Professional Documents
Culture Documents
Edwar Yersinia
Uploaded by
Divya JayaramanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Edwar Yersinia
Uploaded by
Divya JayaramanCopyright:
Available Formats
JOURNAL OF CLINICAL MICROBIOLOGY, June 1985, p.
914-918
Vol. 21, No. 6
0095-1137/85/060914-05$02.00/0 Copyright 1985, American Society for Microbiology
Rapid Microbiochemical Method for Presumptive Identification of Gastroenteritis-Associated Members of the Family Enterobacteriaceae
DAVID C. T. YONG,1 J. STEPHEN THOMPSON,2* AND ANNE PRYTULA' Laboratory Services Branch, Ontario Ministry of Health, Windsor Regional Public Health Laboratory, Windsor N9A 6S2,1 and Peterborough Regional Public Health Laboratory, Peterborough K9J 6 Y8,2 Ontario, Canada
Received 4 December 1984/Accepted 18 March 1985
A method for rapid screening of isolates of pathogenic members of the family Enterobacteriaceae is described. Flow charts are used in conjunction with triple sugar iron agar, o-nitrophenyl-3-D-galactopyranoside-phenylalanine-motility sulfate screening media, oxidase test, and six rapid biochemical tests, namely, lysine decarboxylase, urease, indole, esculin hydrolysis, malonate, and xylose. This scheme is used to provide an inexpensive but rapid presumptive identification of Salmonella, Shigella, Edwardsiella, Aeromonas, Plesiomonas, Vibrio, and Yersinia isolates from stool cultures.
In clinical bacteriology, rapid identification of bacteria that cause gastroenteritis is essential for diagnostic, epidemiological, and public health reasons. When large numbers of fecal specimens are processed by a laboratory, there is a need for rapid screening of negative specimens and confirmation of positive specimens. A methodology that can reduce turn-around time by 1 day is therefore extremely useful. In our laboratories, the search for enteric pathogens consists of initial screening by a two-tube method, triple sugar iron (TSI) agar and o-nitrophenyl-,3-D-galactopyranoside-phenylalanine motility (ONPG-PA-M) sulfate agar (13), before confirmation by additional biochemical and serological testing. A 4-h rapid microbiochemical (RM) method is described for presumptive identification of pathogenic enteric bacteria. This method, in which small amounts of media are used with large inocula of bacteria, is based on methods previously described for the identification of Neisseria gonorrhoeae, Gardnerella vaginalis, and corynebacteria (14, 16, 17). We have also proposed a series of flow charts, based on key reactions, for using the RM tests to select appropriate further tests for each isolate. This approach is similar to that used by Shayegani et al. (11) for identifying nonfermentative gram-negative bacilli. The chart design is similar to that used by Ellner et al. (5) for identification of anaerobes. This method is intended to screen for species of Salmonella, Shigella, Edwardsiella, Aeromonas, Plesiomonas, Vibrio, and Yersinia in fecal samples. It is not intended for complete identification, nor is it intended for identification of organisms from other types of specimens.
MATERIALS AND METHODS Cultures. A total of 1,475 clinical isolates from stool samples were examined, including 626 Salmonella, 24 Shigella, 215 Escherichia coli, 73 Enterobacter, 62 Proteus, 35 Providencia, 320 Citrobacter, 36 Klebsiella, 23 Serratia, 1
*
Corresponding author.
