Professional Documents
Culture Documents
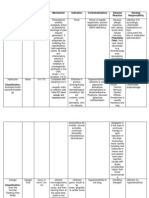
Disease Etiology Manifestation Medical Intervention Surgical Intervention Nursing Intervention
Uploaded by
Archie PunzalanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disease Etiology Manifestation Medical Intervention Surgical Intervention Nursing Intervention
Uploaded by
Archie PunzalanCopyright:
Available Formats
1 Punzalan
Disease Multiple Sclerosis is an immune-mediated progressive demyelinating disease of the CNS. It refers to the destruction of myelin, the fatty & protein material that surround certain nerve fibers in the brain & spinal cord resulting in impaired transmission of nerve impulses.
Etiology Cause is unknown, but most common theories point to a virus or genetic defect, or a combination of both. Geographic studies indicate there may be an environmental factor involved of which shows that Environmental exposure at a young age may play a role in the development of MS in later life.
Manifestation Fatigue Muscle spasms Depression Weakness Numbness Difficulty in coordination Loss of balance Pain Spasticity Visual disturbances such as: diplopia, patchy blindess, blurring of vision, & total blindess Incontinence Constipation Trouble in speech and swallowing
Medical Intervention No cure exists for MS. Medications are to treat symptoms and to delay progression of the disease. Medications used to slow the progression of multiple sclerosis are: Interferons (Avonex, Betaseron, or Rebif), glatiramer acetate (Copaxone), Mitoxantrone (Novantrone), and Natalizumab (Tysabri) Fingolimod (Gilenya ) Medicines to reduce muscle spasms: Lioresal (Baclofen), tizanidine (Zanaflex) Cholinergic medications to reduce urinary problems
Surgical Intervention
Nursing Intervention Provide emotional and psychological support for the patient and family. Assess patients neurologic status for deficits. 1. Monitor bowel and bladder function during hospitalization. 2. Keep bedpan or urinal readily accessible because the need to void is immediate. Promote and emphasize importance of physical mobility through exercises Prevent injury Minimize spasticity & contractures 3. Watch for adverse reactions to administered medications.
2 Punzalan
Antidepressants for mood or behavior symptoms Amantadine for fatigue
Help the patient establish a daily routine to maintain optimal functioning.
3 Punzalan
Myasthenia Gravis an autoimmune disorder affecting the myoneural junction, & is characterized by varying degrees of weakness of the voluntary muscles.
Diplopia Occurs when the immune system produces antibodies that Ptosis (dooping of eyelids) blocks or attacks acetylcholine receptors Fatigue which are components Generalized weakness of the neuromuscular junction.
Neostigmine Bromide (Prostigmin) or Pyridostigmine Bromide (Mestinon) to improve the communication between the nerves and the muscles. Corticosteroids: Prednisone to suppress immune response Plasmapheresis to treat exacerbations
1. 2. Establish accurate neurologic and can produce antigenrespiratory baseline. specific 3. immunosuppression and Stay alert for signs of result in clinical impending myesthenic improvement crisis. 4. 5. Administer medications on time. Thymectomy 6. When swallowing is difficult, give semi-solid foods instead of liquids to lessen the risk of choking. Minimize risk of aspiration. 7. 8. Plan exercise, meals, patient care, and activities to make the most of energy peaks. Help the patient plan daily activities to coincide with energy peaks. Stress the need for
The muscle weakness can lead to a variety of symptoms, including:
Breathing difficulty Chewing or swallo wing difficulty Difficulty talking Facial paralysis or weakness of the facial muscles Dysphonia
4 Punzalan
frequent rest periods. 9. Patient should be taught strategies to conserve energy. Patient should be reminded of important of maintaining health promotion practices.
