Professional Documents
Culture Documents
Plexus Cervicalis
Uploaded by
mcwnotes0 ratings0% found this document useful (0 votes)
281 views5 pagesSkull, scalp, superficial face and neck Bones, sutures, landmarks of the skull o skull / cranium, calvaria, neurocranium o cranial sutures: immovable, fibrous joints between two bones of the skull Coronal, sagittal, lambdoid, Metopic (inconstant) fracture is life threatening because middle meningeal artery can be ruptured leading to epidural hemorrhage Newborn fontan
Original Description:
Original Title
Plexus Cervicalis
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentSkull, scalp, superficial face and neck Bones, sutures, landmarks of the skull o skull / cranium, calvaria, neurocranium o cranial sutures: immovable, fibrous joints between two bones of the skull Coronal, sagittal, lambdoid, Metopic (inconstant) fracture is life threatening because middle meningeal artery can be ruptured leading to epidural hemorrhage Newborn fontan
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
281 views5 pagesPlexus Cervicalis
Uploaded by
mcwnotesSkull, scalp, superficial face and neck Bones, sutures, landmarks of the skull o skull / cranium, calvaria, neurocranium o cranial sutures: immovable, fibrous joints between two bones of the skull Coronal, sagittal, lambdoid, Metopic (inconstant) fracture is life threatening because middle meningeal artery can be ruptured leading to epidural hemorrhage Newborn fontan
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 5
Block 2: Head and Neck
Lecture 11: Skull, Scalp, Superficial Face and Neck
• Bones, sutures, landmarks of the skull
o Skull/cranium, calvaria, neurocranium, viscerocranium
o Cranial sutures: immovable, fibrous joints between two bones of the skull
Coronal, Sagittal, Lambdoid, Metopic (inconstant)
Pterion: fracture is life threatening because middle meningeal artery can be ruptured leading to
epidural hemorrhage
Newborn fontanelles
• Layers of the scalp
o Skin, connective tissue, aponeurosis (galea aponeurotica), loose connective tissue, pericranium
o Scalp lacerations profuse bleeding and gaping wounds if aponeurosis is cut
o Dangerous area: loose connective tissue facilitates transmission of infection (emissary veins to interior of
cranial cavity)
• Muscles of facial expression: motor innervated by Facial Nerve, sensory innervated by branches of Trigeminal Nerve
o Muscles of mastication (temporalis, masseter and medial/lateral pterygoids) motor innervated by CN V3
o Bell’s palsy (peripheral lesion of facial nerve): facial muscle paralysis, cannot close eyelids, angle of mouth
droops, forehead does NOT wrinkle
o Trigeminal neuralgia: intermittent excruciating pain in V2
o Thrombophlebitis of the facial vein (danger triangle): communication of facial vein with cavernous sinus
facilitates spread of infection from superficial face to inside of cranial cavity
• Structures of external, middle ear
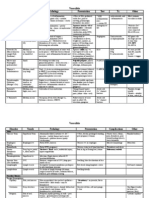
Lecture 12: Introduction to Cranial Nerves
Cranial Nerve Function Route thru skull Structures innervated Injury
I (olfactory) Smell Cribiform plate Anosmia, rhinorrhea
(ethmoid bond)
II (optic) Sight Optic canal Blindness
III (oculomotor) Move eyeball Superior orbital Eye muscles (except SO Eyeball is down and out,
fissure and LR) eyelid droop, dilated pupil
IV (trochlear) Move eyeball Superior orbital Superior oblique Inability to look down when
fissure eyeball in towards nose
V (trigeminal) Sensory: face V1: superior V1: scalp Loss of sensation, chewing
Move jaw orbital fissure V2: cheek, nose
V2: foramen V3: chin, muscles of
rotundum mastication
V3: foramen ovale
VI (abducent) Move eyeball Superior orbital Lateral rectus Medial strabismus (eye turns
fissure towards nose)
VII (facial) Move face, taste Internal acoustic Facial muscles, tongue Bell’s palsy, loss of taste
from front of meatus
tongue
VIII Hear, balance Internal acoustic Hearing, balance problems
(vestibulocochlear) meatus
IX Taste from back Jugular foramen Stylopharyngeus, tongue Problems swallowing, speech
(glossopharyngeal) of tongue, move difficulty