914
Edwardsiella tarda, 1 Vibrio cholerae, 4 Aeromonas hydrophila, 2 Plesiomonas shigelloides, 46 Yersinia, and 7 Arizona (Salmonella subgenus III) isolates. In addition, 24 stock cultures of enteric organisms were obtained from the Central Public Health Laboratory, Ontario Ministry of Health, Toronto, Canada. All organisms were initially isolated on one or more of the following enteric isolation media: modified salmonella-shigella agar (Oxoid Ltd.), MacConkey agar (GIBCO Diagnostics), cefsulodin-irgasan-novobiocin agar (10), thiosulfate citrate bile sucrose cholera medium (Oxoid), and bismuth sulfite agar (Oxoid). Single-colony isolates from enteric isolation media were inoculated into slants of TSI agar (GIBCO) and tubes of ONPG-PA-M sulfate medium (13), followed by incubation at 36C for 18 to 24 h. Each isolate was identified by using API 20E (Analytab Products). Growth from the TSI slant was used to inoculate the following RM and conventional substrates: lysine decarboxylase, indole, urea, esculin, malonate, and xylose. Oxidase tests were performed with filter paper impregnated with a freshly prepared 1% solution of N,N,N',N'-tetramethyl-p-phenylenediamine dihydrochloride (Sigma Chemical Co.). Inoculum from TSI agar was rubbed on the filter paper with a sterile platinum loop. Salmonella serology was performed with omnivalent 0 + Vi and omnivalent H antisera obtained from the Enteric Reference Section, Central Public Health Laboratory, Toronto. The 0 + Vi antiserum contained 0 groups A to W as well as Vi antiserum. Slide agglutinations were performed in each antiserum and a phenolized saline control with growth from a TSI agar slant. Preparation of RM media. Media for the RM biochemical tests were prepared as follows. Lysine decarboxylase broth contained 0.5 g of Moeller decarboxylase base (Difco Laboratories), 0.5 g of L-lysine hydrochloride (Sigma); and 25 ml of distilled water; pH was adjusted to 6.2 with 1 N NaOH. Decarboxylase control broth contained 0.5 g of Moeller decarboxylase base (Difco) and 25 ml of distilled water; pH was adjusted to 6.2 with 1 N NaOH. Tryptophane broth for indole determination contained 1 g of tryptose (Difco) and 25 ml of distilled water; pH was adjusted to 7.4 with 1 N NaOH. Urea broth contained 25 ml of "urea base" and 2.0 g of urea
VOL. 21, 1985
TABLE 1. Comparison of RM and conventional biochemical reactions of clinical isolates No. of No. (%) of Substrate reactions in specimens
tested
ENTEROBACTERIACEAE IDENTIFICATION
915
TABLE 3. Guide for chart selection
TEST
A Test results' indicating use of the following chart: D E B C F
agreement
H2Sb
Lysine
Urease Indole Esculin Malonate
Xylose
1,475 1,475 1,475 1,122 1,315 1,122
1,475 1,472 1,475 1,122 1,311 1,116
(100) (99.8) (100) (100) (99.7) (99.5)
TSI Slant Butt Gas
PA
-
A A -
A A +
-
K A +
-
K A
-
(crystalline; Sigma); pH was adjusted to 7.0 with 1 N NaOH. (Urea base contained 0.01 g of yeast extract [Difco], 0.01 g of monopotassium phosphate, and 100 ml of distilled water.) Esculin broth contained 0.03 g of esculin hydrate crystalline (Sigma), 0.02 g of ferric citrate, 0.3 g of Bacto-Peptone (Difco), 0.17 g of sodium chloride, and 25 ml of distilled water; pH was adjusted to 7.2 with 1 N NaOH. Xylose broth contained 25 ml of RM base and 0.5 g of xylose (Sigma); pH was adjusted to 7.3 with 1 N sodium hydroxide (RM base contained 2.0 g of Casamino Acids [certified; Difco], 0.03 g of L-cysteine hydrochloride [Sigma], 0.03 g of sodium sulfate, 2.5 g of neopeptone [Difco], 0.1 g of phenol red, and 100 ml of distilled water). Malonate broth contained 0.2 g of malonate broth (Difco), 0.03 g of bromothymol blue, and 25
ml of distilled water. All RM media were filter sterilized with a membrane filter (pore size, 0.2 ,um; Nalgene small sterilization filter unit; Sybron/Nalge) and stored at 2 to 8C in glass dropper bottles. Preparation of conventional media. Lysine decarboxylase broth and decarboxylase control broth were made as described in the directions of the manufacturer with Moeller decarboxylase base (Difco) and L-lysine hydrochloride
ONPG
Test results: A, acid; K, alkaline; +, positive; -, negative. b H,S production may be determined from TSI agar or ONPG-PA-M sulfate medium.
