15 pagesCommon Drugs Chartforminsko100% (1)
- Endocrine NursingDocument2 pagesEndocrine Nursingsurviving nursing school100% (2)
- Med Surg Study GuideDocument27 pagesMed Surg Study Guidetrifecta31No ratings yet
- Veterinary Anatomy Coloring BookDocument53 pagesVeterinary Anatomy Coloring BookRamon Gonzalez SayleNo ratings yet
- AntidotesDocument2 pagesAntidotesYemaya84No ratings yet
- Psych Med ChartsDocument5 pagesPsych Med ChartsNursingSchoolNotes100% (5)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Endocrine Disorders (Study Notes)Document11 pagesEndocrine Disorders (Study Notes)Danelle Harrison, RN90% (10)
- Endocrine Study QuestionsDocument16 pagesEndocrine Study QuestionsAcjdd143No ratings yet
- Digestive System PowerPointDocument35 pagesDigestive System PowerPointcelineNo ratings yet
- Cardiovascular: Common Lab Tests For Cardiovascular DisordersDocument49 pagesCardiovascular: Common Lab Tests For Cardiovascular Disorderssarasmith1988No ratings yet
- Gastrointestinal SystemDocument8 pagesGastrointestinal Systemtheglobalnursing100% (1)
- Cardiovascular System Acronyms and MnemonicsDocument18 pagesCardiovascular System Acronyms and Mnemonicsdecsag06No ratings yet
- Medsurg Test 4Document11 pagesMedsurg Test 4Tori RolandNo ratings yet
- Neuro Study GuideDocument11 pagesNeuro Study GuideEllen Hennings100% (1)
- GI Study GuideDocument11 pagesGI Study GuideNursingSchoolNotes75% (4)
- GI Study GuideDocument11 pagesGI Study GuideNursingSchoolNotes75% (4)
- Electrolyte ChartDocument2 pagesElectrolyte ChartJenny Varghese100% (4)
- Cholinergics and AnticholinergicsDocument5 pagesCholinergics and AnticholinergicscatislandbigredNo ratings yet
- Electrolytes ImbalancesDocument4 pagesElectrolytes ImbalancesPeter John Ruiz100% (1)
- 37 Cardiac Problems PDFDocument9 pages37 Cardiac Problems PDFsarasmith1988No ratings yet
- Cardiovascular Med Surg Memory Notebook of NursingDocument8 pagesCardiovascular Med Surg Memory Notebook of NursingdmsapostolNo ratings yet
- Adam's Respiratory Study GuideDocument5 pagesAdam's Respiratory Study GuideNursingSchoolNotesNo ratings yet
- Cardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsDocument4 pagesCardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsJessica100% (1)
- Nursing Pharmacology Perfusion Study GuideDocument9 pagesNursing Pharmacology Perfusion Study GuideChelsea SmithNo ratings yet
- Nursing Pharmacology Inflammation Study GuideDocument11 pagesNursing Pharmacology Inflammation Study GuideChelsea Smith100% (1)
- Acid Base Self Study With Practice QuestionsDocument13 pagesAcid Base Self Study With Practice QuestionsfriendofnurseNo ratings yet
- Chart of Neuro DisordersDocument1 pageChart of Neuro DisordersNursingSchoolNotes100% (2)
- Physiologic Changes of Aging: System AlterationDocument1 pagePhysiologic Changes of Aging: System Alterationshenric16100% (1)
- ENDOCRINE NURSING-FINAL HDDocument15 pagesENDOCRINE NURSING-FINAL HDJayvee Novenario Casaljay100% (1)
- Hematology QuestionsDocument7 pagesHematology QuestionsRaven Atisha100% (1)
- Communicablediseases 110227001506 Phpapp02 PDFDocument30 pagesCommunicablediseases 110227001506 Phpapp02 PDFCrystal Ann Monsale TadiamonNo ratings yet
- Endocrine Study GuideDocument4 pagesEndocrine Study GuideNursingSchoolNotes100% (1)
- MCQ Congenital Intestinal ObstructionDocument6 pagesMCQ Congenital Intestinal ObstructionAmrut LovesmusicNo ratings yet
- Pharmacology A ReviewDocument15 pagesPharmacology A ReviewKathrynne MendozaNo ratings yet
- 3.26.12 Treatment of GI DisordersDocument6 pages3.26.12 Treatment of GI DisordersDiana Hylton100% (4)