5 Punzalan
Guillain-Barre Syndrome Cause is unknown. is a disorder in which the body's immune system attacks part of the peripheral nervous system. Muscle weakness Diminished reflexes of lower extremities that can lead to Quadriplegia Paresthesia Dyskinesia Hyporeflexia Dysphagia Paralysis of the ocular muscles Instability of Cardiovascular system Short-acting medications such as alpha-adrenergic blocking agents to treat tachycardia & hypertension Respiratory therapy or mechanical ventilation Use of anticoagulant agents to prevent thrombosis and pulmonary emboli. Plasmapheresis Continuous ECG monitoring. Enhance physical mobility by performing ROM exercises to patient. Provide adequate nutrition; if patient cannot swallow due to bulbar paralysis (immobility of muscles), a gastrostomy tube may be placed to administer nutrients. Improve communication by establishing or providing means to Maintain respiratory function. Monitor for change in vital capacity. Suctioning may be performed to maintain a clear airway.
6 Punzalan
communicate, collaboration with speech therapist can also be done. Decrease fear and anxiety to patient & family. Provide emotional support to the patient and his family.
7 Punzalan
Trigeminal Neuralgia is a neuropathic disorder characterized by episodes of intense pain in the face, originating from the trigeminal nerve. It is a condition of the 5th cranial nerve characterized by paroxysms of pain in the area innervated by any of the 3 branches, but it most commonly occurs in the 2nd and 3rd branches of the trigeminal nerve. The cause is not certain, but chronic compression or irritation of the trigeminal nerve or degenerative changes in the gasserian ganglion are the suggested causes.
Symptoms may include one or more of these patterns: Episodes of severe, shooting or jabbing pain that may feel like an electric shock Spontaneous attacks of pain or attacks triggered by things such as touching the face, chewing, speaking and brushing teeth Bouts of pain lasting from a few seconds to several seconds Episodes of several attacks lasting days, weeks, months or longer. Pain in areas supplied by the trigeminal nerve, including the cheek, jaw,
Anti-seizure agents such as Carbamazepine (Tegretol) to relieve pain by reducing transmission of impulses at certain nerve terminals. Gabapentin (Neurontin) & Baclofen ( Lioresal) are also used for pain control. Alcohol or phenol injection of the gasserian ganglion & peripheral branches of the trigeminal nerve could relieve pain for several months.
Microvascular Decompression of the Trigeminal Nerve
Instruct the client to avoid factors that can trigger the attack and result in exhaustion and fatigue. Percutaneous Assist the patient in Radiofrequency preventing and reducing Trigeminal Gangliolysis pain by providing choice of surgical preventive strategies. procedure Administer pain medications as needed. Use cotton pads gently, wash face and for oral hygiene. Avoid giving foods to client that are too cold or too hot. Explain to the client and his family the disease and its treatments.
8 Punzalan
teeth, gums, lips, or less often the eye and forehead
Pain affecting one side of your face at a time Attacks becoming more frequent and intense over time.
9 Punzalan
Bells Palsy Bells Palsy or facial paralysis is due to inflammation of the 7th cranial nerve, which results in weakness or paralysis of the facial muscles of the affected side. The cause is unknown, although possible causes may include vascular ischemia, viral disease, autoimmune disease, or a combination of all these factors. Distortion of the face Loss of wrinkling in the forehead Painful sensations in the face, behind the ear, & in the eye Facial spasms Increased lacrimation (tearing) Inability to close eyes Speech difficulty Occasional dysphagia Corticosteroid therapy (Prednisone) to reduce inflammation & edema; appears to diminish severity of disease, relieve the pain, & prevent or minimize denervation. Analgesic agents to control facial pain Electrical stimulation may be applied to the face to prevent muscle atrophy. Surgical decompression of the facial nerve Assess facial nerve function regularly. Maintain muscle tone of the face. Prevent or minimize denervation. Provide for pain relief with analgesics and local application of heat. Provide soft diet with supplementary feedings as indicated. Provide special eye care to protect the cornea. Provide support and reassurance. Administer medications as ordered.