(Sigma). Tryptose broth for indole determination consisted of 10 g of tryptose (Difco), 5 g of sodium chloride, and 1,000 ml of distilled water. Urea agar slants consisted of urea agar base and 40% urea (Oxoid) and were made as described in the directions of the manufacturer. Esculin agar slants (15) consisted of 1 g of esculin (Sigma), 0.5 g of ferric citrate, 40 g of heart infusion agar (Difco), and 1,000 ml of distilled water. Xylose broth (15) consisted of 22.5 g of heart infusion broth (Difco), 10 g of xylose (Sigma), 0.02 g of bromocresol purple, and 1,000 ml of distilled water. Malonate broth (Difco) was made as described in the directions of the manufacturer. Method of inoculation of RM substrates. Just before use, approximately 0.05 ml (1 drop) of each sterile medium was dispensed into sterilized microtubes (disposable borosilicate glass, 6 by 50 mm; Kimble). The tubes were placed in microtiter V plates (Dynatech Laboratories, Inc.), and the media were allowed to warm to room temperature (22C)
TABLE 2. Presumptive identification of 24 stock cultures by using the RM and flow chart method
Organism
LYS URE Reactions in RM tests' IND ESC MAL XYL
Flow chart result
+ Salmonella typhi + Salmonella typhimurium + Salmonella newport Salmonella paratyphi A + Salmonella paratyphi B + Arizona sp. Shigella flexneri Shigella sonnei Yersinia enterocolitica Yersinia intermedia Yersinia frederiksenii Yersinia kristensenii Yersinia pseudotuberculosis + Escherichia coli Proteus mirabilis Providencia rettgeri Providencia stuartii Citrobacter freundii + Edwardsiella tarda Enterobacter cloacae + Klebsiella pneumoniae + Serratia marcescens + Vibrio cholerae Aeromonas hydrophila " Abbreviations: LYS, lysine decarboxylase; URE,
Possible Salmonella (S. typhi) Possible Salmonella sp. Possible Salmonella sp. Posssible Salmonella paratyphi A Possible Salmonella sp. Possible Arizona sp. + Possible Shigella sp. Possible Shigella sp. + Possible Yersinia sp. + + + + Possible Yersinia sp. + + + + Possible Yersinia sp. + + Possible Yersinia sp. + + Possible Yersinia sp. + + Discard + + + Discard + + Discard + + + Discard + + + Discard + + Possible Edwvardsiella sp. + + + Discard + + + Discard + + Discard + Possible Vibrio sp. + + Possible Aeromonas sp. urease; IND, indole; ESC. esculin; MAL. malonate; XYL. xylose; +, positive result; -, negative result.
+ -
+ + + + -
916
YONG, THOMPSON, AND PRYTULA
H2S + PA ONPG TSI A/A H2S Gas PA -
J. CLIN. MICROBIOL.
FIG. 1. Chart A. Scheme for organisms that are H2S positive, PA negative, and ONPG negative. Symbols: -*, positive result; l., , test (as indicated); () , no further negative result; identification necessary (nonpathogenic organism); i, further identification necessary.
<
before inoculation. One-third of a loopful (loop diameter, 3 mm) of pure growth of each isolate (grown for 18 to 24 h on TSI agar slants) was inoculated into each medium. Thorough mixing of inoculum and substrate was necessary to quicken the reaction time. After inoculation, the media in the urea and decarboxylase tubes were overlaid with 2 drops of sterile mineral oil. The inoculated tubes were incubated in a shallow water bath at 36C.
Discard)
FIG. 3. Chart C. Scheme for organisms with an acid slant, an acid butt without gas in TSI agar, and H2S-negative and PA-negative results. Symbols are described in the legend to Fig. 1.
H2S
PA
ONPG
Lysine decarboxylase results were read after 2 h of incubation; a positive test result was indicated by a purple color, provided that the decarboxylase control tube was yellow. The indole result was read in 4 h. After the addition of one drop of Kovac reagent, a positive test produced a red color. All other test results were observed after 2 h, but tubes showing negative reactions were incubated for a total of 4 h. A positive urease test was indicated by a pink color. A positive malonate test was blue, and a negative test was green. In the esculin test, a positive result was indicated by development of a black color. A positive xylose test was yellow and a negative test was red.