stylopharyngeus
X (vagus) Tons of stuff Jugular foramen Lots of muscles in Big problems…
throat/voicebox
XI (accessory) Move In thru foramen Sternocleidomastoid, Can’t raise shoulders, turn
sternocleidomast magnum, out thru trapezius head
oid and trapezius jugular foramen
XII (hypoglossal) Move tongue Hypoglossal canal Intrinsic tongue muscles, Tongue sticks out sideways
extrinsic tongue muscles
except palatoglossus
Autonomic function of Cranial Nerves
Oculomotor nerve:
Edinger-Westphal nucleus ciliary ganglion short ciliary nerves Sphincter pupillae: pupil constriction,
ciliary muscles: lens accommodation
Facial nerves:
Superior salivatory nucleus nervous intermedius to petrosal nerve pterygopalatine ganglion
zygomaticotemporal nerve to lacrimal nerve lacrimal gland: tearing
Superior salivatory nucleus nervous intermedius to chorda tympani submandibular ganglion
submandibular/sublingual salivary glands: salivation
Glossopharyngeal:
Inferior salivatory nucleus lesser petrosal nerve otic ganglion auriculotemporal nerve parotid gland:
salivation
Lecture 13: The Cranial Cavity
• Meninges
o Dura mater
Venous sinuses
o Arachnoid mater
o Pia mater
• Intracranial hemorrhages
o Epidural (arterial)
o Subdural (veinous)
o Subarachnoid (Circle of Willis)
o Cerebral (intracerebral)
• Cerebrospinal fluid = support for brain, blood vessels, nerves
o Site of secretion: choroids plexus
o Circulation
o Hydrocephalus: increased CSF volume leading to pressure on brain (communicating and non-communicating)
o Lumbar puncture
• Circle of Willis
• Anterior cranial fossa
o Frontal bone, ethmoid bone, sphenoid bone
o Foramen cecum, olfactory foramina, crista galli
• Middle cranial fossa
o Sphenoid bone, temporal bone, parietal bone
o Optic canal, superior orbital fissure, foramen rotundum, foramen ovale, foramen spinosum, foramen lacerum
• Posterior cranial fossa
o Sphenoid bone, temporal bone, occipital bone, parietal bone
o Internal acoustic meatus, jugular foramen, foramen magnum, hypoglossal canal
Lecture 14: The Orbit
Axes of orbits diverge at approximately 45 degrees but optical axes are parallel
• Eyelids
o Skin, muscle, tarsal plates/orbital septum, conjunctiva
o Conjunctivitis: common cause of painful red eye, mucopirulent discharge, itching and swelling
• Eyeball
o Lens
Cataract: cloudy lens, treated with surgical extraction
o Anterior cavity: contains aqueous humor
o Posterior cavity: contains vitreous humor
o Fibrous tunic
Sclera, cornea= major refractive structure (avascular)
o Vascular tunic
Choroid, ciliary body
Glaucoma: problem with resorption pressure blindness
Iris
• Lacrimal apparatus
• Blood vessels (arteries via the internal/external carotid artery)
• Autonomic innervation
• Clinical testing of extraocular muscles
• Injuries leading to disorders of eye movement
o Oculomotor nerve injury: ptosis, lateral strabismus, pupil dilation
o Trochlear nerve injury: inability to look down and nasally (leads to head tilt)
o Abducent nerve injury: medial strabismus
o Facial nerve injury: loss of lacrimation (dry cornea)
o Sympathetic fiber injury: Horner’s Syndrome, miosis, ptosis, anhydrosis, erythematosis
Lecture 15: Temporal, Infratemporal and Pterygopalatine Fossae
• Temporal fossa
o Contains temporalis muscle
• Infratemporal fossa
o Inferior to zygomatic arch, posterior to upper jaw
o Contains medial/lateral pterygoid muscles, temporalis muscle, maxillary artery, branches of V3 and VII, otic
ganglion
o Muscles of mastication: innervated by branches of mandibular nerve (V3), supplied by branches of maxillary
artery
Temporalis, masseter, lateral pterygoid, medial pterygoid
Gravity is the prime mover when opening the mouth
o Temporomandibular joint (TMJ) dislocated in ANTERIOR direction typically
o Branches of mandibular nerve: muscular branches, meningeal, buccal, auriculotemporal, inferior alveolar,
lingual
• Pterygopalatine fossa
o Openings
Pterygomaxillary fissure (lateral wall)
Inferior orbital fissure
Sphenopalatine foramen
Foramen rotundum
Pterygoid canal
Palatine foramina
o Contents
Pterygopalatine part of maxillary artery (branches!!)