- Pedia NotesDocument7 pagesPedia NotesFreeNursingNotes100% (1)
- Study Guide Med Surg #1Document22 pagesStudy Guide Med Surg #1cfunk929No ratings yet
- Case Study - Age PediaDocument81 pagesCase Study - Age PediaKryssel Delos Reyes SantosNo ratings yet
- Cardiac Stuff That You Have To MemorizeDocument1 pageCardiac Stuff That You Have To MemorizeNursingSchoolNotes100% (1)
- OB Drug ChartsDocument2 pagesOB Drug ChartsNursingSchoolNotesNo ratings yet
- Pulmonary Med Charts Part 2Document2 pagesPulmonary Med Charts Part 2NursingSchoolNotes100% (3)
- Drugs WorksheetDocument16 pagesDrugs Worksheetninja-2001No ratings yet
- Acute Renal Failure-Student-Rapid ReasoningDocument4 pagesAcute Renal Failure-Student-Rapid Reasoningapi-268403950No ratings yet
- Fluids and Electrolytes ConceptDocument31 pagesFluids and Electrolytes ConceptDarwin AndalNo ratings yet
- Pharmacology Questions CardiacDocument5 pagesPharmacology Questions CardiacAmanda SimpsonNo ratings yet
- NLE Poisons and AntidotesDocument2 pagesNLE Poisons and AntidotesGodfrey Franco100% (1)
- A-T-I Endocrine NotesDocument3 pagesA-T-I Endocrine NotesKelseyAnnBarnesNo ratings yet
- MedSurg CH 44 & 45 Study GuideDocument5 pagesMedSurg CH 44 & 45 Study GuideMichele ShepardNo ratings yet
- Cardiovascular Pharmacology OutlineDocument11 pagesCardiovascular Pharmacology OutlineLhay de OcampoNo ratings yet
- Exam 2 - Neurological Study GuideDocument10 pagesExam 2 - Neurological Study GuideStephanieNo ratings yet
- Digestive Domain Guide 1Document31 pagesDigestive Domain Guide 1surviving nursing school100% (1)
- Urinary EliminationDocument7 pagesUrinary EliminationJeityynnee Tubeo100% (1)
- Dysrhythmias NotesDocument23 pagesDysrhythmias NoteskmimmackNo ratings yet
- AH2 Hesi ReviewDocument46 pagesAH2 Hesi ReviewJamie Antonini Grant100% (1)
- Musculoskeletal Note1Document34 pagesMusculoskeletal Note1FreeNursingNotes100% (4)
- Anemia: Ch. 31 Hematologic ProblemsDocument36 pagesAnemia: Ch. 31 Hematologic Problemshops23100% (3)
- This Study Resource Was: Hesi Pharmacology Test Bank 2018 RN V2 14 Total QuestionsDocument3 pagesThis Study Resource Was: Hesi Pharmacology Test Bank 2018 RN V2 14 Total QuestionsCrystal B Costa78No ratings yet
- Mnemonics PDFDocument15 pagesMnemonics PDFbeingfiredNo ratings yet
- Respiratory Drugs XL Chart 3Document2 pagesRespiratory Drugs XL Chart 3cdp1587100% (1)
- Care PlanDocument11 pagesCare PlanAlyssa CardinalNo ratings yet
- Medical Surgical NotesDocument18 pagesMedical Surgical NotesshalomNo ratings yet
- Blood Disorders AnemiaDocument6 pagesBlood Disorders AnemiaFreeNursingNotesNo ratings yet
- Clinical Medication WorksheetDocument1 pageClinical Medication WorksheetSrkocher100% (1)
- Top 400 Q & A Ms & FundaDocument9 pagesTop 400 Q & A Ms & FundaericNo ratings yet
- Cholinergics and Cholinergic BlockersDocument5 pagesCholinergics and Cholinergic Blockersapi-3739910100% (3)
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Oncology, HIV, DIC Study Guide.Document6 pagesOncology, HIV, DIC Study Guide.NursingSchoolNotes100% (1)
- Cancer Types, ChartDocument2 pagesCancer Types, ChartNursingSchoolNotesNo ratings yet
- Rogers GI Study GuideDocument2 pagesRogers GI Study GuideNursingSchoolNotesNo ratings yet
- Unit 5 Study Guide Part 2Document3 pagesUnit 5 Study Guide Part 2NursingSchoolNotesNo ratings yet
- UNIT 5 Study Guide Part 1Document5 pagesUNIT 5 Study Guide Part 1NursingSchoolNotesNo ratings yet
- Pulmonary Med Charts Part 1Document2 pagesPulmonary Med Charts Part 1NursingSchoolNotes100% (3)
- Unit 4 Study Guide Part 2Document7 pagesUnit 4 Study Guide Part 2NursingSchoolNotesNo ratings yet
