Professional Documents
Culture Documents
Downey L, Lloyd H - Bed Bathing Patients in Hospital - Article
Uploaded by
mamatnamakuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Downey L, Lloyd H - Bed Bathing Patients in Hospital - Article
Uploaded by
mamatnamakuCopyright:
Available Formats
If you would like to contribute to the art and science section contact: Gwen Clarke, art and science
editor, Nursing Standard, The Heights, 59-65 Lowlands Road, Harrow-on-the-Hill, Middlesex HA1 3AW. email: gwen.clarke@rcnpublishing.co.uk
Bed bathing patients in hospital
Downey L, Lloyd H (2008) Bed bathing patients in hospital. Nursing Standard. 22, 34, 35-40. Date of acceptance: January 31 2008.
Summary
There are a number of circumstances that may affect an individuals ability to maintain personal hygiene. Hospitalised patients, and in particular those who are bedridden, may become dependent on nursing staff to carry out their hygiene needs. Assisting patients to maintain personal hygiene is a fundamental aspect of nursing care. However, it is a task often delegated to junior or newly qualified staff. This article focuses on the principles of bed bathing patients in hospital, correct procedure and the importance of maintaining patient dignity and respect in clinical practice.
Authors
Lindsey Downey is practice development nurse and Hilary Lloyd is principal lecturer in nursing practice development and research, Sunderland Royal Hospital. Email: lindsey.downey@chs.northy.nhs.uk
Keywords
Cross-contamination; Dignity and respect; Hygiene care These keywords are based on the subject headings from the British Nursing Index. This article has been subject to double-blind review. For author and research article guidelines visit the Nursing Standard home page at www.nursing-standard.co.uk. For related articles visit our online archive and search using the keywords.
It is important to ensure that essential hygiene needs are met, such as bed bathing, and that nursing procedures are correct and in line with local policies and guidelines to prevent the spread of infection and promote dignity and respect for all patients. Young (1991) described cleanliness as a basic human right, not a luxury. Personal hygiene is the physical act of cleansing the body to ensure that the skin, hair and nails are maintained in an optimum condition (Department of Health (DH) 2003). Assisting a patient to maintain his or her personal hygiene needs contributes to the comfort, safety, wellbeing and dignity of the individual and helps to prevent the spread of infection. Patients should receive the level of assistance that they require to meet their individual personal hygiene needs (DH 2001a), which will vary between individuals and cultures. The nurse should demonstrate sensitivity and competency to be able to deal with the bodies and bodily functions of individual patients and differences in cultural practices to ensure that hygiene needs are met (Castledine 2005).
Bed bathing
THE HEALTHCARE Commission (2007) reported that up to 30% of complaints about care in NHS hospital trusts related to dignity and respect, as well as other aspects of essential personal care. Examples included: Patients left in soiled bedding and clothing. Personal hygiene needs not being met, for example, no regular baths or showers. Hair and nail care not always being provided. Bedside curtains and room doors not being closed properly. Staff entering rooms without knocking or waiting for permission to enter. NURSING STANDARD Bed bathing can help to maintain the hygiene needs of patients who are bedridden as a result of acute illness or chronic debilitation. Although a bed bath is not the most effective way of washing patients, and wherever possible patients should be encouraged and supported to shower or bathe to promote independence (Baker et al 1999), it may be the only way to meet the hygiene needs of, for example, the unconscious patient (Waugh 2007). Cultural awareness and personal preferences Before undertaking a bed bath, or any aspect of hygiene care, the nurse should acknowledge the patients preferences. The nurse should not impose his or her own standards of cleanliness on the patient or even assume that these will be the same as the patients. Personal preferences might april 30 :: vol 22 no 34 :: 2008 35
art & science clinical skills: 47
include what toiletries the patient uses, for example, or whether the patient would normally use soap on his or her face. Other preferences for care may relate to the patients cultural or religious beliefs. Keesing (1981) referred to culture as shared ideas, rules and meanings. Culture underpins the way that human beings live and the way that they express themselves. Nurses should ensure that they have an understanding of patients various religious and cultural needs. Cultural understanding is particularly important in the sensitive and highly personal area of bed bathing and, if requested, all attempts should be made for the bed bath to be performed by someone of the same gender. For example, Muslims and Hindus generally prefer to wash in running water, therefore patients should be given the option of showering where possible (Holland and Hogg 2001). When nursing a Muslim patient, especially of the opposite gender, direct skin-to-skin contact should be avoided, as this may distress the individual (Ethnicity Online 2003). It is important that the nurse views the patient as an individual with different health needs, beliefs and behaviours, while acknowledging religious and cultural practices to maintain patient dignity and wellbeing. Privacy and dignity Privacy and dignity are paramount when assisting a patient with his or her hygiene needs. Bed bathing is a personal and intrusive procedure, and the patient may feel embarrassed or even frustrated relying on someone else to meet his or her intimate needs. Basic methods of maintaining privacy and dignity include: Covering patients with a sheet or towel while they are being washed so that no part of the body is left exposed. Taking care to ensure that any curtains around bed areas are closed properly and that there are no gaps through which other people can see. Trying to prevent other people, staff or visitors from entering the room during bed bathing. It is important that all members of staff respect patient privacy and dignity. If the curtains surrounding a bed are closed or the door to the patients room is closed, staff should ask if they can enter before doing so, either by knocking on the door or asking the person behind the curtain. Assessment Bed bathing provides the nurse with an opportunity to assess the patients activities of living. Valuable insight can be gained regarding the independence or dependence of the patient, 36 april 30 :: vol 22 no 34 :: 2008
&