Maxillary nerve
Lecture 16: Oral and Nasal Cavities
• Nasal cavity
o From external nares to the choanae
o Warm/humidify air (mouthbreathers do not have humidification of air!)
o Close proximity of brain and nasal cavity
o Blood supply from sphenopalatine artery (branch of maxillary artery)
o Paranasal sinuses
Designed to make head lighter
Middle meatus: ethmoid air cells, maxillary and nasal sinuses
Superior meatus: posterior ethoid air cells, sphenoid sinus
Inferior meatus: nasolacrimal duct
• Oral cavity
o Glands lubricate food (many redundancy)
• Pharynx
o Soft palate: sensory branches of V2 and glossopharyngeal nerves, soft palate muscles are innervated by the
vagus nerve EXCEPT tensor veli palatine (innervated by V3)
o Hard palate innervated by V2- greater and lesser palatine foramina
o Teeth
Upper teeth innervated by maxillary nerve
Lower teeth innervated by mandibular nerve
o Tongue
Anterior 2/3 Posterior 1/3
Taste VII-chorda tympani IX
Touch V3- lingual IX
Motor XII XII
• Extrinsic muscles of the tongue: genioglossus, hyoglossus, styloglossus (all innervated by
hypoglossal nerve) and palatoglossus (innervated by vagus nerve)
• Intrinsic muscles of the tongue: all innervated by hypoglossal nerve
• Larynx
Lecture 17: Cervical Region
• Strap muscles of the neck
o Omohyoid, sternohyoid, sternothyroid, thyrohyoid
o Innervated by ansa cervicalis which loops around internal jugular vein
o Stabilizes the hyoid and thyroid cartilages for swallowing, speech
• Cervical plexus: motor
o Ansa cervicalis, phrenic nerve (breathing), accessory nerve
• Triangles of the neck
o Posterior triangle
Borders: trapezius, clavicle, sternocleidomastoid
Contents: brachial plexus, vascular, CN XI
o Anterior triangle
Carotid
• Borders: omohyoid, digastric muscle, sternocleidomastoid
• Contents: LOTS of vasculature (Internal jugular vein, common carotid artery), vagus
nerve
Muscular
• Borders: midline, omohyoid, sternocleidomastoid
• Important structures: strap muscles
• Anterior scalene between subclavian vein and subclavian artery
• Blood supply
o Arterial: high pressure blood flow IN (not symmetric)
Common carotid, internal carotid, external carotid arteries
o Venous
Lecture 18: Visceral Structures of Neck
• Branchial arches
• Branchial cyst- 2nd arch grows over and attaches but does not disappear lump on lateral side of neck
• Branchial fistula- membrane between 2nd and 3rd arch breaks down leading to communication between pharynx and
skin
• Visceral sinus- 2nd arch grows over and does not attach
• Carotid sheath contents: vagus nerve, common carotid artery, internal jugular vein
• Deep cervical fascia: investing layer, pre-trachial layer, pre-vertebral layer
Lecture 19: Pharynx and Larynx
• Pharynx
o Nasopharynx
Auditory (Eustachian) tubes open into lateral wall
Pharyngeal isthmus closed off during swallowing
Adenoids (nasopharyngeal tonsils)= lymphatic tissue
o Oropharynx
Palatine tonsils between palatoglossal and palatopharyngeal arches
Tonsillitis: infectious disease affecting tonsils or adenoids