- Hematologic System Drug ChartsDocument2 pagesHematologic System Drug ChartsNursingSchoolNotesNo ratings yet
- Unit 4 Study Guide Part 1Document6 pagesUnit 4 Study Guide Part 1NursingSchoolNotesNo ratings yet
- Unit 3 Study Guide Adult IIDocument7 pagesUnit 3 Study Guide Adult IINursingSchoolNotesNo ratings yet
- Lyte ChartDocument3 pagesLyte ChartNursingSchoolNotesNo ratings yet
- Sound It Out - ElectrolytesDocument2 pagesSound It Out - ElectrolytesNursingSchoolNotes0% (1)
- Unit 2 Part 1 Study GuideDocument6 pagesUnit 2 Part 1 Study GuideNursingSchoolNotes100% (1)
- Unit 2, Part 2 Study GuideDocument4 pagesUnit 2, Part 2 Study GuideNursingSchoolNotesNo ratings yet
- Unit 1, Part 2 Study GuideDocument4 pagesUnit 1, Part 2 Study GuideNursingSchoolNotes100% (1)
- Enteral Nutrition: Sana Inam Lecturer College of Pharmacy, GCUFDocument18 pagesEnteral Nutrition: Sana Inam Lecturer College of Pharmacy, GCUFAnum AzamNo ratings yet
- UntitledDocument301 pagesUntitledTuấn KiệnNo ratings yet
- Digestion ResonanceDocument52 pagesDigestion ResonanceEkta ManglaniNo ratings yet
- Abbey Secondary School Study Guides Final Biology PDFDocument42 pagesAbbey Secondary School Study Guides Final Biology PDFPeter Lwanda100% (1)
- Nutrition SIBO IMODocument5 pagesNutrition SIBO IMOBenNo ratings yet
- AbsorptionDocument84 pagesAbsorptionDr. Bharat JainNo ratings yet
- Intestinal Neoplasia in HorsesDocument8 pagesIntestinal Neoplasia in HorsesJoão Pedro PiccoloNo ratings yet
- Barium Procedure: Presented by Nur Faizah Wan Norainaa S YamimiDocument19 pagesBarium Procedure: Presented by Nur Faizah Wan Norainaa S YamimiNur faizah bt azmiNo ratings yet
- Gastrointestinal Hormones Regulating AppetiteDocument23 pagesGastrointestinal Hormones Regulating AppetiteHeba IyadNo ratings yet
- BCM Week 6 ModuleDocument22 pagesBCM Week 6 Moduleace danielNo ratings yet
- Physiology of DigestionDocument15 pagesPhysiology of Digestionreema amynNo ratings yet
- Lumen (Anatomy) - WikipediaDocument2 pagesLumen (Anatomy) - WikipediaKabir KhanNo ratings yet
- Original ArticleDocument18 pagesOriginal Articletuani barbosaNo ratings yet
- Robbins Pathology Chapter 17 Liver and Biliary TractDocument2 pagesRobbins Pathology Chapter 17 Liver and Biliary Tractscorpiosphinx79No ratings yet
- Agro-Industrial Wastes Into Animal Feed Through Microbial FermentationDocument14 pagesAgro-Industrial Wastes Into Animal Feed Through Microbial FermentationZahid MahmoodNo ratings yet
- Nutrition in MammalsDocument25 pagesNutrition in Mammalsmuhammad qureshiNo ratings yet
- Digestive System ScriptDocument7 pagesDigestive System ScriptGeraldine Co TolentinoNo ratings yet
- DIARE Pharmacotherapy Handbook 9th Edition 200 205 INGDocument6 pagesDIARE Pharmacotherapy Handbook 9th Edition 200 205 INGNyoman WiraNo ratings yet
- Sci6-Q2-Module-1 - Version 3Document47 pagesSci6-Q2-Module-1 - Version 3Dan RogayanNo ratings yet
- Human Digestive SystemDocument19 pagesHuman Digestive SystemsyagitaNo ratings yet
- База Тестів на ПМК2 з анатомії УКР і АНГDocument183 pagesБаза Тестів на ПМК2 з анатомії УКР і АНГAnzhelika BondarenkoNo ratings yet
- Nutrition Issues in GastroenterologyDocument10 pagesNutrition Issues in GastroenterologyjinniNo ratings yet
- DiverticulosisDocument49 pagesDiverticulosisJewelyn Alafriz AngelesNo ratings yet
- Organ Systems Power PointDocument14 pagesOrgan Systems Power PointJohn Harzel NagaNo ratings yet
- Demo Digestive DLPDocument8 pagesDemo Digestive DLPRimuru TempestNo ratings yet
- Diverticulum in Small Bowel With Foreign ObjectDocument7 pagesDiverticulum in Small Bowel With Foreign ObjectFerris BuhlerNo ratings yet