10 Punzalan
Parkinsons Disease is a slowly progressing neurologic movement disorder that eventually leads to disability. The cause of most cases is unknown, but research suggests several causative factors, including genetics, atherosclerosis, excessive accumulation of oxygen free radicals, viral infections, head trauma, chronic antipsychotic medication use & some environmental exposures. Tremor Bradykinesia Rigid muscles Impaired posture and balance Loss of automatic movements Speech changes Dementia Antiviral therapy: Amantadine hydrochloride (Symmetrel_ used in early Parkinsons tx to reduce 3 cardinal signs of Parkinsons disease. Antidepressants: Tricyclic antidepressants to alleviate the depression. Antihistamines Dopamine Agonists Anticholinergic Agents such as Trihexyphenidyl, Cycrimine, Procyclidine, Biperiden, & Benztropine Mesylate) effective in controlling tremor & rigidity. Antiparkinsoninan Medications: Levodopa (Dopar, Larodopa) the most effective agent & the mainstay of tx. Thalamotomy and Pallidotomy are effective in relieving many symptoms of Parkinsons disease; the procedure interrupt nerve pathways, thereby alleviating tremor or rigidity Neural Transplantation Deep Brain Stimulation Improve mobility by encouraging the patient to participate in daily exercise, such as walking, riding stationary bike, swimming, or gardening. Advise the patient to perform stretching and postural exercises as outlined by a physical therapist. Teach the patient walking techniques to offset parkinsonian shuffling gait and tendency to lean forward. Monitor drug treatment to note adverse reactions. Monitor the patients nutritional intake and check weight regularly. Monitor the patients ability to perform activities of daily living.
11 Punzalan
Monoamine Oxidase Inhibitors (MAO INHIBITORS) Catechol-OMethyltransferase (COMT) Inhibitors
Encourage the patient to take warm baths and massage muscles to help relax muscles. Instruct the patient to rest often to avoid fatigue and frustration. Obtained a raised toilet seat to help the patient sit and stand. Teach the patient facial exercises and breathing methods to obtain appropriate pronunciation, volume, and intonation. Teach the patient about the medication regimen and adverse reaction.
You might also like
- A Simple Guide to Hand Tremors, Related Diseases and Use in Disease DiagnosisFrom EverandA Simple Guide to Hand Tremors, Related Diseases and Use in Disease DiagnosisRating: 3.5 out of 5 stars3.5/5 (3)
- Myasthenia Gravis, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMyasthenia Gravis, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Pathophysiology (Myasthenia Gravis) ..Document20 pagesPathophysiology (Myasthenia Gravis) ..Suku ydvNo ratings yet
- Neuro Continuation: Elenita H. Tinio, RN, MD, UsrnDocument52 pagesNeuro Continuation: Elenita H. Tinio, RN, MD, UsrnJessieRamosAnicetoNo ratings yet
- Neuromuscular Junction Diseases Presentation Dr. TarekDocument21 pagesNeuromuscular Junction Diseases Presentation Dr. TarekHero StoreNo ratings yet
- Sarah S. Taupan, RN, MN, DPADocument33 pagesSarah S. Taupan, RN, MN, DPAKatri ArasaNo ratings yet
- Multiple SclerosisDocument30 pagesMultiple Sclerosischikanyamichelle31No ratings yet
- Hes 005 Session 12 SasDocument12 pagesHes 005 Session 12 SasBread PartyNo ratings yet
- Hes 005 Session 12 SasDocument12 pagesHes 005 Session 12 SasJose Melmar Autida AutenticoNo ratings yet