including mobility, hygiene, dressing and continence needs. The nurse can use this contact with the patient to find out about his or her nutritional status, sleeping patterns and pain experiences. Communication will enable the patient to discuss any issues or concerns regarding the care plan or treatment regimen. The nurse is also ideally placed to assess the patients skin and pressure areas as well as the risk of pressure ulcer development. During bed bathing the nurse can also observe for any non-verbal cues, such as grimacing or frowning, which may suggest that the patient is experiencing pain or discomfort. Communication The provision of hygiene care offers an opportunity for the nurse to communicate with the patient and assess the individuals physical and psychological state, detecting potential anxieties and fears (Wilson 1986). Meaningful conversation enables the nurse to provide a supportive dialogue and discuss any sensitive and difficult issues that may arise. Discussion, observation, explanation and evaluation during this time can inform realistic care planning, with individualised, achievable goals (Baker et al 1999). It is important that the nurse engages in appropriate conversation with the patient. If two nurses are present during bed bathing the patient should not be excluded. The discussion of personal issues between nurses and talking over the patient should be avoided. Many patients appreciate the opportunity to participate in small talk with the nurse to reduce embarrassment. Language used when conversing with the patient or describing nursing terms and anatomy should be kept simple. For example, a patient might not understand what the nurse means when asking: Can I wash your sacral area? Complex language and terminology should be adapted to meet the needs of the patient and ensure that he or she understands the procedure. If a patient requires language or signing support, he or she should be offered the services of an interpreter, communication aids or identified support systems to ensure effective communication takes place. Consent The registered nurse must obtain consent from the patient before providing treatment or care (Nursing and Midwifery Council (NMC) 2004). All professionals should understand the laws and local policy pertaining to consent. The NMC Code of Professional Conduct (NMC 2004) and the Good Practice in Consent Implementation Guide (DH 2001b) provide guidance for nurses on gaining consent. To ensure consent, the nurse explains all aspects of care to the patient before any procedure is performed. It is important to remember that even if the patient gives his or her verbal consent to a NURSING STANDARD
bed bath before it is carried out, the patient can withdraw this consent at any time or may choose not to consent to a particular part of his or her body being washed by the nurse. Delegating Bed bathing is often seen as a mundane nursing task. Castledine (2005) suggested that some aspects of nursing care were viewed as unattractive because they involved unpleasant, repetitive and harder physical work. Delegating the task of bed bathing to a junior member of the team or a healthcare assistant may result in the nurse in charge of the patients care missing vital information and the opportunity to enhance the nurse-patient relationship. It is important that the nurse recognises his or her personal accountability for the care that is provided, but also for delegating that care to an appropriate person (NMC 2004). The nurse should ensure that details of care delivered are documented in an accurate and timely fashion. This includes documenting any occasions when a patient may have refused care or treatment. Risk assessment It is essential to ensure that any relevant risk assessments have been carried out before performing a bed bath. The nurse accountable for delegating a bed bath must also ensure that any risks have been communicated to colleagues to maintain their health and safety as well as that of the patient. Risk assessments might include moving and handling, pressure area, falls and infection control. The nurse should always follow local policies and procedures in the reduction of risk.
Flannel or wash cloth, preferably disposable, or wipes. Clean linen and laundry skip. At least two sets of washbowls and towels. Toiletries such as soap, shampoo, conditioner and deodorant. Toothbrush and toothpaste or mouth care pack. Brush or comb. Shaving equipment. Cleanser or moisturiser. Incontinence pad, if needed. Clean nightclothes. Table 1 provides an example of a procedure that could be used when carrying out a bed bath. Special considerations There are a number of areas that require special attention during bed bathing to maintain the patients health and comfort. If the patient has frail or dehydrated skin, wounds or pressure ulcers, or any areas which are reddened, the nurse should take extra care while washing these areas, to ensure that further damage to the skin does not occur. Patients may have intravenous (IV) or arterial devices in situ, a wound or chest drain or a wound dressing. The nurse should take care when washing around these devices to reduce the risk of infection and prevent any drains or IV catheters from being dislodged. Consideration should also be given to patients who may experience pain or discomfort on movement, for example, following surgery. The nurse should ensure that any unnecessary movement is minimised and consider the use of analgesics before carrying out a bed bath. Extra care must be taken with patients who are haemodynamically unstable, for example, have abnormal cardiac function. The use of disposable flannels or wash cloths is recommended. This reduces the risk of fabric wash cloths becoming colonised with micro-organisms from warm and moist body areas, such as the axillae, genitals, groin, buttocks and anal area, when they are left to dry and are later reused to wash another part of the body. Soiled and infected linen must be disposed of as per local trust policy. Disposable gloves and aprons should be used as specified in the trusts policies and procedures, for example, to prevent cross-contamination of patients with Clostridium difficile. The nurse should ensure that universal precautions are maintained when carrying out a bed bath, particularly when washing a patients genitals. It is not necessary, however, to wear gloves for april 30 :: vol 22 no 34 :: 2008 37
Bed bathing procedure
NHS trusts may choose to develop guidelines for undertaking a bed bath or they may adopt one of the guidelines or procedures published in the nursing literature. Some organisations advocate following the procedure outlined in The Royal Marsden Hospital Manual of Clinical Nursing Procedures (Allen et al 2004). Other comprehensive procedures have been illustrated by Baker et al (1999) and Pegram et al (2007). There is generally a lack of research on the topic of bed bathing and further evidence is required to identify best clinical practice and improve patient care. Equipment Before carrying out a bed bath the nurse should ensure that he or she has all of the necessary equipment to hand. The nurse should never leave the patient exposed or at risk during the procedure to obtain missing equipment. Equipment required for a bed bath should include: Disposable apron, gloves and yellow clinical waste bag. Sliding sheet or hoist, if required. NURSING STANDARD