RESULTS Table 1 shows 99.8% agreement between test results obtained with conventional and RM methods in 7,984 individual tests. All RM reactions were complete within 4 h, although with most substrates, positive reactions were apparent within 2 h of inoculation. Urease, malonate, and xylose tests yielded more positive reactions in the conventional tests than in the RM tests, with three, four, and six discrepancies, respectively. Three Klebsiella isolates showed false-negative urease results; three Escherichia coli, two Providencia, and one Serratia isolate showed false-negative xylose results; and two Klebsiella and two Enterobacter isolates showed false-negative malonate results with RM media. Tests which were negative by the RM method but positive with conventional substrates were considered to be false-negative. Table 2 shows the reactions of 24 stock cultures tested by the RM method. All RM results agreed with those of
FIG. 2. Chart B. Scheme for organisms that are H2S positive, PA negative, and ONPG positive. Symbols are described in the legend to Fig. 1.
VOL. 21, 1985
ENTEROBACTERIACEAE IDENTIFICATION
917
conventional tests and with published results for each species (3, 4, 6). All Salmonella, Shigella, Edwardsiella tarda, Vibrio cholerae, Aeromonas hydrophila group, Plesiomonas shigelloides, and Yersinia enterocolitica isolates were detected by this system. This included one lactose-positive stock culture of Salmonella newport that was H2S negative in TSI agar. DISCUSSION Good correlation (99.8%) was demonstrated between the RM and conventional biochemical tests. There were discrepancies in 13 individual tests, with the RM tests appearing to be undersensitive in each instance. None of the discrepancies occurred in a test critical to the identification of the organism involved. Other papers have described rapid tests for screening of enteric pathogens (2, 9, 12), esculin tests (8), and identification schemes (7). Burns et al. (1) have proposed an extensive series of flow charts to aid in the identification ofboth fermentative and nonfermentative gramnegative bacteria. The proposed method facilitates the discarding of isolates which have no clinical relevance without extensive identification. In this regard, an important screening step is the use of a positive phenylalanine deaminase (PA) reaction to screen for Proteus, Providencia, and Morganella spp., which are discarded as normal enteric flora without further biochemical testing. Table 3 directs the investigation into one of the flow charts
TSI A/A
Possible
H2S Gas PA
+
-
Shigella (Aerogenic)
FIG. 5. Chart E. Scheme for organisms with an alkaline slant, an acid butt with gas in TSI agar, and H2S-negative and PA-negative results. Symbols are described in the legend to Fig. 1.
an
FIG. 4. Chart D. Scheme for organisms that have an acid slant, acid butt with gas in TSI agar, and H2S-negative and PA-negative results. Symbols are described in the legend to Fig. 1.
based on reactions obtained in the preliminary screening media, TSI and ONPG-PA-M sulfate. Figure 1 is the simplest chart and would probably be the most extensively used in a laboratory processing a large number of Salmonella spp. isolates. The key is the same for all six flow charts. Each symbol gives processing directions. For each substrate all arrows from the right-hand apex represent positive reactions. The ovoid discard symbol means that the organism has been screened as a nonpathogen and no further identification is necessary. The rectangular identify symbol means that further identification is necessary to confirm the presumptive identification or to differentiate between several possibilities. Identification was performed by using API 20E during this project, but other systems or conventional testing could be used. For these flow charts, the TSI reactions, PA, ONPG, and motility were all derived from the two media used for preliminary screening, TSI slants and ONPG-PA-M sulfate agar. Often, only these reactions would be necessary to produce a preliminary identification. When the charts indicated that more tests were necessary, the remaining substrates were inoculated simultaneously. The flow charts then provided an order in which to interpret test results. Figures 2 through 6 present schemes of various complexities, but the directions for use remain the same. Since the initial study, this scheme has been used routinely in one of our laboratories for 22 months. During this
918
YONG, THOMPSON, AND PRYTULA
TSI K/A H2S Gas PA -
J. CLIN. MICROBIOL.
and Willem vander Kolk and the Regional Audio-Visual staff for the graphics.