- Epilepsy & Antiepileptic Drugs: Dr. Siva Priya Sonali Thanushanthan Tivashkar Srinaath SidhantasahooDocument40 pagesEpilepsy & Antiepileptic Drugs: Dr. Siva Priya Sonali Thanushanthan Tivashkar Srinaath Sidhantasahoothanush_15No ratings yet
- Neuropathies: Mrs. Keerthana.B Assistant Professor MSN, PSG ConDocument65 pagesNeuropathies: Mrs. Keerthana.B Assistant Professor MSN, PSG ConKeerthana BNo ratings yet
- Autoimmune Processes: Dr. Lubna DwerijDocument46 pagesAutoimmune Processes: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Trigeminal NeuralgiaDocument3 pagesTrigeminal NeuralgiaAira Alaro50% (2)
- NR 325 Neuro Worksheet 2Document6 pagesNR 325 Neuro Worksheet 2John Thomas100% (1)
- HeadacheDocument42 pagesHeadacheRaghoba GaonkarNo ratings yet
- Myasthenia Gravis: Dr. Ken Wirastuti, Mkes, SP.S Bagian Ilmu Penyakit Saraf Fk. UnissulaDocument30 pagesMyasthenia Gravis: Dr. Ken Wirastuti, Mkes, SP.S Bagian Ilmu Penyakit Saraf Fk. UnissulafemmytaniaNo ratings yet
- Multiple Sclerosis: Demyelination-Damages The Myelin Sheath and Neurons This Damage Slows Down orDocument6 pagesMultiple Sclerosis: Demyelination-Damages The Myelin Sheath and Neurons This Damage Slows Down orNorhana ManasNo ratings yet
- Disorder of Neuromuscular Junction: Myasthenia Gravis and Lambert-Eaton Myasthenic SyndromeDocument36 pagesDisorder of Neuromuscular Junction: Myasthenia Gravis and Lambert-Eaton Myasthenic SyndromePraneethaNo ratings yet
- Presented By: VIVEK DEVDocument38 pagesPresented By: VIVEK DEVFranchesca LugoNo ratings yet
- Myasthenia Gravis: Submitted To: Submitted byDocument10 pagesMyasthenia Gravis: Submitted To: Submitted bypandem soniyaNo ratings yet
- Movement Disorders: AtaxiaDocument7 pagesMovement Disorders: AtaxiaChakram SundarNo ratings yet
- CNS 2022Document8 pagesCNS 2022Kathleen Kate MonsalveNo ratings yet
- Multiple SclerosisDocument44 pagesMultiple SclerosisVijaya LakshmiNo ratings yet
- Degen Dses PDMSMGDocument28 pagesDegen Dses PDMSMGCrizale CorpuzNo ratings yet
- MGGBSDocument27 pagesMGGBSCyril_Cybernat_1553No ratings yet
- E-Therapeutics+ - Minor Ailments - Therapeutics - Central Nervous System Conditions - Vertigo and DizzinessDocument5 pagesE-Therapeutics+ - Minor Ailments - Therapeutics - Central Nervous System Conditions - Vertigo and DizzinessSamMansuriNo ratings yet
- Myasthenia GravisDocument45 pagesMyasthenia GravisVirgilio Reyes ManuelNo ratings yet
- Central Ner Vous System Disorders and Homotoxicology: Parkinson'S DiseaseDocument3 pagesCentral Ner Vous System Disorders and Homotoxicology: Parkinson'S DiseaseRui PiresNo ratings yet
- Adverse Effects of Antipsychotic DrugsDocument18 pagesAdverse Effects of Antipsychotic DrugsBhumika PatelNo ratings yet
- Chapter 21: Parkinson's Disease TreatmentDocument34 pagesChapter 21: Parkinson's Disease TreatmentrobinkirvenNo ratings yet
- Endocrine DisordersDocument54 pagesEndocrine Disorderspradeep pintoNo ratings yet
- FM-tute 4Document9 pagesFM-tute 4Sandarekha PereraNo ratings yet
- Neurological DisorderDocument10 pagesNeurological DisordersonyNo ratings yet
- Myasthenia GravisDocument32 pagesMyasthenia GravisSandhya HarbolaNo ratings yet
- Myathenis Gravis - 1St Draft: 3. Diagnosis and Symptomatology 3.1. SymptomatologyDocument4 pagesMyathenis Gravis - 1St Draft: 3. Diagnosis and Symptomatology 3.1. SymptomatologyAxl0No ratings yet
- Guillain-Barré Syndrome, Myasthenia Gravis,: Dr. Nermine ElcokanyDocument31 pagesGuillain-Barré Syndrome, Myasthenia Gravis,: Dr. Nermine ElcokanyTheresia Avila KurniaNo ratings yet