art & science clinical skills: 47
the whole procedure and the nurse should use his or her clinical judgement when deciding to do so, and an explanation should be offered to the patient. The wash water should be changed whenever it becomes dirty, cold or too soapy, and should always be changed after washing the genitals, buttocks and anal area. The temperature of the water must be checked by the nurse before washing the patient to ensure that it is not too hot or too cold; this should be in accordance TABLE 1 Procedure guidelines for bed bathing a patient
Action The patients plan of care should be consulted before carrying out a bed bath. This should include an assessment of the patients needs and preferences and should address religious and cultural beliefs. Before each step of the bed bath the patients independence and level of participation should be assessed. Where possible, the patient should be encouraged and enabled to carry out his or her own personal hygiene needs with the nurse assisting as required. During each step of the procedure the nurse should ensure that correct manual handling techniques and/or equipment are used. Hearing aids or spectacles should be cleaned. The procedure should be explained to the patient. The patient should be given the option of using the urinal, bedpan or commode. All equipment required should be collected before the procedure. The environment should be prepared. The area around the bed should be kept private and draught free. Curtains and/or doors should be closed. A washbowl should be filled with warm water. The patient should be asked to confirm the temperature of the water (if able). Hands should be washed. Disposable gloves and aprons should be worn according to local guidelines. The patient should be assisted with the removal of clothing. The patient should be covered with a bath towel or sheet before folding back the bedclothes. The patient should be asked whether he or she uses soap on the face. The face, neck and ears should be washed, rinsed and dried. The top half of the body, including the hands, arms, axillae and torso, should be washed and rinsed. It is important to ensure that the area under the breasts is washed and dried thoroughly. Areas of the body that are not being washed should remain covered. Care should be taken not to wet drains, dressings and/or intravenous devices. Toiletries should be applied as required. The water should be changed and disposable gloves should be worn. The patient should be informed that the area around the genitalia is going to be washed. Verbal consent from the patient should be obtained or the patient should be asked to wash the area, if possible.
&
with the patients preference and local or national guidance relating to health and safety. Within the Essence of Care hygiene benchmark patients are expected to supply their own toiletries and single-use toiletries should be provided until patients can supply their own (DH 2003). It may be necessary for the nurse to ask the patients family or friends to bring the patients toiletries into hospital. Communal toiletries should not be used or shared between patients, as this increases the risk of cross-contamination. Special consideration should be given to the eyes and mouth. They have been mentioned in brief as these are standalone procedures. It is recommended that the nurse reads additional
Rationale To plan care and ensure patient comfort and safety during the procedure. To promote the patients dignity and uphold his or her human rights. To negotiate involvement by the patient and so promote independence.
To reduce the risk of the patient or nurse sustaining a manual handling injury. To ensure the prosthesis is in good working order and free from debris and contaminants. To ensure that the patient understands the procedure and gives his or her consent. To reduce any disruption to the procedure and prevent any discomfort. To minimise time spent away from the patient during the procedure. To maintain a safe environment and promote privacy and dignity. To maintain the safety and comfort of the patient. To minimise the risk of cross-contamination in the clinical environment. To maintain the patients modesty and sustain body temperature. To promote cleanliness and ensure that patient preferences are acknowledged. To promote patient wellbeing and cleanliness and reduce the risk of cross-contamination.
To reduce the risk of cross-contamination and to maintain patient comfort and dignity.
38 april 30 :: vol 22 no 34 :: 2008
NURSING STANDARD
TABLE 1 Procedure guidelines for bed bathing a patient (continued)
A separate flannel or wipe should be used to wash around the genitalia. To promote good meatal hygiene and reduce the risk The area should be dried. Gloves should be removed and disposed of in line of cross-contamination. with hospital policy. Hands should be decontaminated. When washing this area, it is important to remember that female patients must be washed from the front to the back. Male patients should draw back the foreskin, if uncircumcised, when washing the penis. If the patient has a urinary catheter appropriate catheter hygiene should be carried out. Change the water and towel. The legs and feet should be washed and dried. All areas that are not being washed should remain covered. The need for possible podiatry referral should be assessed. The patient should be assisted to roll onto his or her side. The patients back should be washed, rinsed and dried. Disposable gloves should be worn and a disposable flannel or wipe should be used to wash and dry the sacral area, observing pressure areas. Gloves should be removed and disposed of in line with hospital policy. Hands should be decontaminated. Clothes should be replaced. If the patient is to remain in bed, the bottom sheet should be changed while the patient is being turned. A minimum of two nurses should be present during the procedure. The top bedclothes should be remade. Dispose of soiled bedclothes in line with hospital policy. The patient should be assisted with facial shaving or application of make up, if required. The patients teeth and mouth should be cleaned using a toothbrush and toothpaste or sponge sticks. Dentures should be removed, cleaned and replaced. The patients hair should be brushed or combed as desired. The patient should be assisted to sit or lie in the desired position. To reduce the risk of cross-contamination. To promote cleanliness and ensure that privacy is maintained. To maintain the safety of the patient and ensure safe manual handling, and to reduce the risk of cross-contamination.