• Lymphatics drain into jugulodigastric lymph nodes
o Laryngopharynx
Piriform fossae (swallowed objects may lodge in this fossae… During extraction, be careful not
to damage internal branch of superior laryngeal nerve- branch of vagus nerve)
o Pharyngeal muscles (6 paired muscles)
Superior pharyngeal constrictor
Middle pharyngeal constrictor
Inferior pharyngeal constrictor
• Attaches to cridoid and thyroid cartilages
• Innervated by external pharyngeal nerve and recurrent laryngeal nerve
Stylopharyngeus (innervated by CN IX)
Salpingopharyngeus
Palatopharyngeus
o Innervation of the pharynx
o Pharyngitis: inflammation of pharynx, usually viral
o Swallowing (dysphagia= problem swallowing)
• Larynx (voice production)
o Skeleton
Thyroid cartilage
Cricoid cartilage (forms a complete ring)
Arytenoid (2)
Corniculate
Cuneiform
o Membranes/ligaments/folds
Rima glottides= space between the vocal folds
o Muscles (innervated by recurrent laryngeal nerve)
Cricothyroids: innervated by external laryngeal nerve
Transverse arytenoids
Oblique arytenoids
Posterior cricoarytenoids: OPEN THE RIMA GLOTTIDIS
Thyroarytenoids
Lateral Cricoarytenoids
Vocalis
o Innervation of the Larynx
Superior laryngeal nerve: Internal and external laryngeal nerves
Recurrent laryngeal nerve
o Epiglottitis/supraglottitis: inflammation of the soft tissues above the vocal folds (life-threatening because this
can obstruct airways)
o Laryngitis
o Croup: infection of upper respiratory tract
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Humerus Arm Anatomical Neck ArmDocument41 pagesHumerus Arm Anatomical Neck ArmmcwnotesNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesNo ratings yet
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesNo ratings yet
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNo ratings yet
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNo ratings yet
- Lab 2: Contractility of Visceral and Vascular (Aorta) SmoothDocument3 pagesLab 2: Contractility of Visceral and Vascular (Aorta) SmoothmcwnotesNo ratings yet
- Hypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesDocument1 pageHypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesmcwnotesNo ratings yet
- Surface Molecules: Molecule Location Ligand Action OtherDocument1 pageSurface Molecules: Molecule Location Ligand Action OthermcwnotesNo ratings yet
- Lab 10 Digestive System: Salivary Glands, Tongue, Esophagus, StomachDocument3 pagesLab 10 Digestive System: Salivary Glands, Tongue, Esophagus, StomachmcwnotesNo ratings yet
- Lab 1: Electrical and Mechanical Properties of Skeletal MuscleDocument3 pagesLab 1: Electrical and Mechanical Properties of Skeletal MusclemcwnotesNo ratings yet
- Lab 1: Electrical and Mechanical Properties of Skeletal MuscleDocument3 pagesLab 1: Electrical and Mechanical Properties of Skeletal MusclemcwnotesNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- ThyroidectomyDocument15 pagesThyroidectomyCalvin0% (1)
- External Carotid ArteryDocument80 pagesExternal Carotid Arterybaba bunnyNo ratings yet