- Myasthenia Gravis: Moderator: DR Anitha PG: DR VijethaDocument45 pagesMyasthenia Gravis: Moderator: DR Anitha PG: DR VijethaJerusha VijethaNo ratings yet
- Extrapyramidal DisorderDocument35 pagesExtrapyramidal DisorderFerdy SetiawanNo ratings yet
- Hereditary Diseases of Nervous SystemDocument52 pagesHereditary Diseases of Nervous SystemAhmed Adel SaadNo ratings yet
- ATI Flash Cards 05, Medications Affecting The Nervous SystemDocument110 pagesATI Flash Cards 05, Medications Affecting The Nervous SystemGiovanni MictilNo ratings yet
- Headache 2Document21 pagesHeadache 2geeeelzy07No ratings yet
- Week 6 Discussion QuestionDocument8 pagesWeek 6 Discussion QuestionMayumi BalmesNo ratings yet
- Myasthenia Gravis: Prepared by Under Supervision of DRDocument13 pagesMyasthenia Gravis: Prepared by Under Supervision of DRAhoood ,No ratings yet
- 3 ConvulsionDocument22 pages3 ConvulsionMohamed Na3eemNo ratings yet
- Presentation On Myasthenia Gravis: Presented By: Sandhya Harbola M.Sc. Nursing 1 Year PcnmsDocument32 pagesPresentation On Myasthenia Gravis: Presented By: Sandhya Harbola M.Sc. Nursing 1 Year PcnmsShubham Singh Bisht100% (3)
- Bell's Palsy, MS, Epilepsy 2Document40 pagesBell's Palsy, MS, Epilepsy 2abdoNo ratings yet
- Myasthenia Gravis, Alzheimers Disease, Multiple Sclerosis, Guillain-Barre Syndrome and Bell PalsyDocument9 pagesMyasthenia Gravis, Alzheimers Disease, Multiple Sclerosis, Guillain-Barre Syndrome and Bell PalsyNielArmstrongNo ratings yet
- Chapter 21 - NeuromuscularDocument5 pagesChapter 21 - NeuromuscularJazlyn McClairenNo ratings yet
- Headache Syndromes Presentation Dr. TarekDocument50 pagesHeadache Syndromes Presentation Dr. TarekHero StoreNo ratings yet
- Anticonvulsants NotesDocument19 pagesAnticonvulsants NotesPIRENANo ratings yet
- Extrapyramidal Symptoms - StatPearls - NCBI BookshelfDocument6 pagesExtrapyramidal Symptoms - StatPearls - NCBI BookshelfFitrah RahmadhaniNo ratings yet
- PharmTest3 StudyGuideDocument9 pagesPharmTest3 StudyGuideTara Bickford ManisNo ratings yet
- Ankylosing Spondylitis: - Arun - RDocument28 pagesAnkylosing Spondylitis: - Arun - RArun KumarNo ratings yet
- Multiple SclerosisDocument35 pagesMultiple SclerosisJc SeguiNo ratings yet
- Headache: by Yahya Ibrahim MBCHB 3. Dr. BacwaDocument54 pagesHeadache: by Yahya Ibrahim MBCHB 3. Dr. BacwaHarun MohamedNo ratings yet
- Tension Type HeadacheDocument30 pagesTension Type HeadacheIndraYudhi100% (2)
- 2 - MultipleSclerosisDocument32 pages2 - MultipleSclerosisHADI BADWANNo ratings yet
- Park in SonDocument2 pagesPark in SonrajeevkeyarNo ratings yet
- Myasthenia GravisDocument15 pagesMyasthenia GravisHibba NasserNo ratings yet
- Case 1Document12 pagesCase 1Denisa-Alexandra MănăstireanuNo ratings yet
- Para Iterax XylogelDocument2 pagesPara Iterax XylogelArchie PunzalanNo ratings yet
- Sample RN Staff School Nurse Evaluation Form Final 10 6 2011Document4 pagesSample RN Staff School Nurse Evaluation Form Final 10 6 2011Archie PunzalanNo ratings yet
- Para Iterax XylogelDocument2 pagesPara Iterax XylogelArchie PunzalanNo ratings yet
- Pneumonia Case Pres Level 2 Group 4Document43 pagesPneumonia Case Pres Level 2 Group 4Archie Punzalan67% (3)
- Lesson Plan On Spina BifidaDocument24 pagesLesson Plan On Spina BifidaPriyaNo ratings yet