To promote patient comfort and modesty. To maintain the safety of the patient and ensure safe manual handling. To reduce the risk of cross-contamination. To promote a positive body image. To promote good oral hygiene.
To promote a positive body image and enhance patient comfort. To reduce the risk of pressure ulcer development and enhance patient comfort.
Equipment should be removed from the bedside. The patients possessions To maintain a safe environment and promote patient should be put back in their appropriate place. The locker, bedside table and call safety. bell should be placed within reach. Hands should be washed and any clinical waste should be disposed of in line with hospital policy. Care provided should be documented. To reduce the risk of cross-contamination. To provide recorded documentation of care to aid communication with other members of the multiprofessional team.
(Adapted from Baker et al 1999, Allen et al 2004, Pegram et al 2007)
information on the appropriate procedures available for eye and mouth care.
Benchmarking care
The NHS Plan (DH 2000) reinforced the importance of getting the basics of nursing care right, while improving the patient experience. Essence of Care provided a clinical benchmarking tool to enable practitioners to adopt a patient-focused and structured approach to establish and share best practice (DH 2001a). Benchmarks relating to hygiene, self-care and NURSING STANDARD
privacy and dignity are particularly important when meeting the needs of patients during the task of bed bathing. However, communication, continence, bladder and bowel care, nutrition, pressure ulcer care, record keeping, safety, promoting health and the environment are also important considerations when reviewing and identifying best practice and developing action plans to improve patient care relating to hygiene. Nurses should familiarise themselves with the Essence of Care benchmarks (DH 2003) to ensure that care is patient focused and based on best practice (Table 2). april 30 :: vol 22 no 34 :: 2008 39
art & science clinical skills: 47
Conclusion
Personal cleanliness is important to promote wellbeing. Hospitalised patients should be assisted TABLE 2 Benchmarks for personal and oral hygiene
Factor Individual assessment of personal and oral hygiene needs. Care for personal and oral hygiene negotiated and planned based on assessment. Environment within which oral and personal hygiene needs are met. Provision of toiletries for own personal use.
&
to maintain personal hygiene to promote comfort, dignity and prevent the spread of infection. Bed bathing should be carried out with competency and sensitivity to the patients individual preferences and cultural and religious needs. The procedure for bed bathing should follow local guidelines and policies to ensure that care is safe, patient focused and based on best practice NS
Benchmark for best practice All patients are assessed to identify the advice and/or care required to maintain and promote individualised personal and oral hygiene. Planned care is negotiated with patients and/or carers and is based on assessment of individual needs. Patients have access to an environment that is safe and acceptable to the individual. Patients are expected to supply their own toiletries but single-use toiletries are provided until they can do so. Patients have access to the level of assistance that they require to meet individual personal and oral hygiene needs. Patients and/or carers are provided with information and education to meet the patients individual personal and oral hygiene needs. Care is continually evaluated, reassessed and the care plan renegotiated with the patient.
Providing assistance with personal and oral hygiene when required.
Information and education to support patients in meeting personal and oral hygiene needs, particularly if these are changing or are having to be met in unfamiliar surroundings. Evaluation and reassessment of personal and oral hygiene needs and how effectively these are being met.
(Department of Health 2003)
References
Allen K, Duncan A, Maguire J (2004) Personal hygiene: skin care. In Dougherty L, Lister S (Eds) The Royal Marsden Hospital Manual of Clinical Nursing Procedures. Sixth edition. Blackwell Publishing, Oxford, 580-586. Baker F, Smith L, Stead L (1999) Giving a blanket bath: 1. Nursing Times. 95, 3, Suppl 1-2. Castledine G (2005) The been there, done that attitude. British Journal of Nursing. 14, 20, 1103. Department of Health (2000) The NHS Plan: A Plan for Investment, A Plan for Reform. The Stationery Office, London. Department of Health (2001a) Essence of Care: Patient-focused Benchmarking for Health Care Practitioners. The Stationery Office, London. Department of Health (2001b) Good Practice in Consent Implementation Guide: Consent to Examination or Treatment. The Stationery Office, London. Department of Health (2003) Essence of Care: Patient-Focused Benchmarks for Clinical Governance. The Stationery Office, London. Ethnicity Online (2003) Muslims: Inpatient Care. www.ethnicityonline.net/ islam_inpatient_care.htm (Last accessed: April 4 2008.) Healthcare Commission (2007) State of Healthcare 2007: Improvements and Challenges in Services in England and Wales. Commission for Healthcare Audit and Inspection, London. Holland K, Hogg C (2001) Cultural Awareness in Nursing and Health Care: An Introductory Text. Hodder Arnold, London. Keesing RM (1981) Cultural Anthropology: A Contemporary Perspective. Holt, Rinehart and Winston, Austin TX. Nursing and Midwifery Council (2004) The NMC Code of Professional Conduct: Standards for Conduct, Performance and Ethics. NMC, London. Pegram A, Bloomfield J, Jones A (2007) Clinical skills: bed bathing and personal hygiene needs of patients. British Journal of Nursing. 16, 6, 356-358. Waugh A (2007) Caring for the person with physical needs, sensory impairment and unconsciousness. In Brooker C, Waugh A (Eds) Foundations of Nursing Practice: Fundamentals of Holistic Care. Mosby, London, 16, 425-462. Wilson M (1986) Personal cleanliness. Nursing. 3, 2, 80-82. Young L (1991) The clean fight. Nursing Standard. 5, 35, 54-55.