- LarynxDocument21 pagesLarynxnano1987N100% (1)
- Anatomi MenelanDocument74 pagesAnatomi MenelanAnonymous KrEomRrNo ratings yet
- Complications of Thyroid SurgeryDocument26 pagesComplications of Thyroid SurgeryAhmed FriegNo ratings yet
- Larynx 18.07Document19 pagesLarynx 18.07Saneem AnwerNo ratings yet
- Clinical Manifestations: Psammoma BodiesDocument1 pageClinical Manifestations: Psammoma BodiesshinaNo ratings yet
- Anatomy of The Larynx: General DescriptionDocument38 pagesAnatomy of The Larynx: General DescriptionDr-Firas Nayf Al-ThawabiaNo ratings yet
- Functional Anatomy of Respiratory System and Mechanics of BreathingDocument98 pagesFunctional Anatomy of Respiratory System and Mechanics of BreathingdrusmanjamilhcmdNo ratings yet
- NEET PG 2013 Question Paper With SolutionsDocument2,164 pagesNEET PG 2013 Question Paper With SolutionsSK RaulNo ratings yet
- Larynx MCQSDocument114 pagesLarynx MCQSsidsudp100% (2)
- FCPS Surgery 25 Aug 2023 (M)Document20 pagesFCPS Surgery 25 Aug 2023 (M)Tauseef AfridiNo ratings yet
- PDFDocument156 pagesPDFvaishnavivivekNo ratings yet
- اسئلة تشريحDocument20 pagesاسئلة تشريحابراهيم فلاح حسنNo ratings yet
- Mcqs Head and NeckDocument11 pagesMcqs Head and NeckHazim Rhman Ali100% (2)
- Vocal Cord ParalysisDocument37 pagesVocal Cord ParalysisDr. T. Balasubramanian100% (3)
- Subtotal and Total Thyroidectomy: AuthorDocument10 pagesSubtotal and Total Thyroidectomy: AuthorAgustina TambingNo ratings yet
- Open Access Atlas of Otolaryngology, Head & Neck Operative SurgeryDocument20 pagesOpen Access Atlas of Otolaryngology, Head & Neck Operative SurgeryJamesNo ratings yet
- Superior Laryngeal Nerve InjuryDocument11 pagesSuperior Laryngeal Nerve InjuryBrilli Bagus DipoNo ratings yet
- Cranial NervesDocument44 pagesCranial NervesAlexandros LazarouNo ratings yet
- Kpbi 2010 Answer Respi SystemDocument38 pagesKpbi 2010 Answer Respi Systemwidyani rachimNo ratings yet
- Anatomy Head Neck EMRCS MCQDocument23 pagesAnatomy Head Neck EMRCS MCQTowhid HasanNo ratings yet
- Notes For USMLE Rx-01312019-Part IDocument410 pagesNotes For USMLE Rx-01312019-Part IjillNo ratings yet
- Unit 5: Anatomy and Physiology of LarynxDocument64 pagesUnit 5: Anatomy and Physiology of LarynxsachinlcNo ratings yet
- Awake Fiber-Optic BronchosDocument60 pagesAwake Fiber-Optic BronchosManisha SagarNo ratings yet
- Surface Anatomy and Other LandmarksDocument7 pagesSurface Anatomy and Other LandmarksoristoNo ratings yet
- Superior Laryngeal Neuralgia: Reported by O.R.GaneshamurthiDocument25 pagesSuperior Laryngeal Neuralgia: Reported by O.R.GaneshamurthiDr.O.R.GANESAMURTHINo ratings yet
- A Color Atlas of Orofacial Health and Disease in Children and Adolescents - ScullyDocument241 pagesA Color Atlas of Orofacial Health and Disease in Children and Adolescents - ScullyHameleo1000100% (3)
- Unit13 Anatomy MCQsDocument50 pagesUnit13 Anatomy MCQsAsadullah Yousafzai100% (2)
- ThyroidectomyDocument3 pagesThyroidectomyAnshuman Fotedar100% (1)