- Family Laboratory For Medical Analysis: Test & SpecimenDocument1 pageFamily Laboratory For Medical Analysis: Test & SpecimenMohamad BadranNo ratings yet
- Foundations of Operative Surgery An Introduction To Surgical TechniquesDocument165 pagesFoundations of Operative Surgery An Introduction To Surgical TechniquesTeodora-Valeria TolanNo ratings yet
- Full Body To Body Massage Centre in MG Road Gurgaon - Spa in Gurgaon MG RoadDocument11 pagesFull Body To Body Massage Centre in MG Road Gurgaon - Spa in Gurgaon MG RoadFlip Body SpaNo ratings yet
- Pukpuklo A Wealth in The SeaDocument2 pagesPukpuklo A Wealth in The SeaKrizha Angela NicolasNo ratings yet
- HIV Drug Chart (2021)Document1 pageHIV Drug Chart (2021)savNo ratings yet
- Insights and Images: Vascular Channel Mimicking A Skull FractureDocument2 pagesInsights and Images: Vascular Channel Mimicking A Skull Fracturethariq mubarakNo ratings yet
- Editorial: Dental Caries and OsteoporosisDocument2 pagesEditorial: Dental Caries and OsteoporosisBagis Emre GulNo ratings yet
- PhobiaDocument4 pagesPhobiaZeba QuadiriNo ratings yet
- AMARACHI WORK FinalizedDocument67 pagesAMARACHI WORK FinalizedocNo ratings yet
- Anatomy and Physiology - Dengue FeverDocument3 pagesAnatomy and Physiology - Dengue Feverhael yam62% (13)
- Acute Gastritis CiciDocument43 pagesAcute Gastritis CiciDwi Rezky AmaliaNo ratings yet
- Wound CareDocument77 pagesWound CareNestor Balboa100% (1)
- Meningococcal Infection in ChildrenDocument6 pagesMeningococcal Infection in ChildrenAdrian KhomanNo ratings yet
- Total Hip and Total Knee Replacement Post Operatif Nursing ManagementDocument5 pagesTotal Hip and Total Knee Replacement Post Operatif Nursing ManagementAnas KhafidNo ratings yet
- Behavioral Health Care Plan: Assessment DataDocument9 pagesBehavioral Health Care Plan: Assessment Dataapi-521018364No ratings yet
- CortisolDocument27 pagesCortisolCao YunNo ratings yet
- Siobhan (2017) - Smudging of The Motor Cortex Is Related To The Severity of Low Back PainDocument7 pagesSiobhan (2017) - Smudging of The Motor Cortex Is Related To The Severity of Low Back PainLuciana AraújoNo ratings yet
- Curriculum Vitae: School of Regeneration and Encouragement KEMA FK UNPADDocument7 pagesCurriculum Vitae: School of Regeneration and Encouragement KEMA FK UNPADReki PebiNo ratings yet
- ShockDocument53 pagesShockHassan Ahmed100% (3)
- Beth PRC FormDocument11 pagesBeth PRC FormNev Bryan DapitanNo ratings yet
- Che 225 Control of Communicable DiseasesDocument19 pagesChe 225 Control of Communicable DiseasesAbdullahi Bashir SalisuNo ratings yet
- Comparative Efficacy and Acceptability META-ANALYSIS 2015Document11 pagesComparative Efficacy and Acceptability META-ANALYSIS 2015Alexandra CastellanosNo ratings yet
- Bilateral OsteoarthritisDocument58 pagesBilateral OsteoarthritisMaya VilNo ratings yet
- Ncma215 - Nutrition and Diet Therapy: Week - 9Document4 pagesNcma215 - Nutrition and Diet Therapy: Week - 9ABEGAIL BALLORANNo ratings yet
- D An Introduction: Physical Medicine and RehabilitationDocument33 pagesD An Introduction: Physical Medicine and RehabilitationChadNo ratings yet
- Urtricaria SDocument8 pagesUrtricaria SpalNo ratings yet
- 2020 Anaphylaxis JACI 2020Document42 pages2020 Anaphylaxis JACI 2020Peter Albeiro Falla CortesNo ratings yet
- Eye Lids and Lacrimal System: Dr. Binto Akturusiano, SPMDocument59 pagesEye Lids and Lacrimal System: Dr. Binto Akturusiano, SPMranz ibonkNo ratings yet
- TramadolDocument2 pagesTramadolJordanne EtisNo ratings yet