40 april 30 :: vol 22 no 34 :: 2008
NURSING STANDARD
You might also like
- Article The Nurse S Role in Helping Older People To Use The ToiletDocument5 pagesArticle The Nurse S Role in Helping Older People To Use The ToiletAnonymous hnk5L17No ratings yet
- Lec NCM 100Document27 pagesLec NCM 100Jay DavidNo ratings yet
- Lydia HallDocument2 pagesLydia HallHazel ZullaNo ratings yet
- The Complete Guide to Nursing and Interview Questions and AnswersFrom EverandThe Complete Guide to Nursing and Interview Questions and AnswersNo ratings yet
- Fundamentals of Nursing Week12 2Document49 pagesFundamentals of Nursing Week12 2alyssatorillo22No ratings yet
- Humanism, Nursing, Communication and Holistic Care: a Position Paper: Position PaperFrom EverandHumanism, Nursing, Communication and Holistic Care: a Position Paper: Position PaperNo ratings yet
- Personal Hygiene: Mary Grace L. Araullo RN MSCPDDocument23 pagesPersonal Hygiene: Mary Grace L. Araullo RN MSCPDgraceNo ratings yet
- Nurs04 WK4Document10 pagesNurs04 WK4MARY ROSE FAJUTINANo ratings yet
- Incontinence CareDocument7 pagesIncontinence Careapi-308965846No ratings yet
- Midwife-Led Units, Community Midwifery Units and Birth CentresDocument13 pagesMidwife-Led Units, Community Midwifery Units and Birth CentresLara AldazNo ratings yet
- FOSTERING DIGNITY AND RESPECT IN CARE NewDocument5 pagesFOSTERING DIGNITY AND RESPECT IN CARE NewSidra Waqar KhanNo ratings yet
- FOSTERING DIGNITY AND RESPECT IN CARE NewDocument5 pagesFOSTERING DIGNITY AND RESPECT IN CARE NewSidra Waqar Khan100% (2)
- Nursing As A Profession: by Jeelani SaimaDocument53 pagesNursing As A Profession: by Jeelani Saimajeelani saimaNo ratings yet
- 0010 - ETHOS OF NURSING PRACTICE Full Note PDFDocument48 pages0010 - ETHOS OF NURSING PRACTICE Full Note PDFRicardo Domingos100% (1)
- Research TitleDocument4 pagesResearch TitlebnellaNo ratings yet
- Principles and Fundamentals of NursingDocument1,060 pagesPrinciples and Fundamentals of Nursingkariuki90406978No ratings yet
- C304 Task 1 Word A PDFDocument33 pagesC304 Task 1 Word A PDFCamille Joy BaliliNo ratings yet
- Nurses' Roles and Responsibilities in Providing Care and Support at The End of LifeDocument10 pagesNurses' Roles and Responsibilities in Providing Care and Support at The End of Lifededsec hackerNo ratings yet
- Perioperative NursingDocument103 pagesPerioperative NursingRochelle Anne SorioNo ratings yet
- Introduction To NDocument42 pagesIntroduction To NS. KNo ratings yet
- Gibbs Reflective Journal SampleDocument4 pagesGibbs Reflective Journal SampleCres Padua Quinzon100% (2)
- Clinical Methods: Nursing RoundsDocument7 pagesClinical Methods: Nursing RoundsYAMINIPRIYANNo ratings yet
- LeiningerDocument36 pagesLeiningerAshley EmperadorNo ratings yet
- Presentation Transcultural NursingDocument23 pagesPresentation Transcultural NursingHazel Eñga Tiam Wat100% (2)
- AdvocacyinnursingDocument5 pagesAdvocacyinnursingjkm36403No ratings yet
- Futuristic NursingDocument14 pagesFuturistic NursingHarpreet Dhatt50% (4)
- Chapter 1-3Document26 pagesChapter 1-3Jemimah Ruth Madayag Valenzuela100% (1)
- #175670601Document5 pages#175670601freelance writerNo ratings yet
- Fundamentals of Professional NursingDocument50 pagesFundamentals of Professional NursingKwasi PatrickNo ratings yet
- Autonomy, HospitalityDocument12 pagesAutonomy, HospitalityDr. Mohammed SayedNo ratings yet
- Log 3 NIP1003: C Bogateanu M00526321Document6 pagesLog 3 NIP1003: C Bogateanu M00526321trandafirashNo ratings yet
- Nursing ServiceDocument97 pagesNursing ServicePragyashaa ChaudharyNo ratings yet
- Fundamentals of Nursing - 1Document1,794 pagesFundamentals of Nursing - 1Emmanuel Kiprono100% (1)
- Code of Ethics: RightsDocument15 pagesCode of Ethics: Rightsmarilen099No ratings yet
- Nursing Ethnography Final DraftDocument9 pagesNursing Ethnography Final Draftapi-315823367No ratings yet
- 9780199237838Document11 pages9780199237838Jasmine Ann Catherine Price100% (1)
- Florence Nightingale (Environmental Theory)Document23 pagesFlorence Nightingale (Environmental Theory)Irah A.No ratings yet
- Faye Glenn Abdellah S Nursing TheoryDocument11 pagesFaye Glenn Abdellah S Nursing TheoryJeffrey Ian M. KoNo ratings yet