LITERATURE CITED 1. Burns, M. C., E. R. Richter, M. S. Rheins, and G. J. Baniwart. 1982. An identification scheme for gram negative fermentative and nonfermentative bacteria. Public Health Lab. 40:86-108. 2. Davis, J. R., C. E. Stager, R. D. Wende, and S. M. H. Qadri. 1981. Clinical laboratory evaluation of the AutoMicrobic system Enterobacteriaceae biochemical card. J. Clin. Microbiol.
14:370-375.
3. Devenish, J. A., and D. A. Schiemann. 1981. An abbreviated scheme for identification of Yersinia enterocolitica isolated from food enrichments in CIN (cefsoludin-iragasan novobiocin) agar. Can. J. Microbiol. 27:937-941. 4. Edwards, P. R., and W. H. Ewing. 1972. Identification of Enterobacteriaceae, 3rd ed. Burgess Publishing Co., Minneapolis, Minn. 5. Ellner, P. D., P. A. Granato, and C. B. May. 1973. Recovery and identification of anaerobes: a system suitable for the routine clinical laboratory. Appl. Microbiol. 26:904-913. 6. Martin, W. J., and J. A. Washington II. 1980. Enterobacteriaceae, p. 195-216. In E. H. Lennette, A. Balows, W. J. Hausler, Jr., and J. P. Truant (ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington, D.C. 7. Nord, C. E., A. A. Lindberg, and A. Dahlback. 1975. Four hour-tests for the identification of Enterobacteriaceae. Med. Microbiol. Immunol. 161:231-238. 8. Qadri, S. M. H., and J. C. Smith. 1982. Rapid degradation of esculin to esculation by gram negative bacteria. Public Health Lab. 40:27-33. 9. Sanders, A. C., and K. Okabe. 1954. A rapid screening method for the isolation of enteric pathogens. Public Health Lab. 12:12-14. 10. Schiemann, D. A. 1979. Synthesis of a selective agar medium for Yersinia enterocolitica. Can. J. Microbiol. 25:1298-1304. 11. Shayegani, M., A. M. Lee, and L. M. Parsons. 1977. A scheme for the identification of nonfermentative gram negative bacteria. Health Lab. Sci. 14:83-94. 12. Stager, C. E., E. Erikson, and J. R. Davis. 1983. Rapid method for detection, identification, and susceptibility testing of enteric pathogens. J. Clin. Microbiol. 17:79-84. 13. Thompson, J. S., and A. A. Borczyk. 1984. Use of a single-tube
Possible Shigells
FIG. 6. Chart F. Scheme for organisms with an alkaline slant, an acid butt with no gas in TSI agar, H2S-negative, and PA-negative results. Symbols are described in the legend to Fig. 1.
period, ca. 21,000 stool cultures were processed, resulting in the detection of the following pathogens: Salmonella spp. (1,712 isolates), Shigella spp. (19 isolates), Yersinia enterocolitica (63 isolates), and Vibrio cholerae (4 isolates). Sixtyseven isolates of nonpathogens which were not screened out by the flow chart scheme but required further identification by API 20E included Citrobacter spp. (28 isolates), anaerogenic Escherichia coli (38 isolates), and Morganella morganii (1 isolate). These RM tests, when used with the flow chart scheme, provide a practical and economical diagnostic tool for dealing with routine enteric bacteriology.
ACKNOWLEDGMENTS We are grateful for the assistance of A. A. Borczyk throughout the project and for review of the manuscript. We also thank S. Toma for critical review, R. Terro, D. S. Hodge, and F. E. Cahoon for advice,
14.
15.