- 2022 Nurses Week PresentationDocument19 pages2022 Nurses Week PresentationMargaret DigitemieNo ratings yet
- The Role of The Charge Nurse: What I Believe It To Be, Why I Am Here and What I Could Offer To The RoleDocument25 pagesThe Role of The Charge Nurse: What I Believe It To Be, Why I Am Here and What I Could Offer To The RoleAlan George BevanNo ratings yet
- Nursing TheoriesDocument3 pagesNursing TheoriesAyessa Camelle DumileNo ratings yet
- Leininger2 - Culture Care Universality & DiversityDocument32 pagesLeininger2 - Culture Care Universality & Diversitymao ayunan (misaki minna ayunan)No ratings yet
- TransculturalDocument13 pagesTransculturalDONALDNo ratings yet
- Patient Autonomy A View From The KitchenDocument10 pagesPatient Autonomy A View From The KitchenTin Ker JoNo ratings yet
- Nursing TheoristsDocument97 pagesNursing TheoristsMarti GregorioNo ratings yet
- Example Literature Review Hand WashingDocument7 pagesExample Literature Review Hand Washingmtxziixgf100% (1)
- Program ProposalDocument14 pagesProgram ProposalJoey Dee Bravo100% (1)
- Faye Glenn AbdellahDocument12 pagesFaye Glenn AbdellahAnnapurna Dangeti100% (1)
- Assessment 2 Cultural SafetyDocument2 pagesAssessment 2 Cultural SafetyMahal PaetNo ratings yet
- Nursing FoundationDocument200 pagesNursing FoundationManu CvNo ratings yet
- Mortensene ApasafetyqualityDocument5 pagesMortensene Apasafetyqualityapi-284786443No ratings yet
- cs4 Case StudyDocument7 pagescs4 Case Studyapi-436279390No ratings yet
- Nursing Autonomy and Responsibilities To Family MembersDocument4 pagesNursing Autonomy and Responsibilities To Family MembersKoEy Are UNo ratings yet
- Nursng ReportDocument19 pagesNursng ReportNgurahNo ratings yet
- Nursing TheoriesDocument7 pagesNursing TheoriesemsdaxxNo ratings yet
- A Case Study From A Cultural PerspectiveDocument4 pagesA Case Study From A Cultural Perspectiveapi-436279390No ratings yet
- Trancultural Nursing: EssayDocument6 pagesTrancultural Nursing: EssayJoko Tri WahyudiNo ratings yet
- Retro-Fitting L-Type Mudguards:: Aug-10 Mglret DsDocument4 pagesRetro-Fitting L-Type Mudguards:: Aug-10 Mglret DsmamatnamakuNo ratings yet
- Toolkit Included in The Toolkit: DATA SHEET: Ds-Toolkit ISSUE S1001Document2 pagesToolkit Included in The Toolkit: DATA SHEET: Ds-Toolkit ISSUE S1001mamatnamakuNo ratings yet
- Suspension Block AssemblyDocument1 pageSuspension Block AssemblymamatnamakuNo ratings yet
- Wheels Rims and Spokes Important Information: DATA SHEET: Ds-Wheel ISSUE S1004Document1 pageWheels Rims and Spokes Important Information: DATA SHEET: Ds-Wheel ISSUE S1004mamatnamakuNo ratings yet
- Fig GTR1: Aug-10 Gtrigb3 DsDocument3 pagesFig GTR1: Aug-10 Gtrigb3 DsmamatnamakuNo ratings yet
- Derailleur Chain Tensioner Idlers Etc.: Fig CT4Document1 pageDerailleur Chain Tensioner Idlers Etc.: Fig CT4mamatnamakuNo ratings yet
- These Notes Relate Mainly To Fitting A New Pillar, But They May Also Be Helpful When Exchanging Certain PartsDocument2 pagesThese Notes Relate Mainly To Fitting A New Pillar, But They May Also Be Helpful When Exchanging Certain PartsmamatnamakuNo ratings yet
- BS en 14885-2015Document64 pagesBS en 14885-2015mamatnamaku100% (3)
- INTR - Indonesia National Trade Repository PDFDocument4 pagesINTR - Indonesia National Trade Repository PDFmamatnamakuNo ratings yet
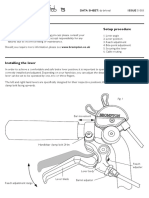
- Brake Lever Setup Important Information Setup Procedure: DATA SHEET: Ds-Brleval ISSUE S1003Document2 pagesBrake Lever Setup Important Information Setup Procedure: DATA SHEET: Ds-Brleval ISSUE S1003mamatnamakuNo ratings yet
- Lamp Brackets / Battery Lights.: Jan-12 Batlam DsDocument4 pagesLamp Brackets / Battery Lights.: Jan-12 Batlam DsmamatnamakuNo ratings yet
- Derailleur Chain Tensioner Idlers Etc.: Fig CT4Document1 pageDerailleur Chain Tensioner Idlers Etc.: Fig CT4mamatnamakuNo ratings yet
- This Luggage Item Is NOT Suitable For Use With A Brompton S-Type ModelDocument2 pagesThis Luggage Item Is NOT Suitable For Use With A Brompton S-Type ModelmamatnamakuNo ratings yet
- CHAIN TENSIONER DISC Cta - DsDocument4 pagesCHAIN TENSIONER DISC Cta - DsAgus SujantoNo ratings yet
- Derailleur Chain Tensioner Idlers Etc.: Fig CT4Document1 pageDerailleur Chain Tensioner Idlers Etc.: Fig CT4mamatnamakuNo ratings yet
- BS en 16615-2015Document44 pagesBS en 16615-2015mamatnamaku100% (7)
- BS en 16616-2015Document40 pagesBS en 16616-2015mamatnamaku100% (3)
- Fibrous JointDocument5 pagesFibrous JointmamatnamakuNo ratings yet
- BS en 01040-2005Document44 pagesBS en 01040-2005mamatnamaku100% (5)
- Validation EtoDocument8 pagesValidation EtomamatnamakuNo ratings yet
- Xtrail t32Document113 pagesXtrail t32mamatnamakuNo ratings yet
- BS en 01040-2005Document44 pagesBS en 01040-2005mamatnamaku100% (5)
- DJI Spark DesignDocument1 pageDJI Spark DesignmamatnamakuNo ratings yet
- E ShoppingDocument11 pagesE ShoppingZil ShahNo ratings yet
- Virtualization: Old Technology Offers Huge New Potential: Greg GothDocument4 pagesVirtualization: Old Technology Offers Huge New Potential: Greg GothmamatnamakuNo ratings yet
- Cdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008Document158 pagesCdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008fuentenatura100% (1)
- Class II Special Controls Guidance Document Surgical SuturesDocument12 pagesClass II Special Controls Guidance Document Surgical Sutures601026No ratings yet
- Computer Science: From Wikipedia, The Free EncyclopediaDocument15 pagesComputer Science: From Wikipedia, The Free EncyclopediamamatnamakuNo ratings yet
- Pembagian Kelas Alat Kesehatan Perkategori ProdukDocument41 pagesPembagian Kelas Alat Kesehatan Perkategori Produkdimitrijm100% (1)
- 1-A Business Model Framework For The Design and Evaluation of Business Models in The Internet of ServicesDocument13 pages1-A Business Model Framework For The Design and Evaluation of Business Models in The Internet of ServicesmamatnamakuNo ratings yet
- Proc PDF FileDocument8 pagesProc PDF FileVivek GutamNo ratings yet
- Management of Patients With Hepatocellular Carcinoma (HCC) : H P B (HPB) F C GDocument15 pagesManagement of Patients With Hepatocellular Carcinoma (HCC) : H P B (HPB) F C GFloyd balansagNo ratings yet
- UPSIDC Bylaws 17052017 PDFDocument193 pagesUPSIDC Bylaws 17052017 PDFPraveen kumarNo ratings yet
- Eaglet Volume 56 # 3 SY 2009-2010Document40 pagesEaglet Volume 56 # 3 SY 2009-2010Mara Melanie D. PerezNo ratings yet
- Medical Tourism in IndiaDocument23 pagesMedical Tourism in IndiaIndu ShekharNo ratings yet
- Annual Report 2008Document32 pagesAnnual Report 2008vnatcNo ratings yet
- Lhay Project UnfinishedDocument26 pagesLhay Project UnfinishedLhay WafuNo ratings yet
- Lone Star Shopper: Johnnie StoneDocument12 pagesLone Star Shopper: Johnnie StoneCoolerAdsNo ratings yet
- Nowell Ona CVDocument3 pagesNowell Ona CVNowell Ona AdmsNo ratings yet
- Kibera Mirror MayDocument8 pagesKibera Mirror Mayvincent achuka maisibaNo ratings yet
- Starting A PharmacyDocument8 pagesStarting A PharmacyLloyd Fyl O. RazoNo ratings yet
- FIP PharmabridgeDocument2 pagesFIP PharmabridgeInternational Pharmaceutical Students' Federation (IPSF)No ratings yet
- DM PH&SD P4 TG17 (Guidelines+for+First Aid+Requirement)Document0 pagesDM PH&SD P4 TG17 (Guidelines+for+First Aid+Requirement)ahmedspecbvNo ratings yet
- Posttest. Renal DisordersDocument3 pagesPosttest. Renal Disordersjbagacay100% (3)
- Some RRLDocument3 pagesSome RRLOmar Christian TuazonNo ratings yet
- TDocument5 pagesTShwardz PamittanNo ratings yet
- SPF's Love and Peace MagazineDocument80 pagesSPF's Love and Peace MagazinekishwarNo ratings yet
- 1Document94 pages1Emanuel Acray Nkondola100% (2)
- 27th SFTC Biam BograDocument5 pages27th SFTC Biam BograPritam RoyNo ratings yet
- Case Study:: Maitreya-Buddha PyramidDocument3 pagesCase Study:: Maitreya-Buddha PyramidShreenivasan Muthukumarasamy100% (6)
- 2017 UB04 Hospital Instructions-Final 8FEB2018Document99 pages2017 UB04 Hospital Instructions-Final 8FEB2018krishna EnagaluruNo ratings yet
- A Study On Effectiveness of Promotional Strategy of AMRI Hospital DhakuriaDocument53 pagesA Study On Effectiveness of Promotional Strategy of AMRI Hospital DhakuriaGourab Majumder50% (2)
- Organogram HospitalDocument1 pageOrganogram HospitalNisha BhimsariaNo ratings yet
- Healing Gardens FinalDocument20 pagesHealing Gardens FinalMohd Salahuddin100% (1)
- Professor HieronimusDocument341 pagesProfessor Hieronimusbob robNo ratings yet
- To Whom It May ConcernDocument8 pagesTo Whom It May ConcernKaren EstavilloNo ratings yet
- Thyroidectomy NCPDocument3 pagesThyroidectomy NCPKim Enrico Jumarang100% (2)
- INVESTMENT MEMO - TanzaniteDocument5 pagesINVESTMENT MEMO - TanzaniteSuresh PoojariNo ratings yet
- London'S Top 50 Wellbeing Gurus: Thelondonnews ThelondonnewsDocument1 pageLondon'S Top 50 Wellbeing Gurus: Thelondonnews ThelondonnewsAlireza HemmatiNo ratings yet
- Patient Safety and Patient Assessment in Pre-Hospital Care: A Study ProtocolDocument7 pagesPatient Safety and Patient Assessment in Pre-Hospital Care: A Study ProtocolDeby KurniawanNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- Breaking the Habit of Being YourselfFrom EverandBreaking the Habit of Being YourselfRating: 4.5 out of 5 stars4.5/5 (1459)
- Briefly Perfectly Human: Making an Authentic Life by Getting Real About the EndFrom EverandBriefly Perfectly Human: Making an Authentic Life by Getting Real About the EndNo ratings yet
- No Mud, No Lotus: The Art of Transforming SufferingFrom EverandNo Mud, No Lotus: The Art of Transforming SufferingRating: 5 out of 5 stars5/5 (175)
- The Happiest Baby on the Block: The New Way to Calm Crying and Help Your Newborn Baby Sleep LongerFrom EverandThe Happiest Baby on the Block: The New Way to Calm Crying and Help Your Newborn Baby Sleep LongerRating: 4.5 out of 5 stars4.5/5 (58)
- Prisoners of Geography: Ten Maps That Explain Everything About the WorldFrom EverandPrisoners of Geography: Ten Maps That Explain Everything About the WorldRating: 4.5 out of 5 stars4.5/5 (1145)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipFrom EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipRating: 4.5 out of 5 stars4.5/5 (1135)
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissFrom EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissRating: 4.5 out of 5 stars4.5/5 (82)
- Peaceful Sleep Hypnosis: Meditate & RelaxFrom EverandPeaceful Sleep Hypnosis: Meditate & RelaxRating: 4.5 out of 5 stars4.5/5 (142)
- The Bridesmaid: The addictive psychological thriller that everyone is talking aboutFrom EverandThe Bridesmaid: The addictive psychological thriller that everyone is talking aboutRating: 4 out of 5 stars4/5 (131)
- Neville Goddard Master Course to Manifest Your Desires Into Reality Using The Law of Attraction: Learn the Secret to Overcoming Your Current Problems and Limitations, Attaining Your Goals, and Achieving Health, Wealth, Happiness and Success!From EverandNeville Goddard Master Course to Manifest Your Desires Into Reality Using The Law of Attraction: Learn the Secret to Overcoming Your Current Problems and Limitations, Attaining Your Goals, and Achieving Health, Wealth, Happiness and Success!Rating: 5 out of 5 stars5/5 (284)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- For Women Only, Revised and Updated Edition: What You Need to Know About the Inner Lives of MenFrom EverandFor Women Only, Revised and Updated Edition: What You Need to Know About the Inner Lives of MenRating: 4.5 out of 5 stars4.5/5 (271)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- My Little Brother: The unputdownable, page-turning psychological thriller from Diane SaxonFrom EverandMy Little Brother: The unputdownable, page-turning psychological thriller from Diane SaxonRating: 4.5 out of 5 stars4.5/5 (38)
- 369: Manifesting Through 369 and the Law of Attraction - METHODS, TECHNIQUES AND EXERCISESFrom Everand369: Manifesting Through 369 and the Law of Attraction - METHODS, TECHNIQUES AND EXERCISESRating: 5 out of 5 stars5/5 (50)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (393)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Summary of The Art of Seduction by Robert GreeneFrom EverandSummary of The Art of Seduction by Robert GreeneRating: 4 out of 5 stars4/5 (46)
- The Secret Teachings Of All Ages: AN ENCYCLOPEDIC OUTLINE OF MASONIC, HERMETIC, QABBALISTIC AND ROSICRUCIAN SYMBOLICAL PHILOSOPHYFrom EverandThe Secret Teachings Of All Ages: AN ENCYCLOPEDIC OUTLINE OF MASONIC, HERMETIC, QABBALISTIC AND ROSICRUCIAN SYMBOLICAL PHILOSOPHYRating: 4.5 out of 5 stars4.5/5 (4)