16. 17.
medium, o-nitrophenyl-p-D-galactopyranoside-phenylalaninemotility sulfate, for screening of pathogenic members of the family Enterobacteriaceae. J. Clin. Microbiol. 20:136-137. Thompson, J. S., D. R. Gates-Davis, and D. C. T. Yong. 1983. Rapid microbiochemical identification of Corynebacterium diphtheriae and other medically important corynebacteria. J. Clin. Microbiol. 18:926-929. Vera, J. S., and D. A. Power. 1980. Culture media, p. 965-999. In E. H. Lennette, A. Balows, W. J. Hausler, Jr., and J. P. Truant (ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington, D.C. Yong, D. C. T., and A. Prytula. 1978. Rapid micro-carbohydrate test for confirmation of Neisseria gonorrhoeae. J. Clin. Microbiol. 8:643-647. Yong, D. C. T., and J. S. Thompson. 1982. Rapid microbiochemical method for identification of Gardnerella (Haemophilus) vaginalis. J. Clin. Microbiol. 16:30-33.
You might also like
- Iggagainst Rehsus PDFDocument4 pagesIggagainst Rehsus PDFDivya JayaramanNo ratings yet
- ch1 PDFDocument14 pagesch1 PDFDivya JayaramanNo ratings yet
- Altrnat For FbsDocument56 pagesAltrnat For FbsDivya JayaramanNo ratings yet
- Antibacterial Activity of Silver Nanoparticles Synthesized by Fusarium Oxysporum StrainDocument5 pagesAntibacterial Activity of Silver Nanoparticles Synthesized by Fusarium Oxysporum StrainDivya JayaramanNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Co DR Rajagopal, 4Th Street Arokiya Nagar, NK Road, Near Eb Colony, Thanjavur, Tamilnadu.,613005Document16 pagesCo DR Rajagopal, 4Th Street Arokiya Nagar, NK Road, Near Eb Colony, Thanjavur, Tamilnadu.,613005Rahul GNo ratings yet
- Safety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/ UndertakingDocument12 pagesSafety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/ UndertakingWashington MejiaNo ratings yet
- Gambaran Dan Lesi Rahang Pada Radiograf: Border Periosteal ReactionDocument6 pagesGambaran Dan Lesi Rahang Pada Radiograf: Border Periosteal ReactionI Dewa Ayu SavitriNo ratings yet
- Formulation of Accident Prevention ProgrammeDocument24 pagesFormulation of Accident Prevention ProgrammeCHANDUNo ratings yet
- KJFP003 01 06Document17 pagesKJFP003 01 06Mai Thiện NhânNo ratings yet
- Soal Teks Advertisement 1 (Jawaban)Document14 pagesSoal Teks Advertisement 1 (Jawaban)Bona LiongNo ratings yet
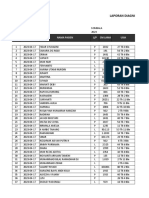
- Laporan Diagnosa Pasien Harian: Puskesmas: TanggalDocument9 pagesLaporan Diagnosa Pasien Harian: Puskesmas: TanggalRamlawatiNo ratings yet
- ZIRCONIA: Most Durable Tooth-Colored Crown Material in Practice-Based Clinical StudyDocument4 pagesZIRCONIA: Most Durable Tooth-Colored Crown Material in Practice-Based Clinical StudygmacaneataNo ratings yet
- Benefits of JCI and ISO AccreditationDocument7 pagesBenefits of JCI and ISO AccreditationOdesa AvilesNo ratings yet
- Chapter 47Document11 pagesChapter 47Aziil LiizaNo ratings yet
- COVID in Children - AdvisoryDocument2 pagesCOVID in Children - AdvisorySMN CV APPLICATIONSNo ratings yet
- High Capacity Stacker-F1-G1-H1 Safety Guide en - USDocument14 pagesHigh Capacity Stacker-F1-G1-H1 Safety Guide en - UShenry lopezNo ratings yet
- 2 - Student Handout 2.1a - Blood Test Data - RevisedDocument9 pages2 - Student Handout 2.1a - Blood Test Data - RevisedDefault AccountNo ratings yet
- DraftRajasthan State Women PolicyDocument29 pagesDraftRajasthan State Women PolicyAADYA SHARMANo ratings yet
- Ebook Ekg Plain and Simple 4Th Edition Ellis Test Bank Full Chapter PDFDocument30 pagesEbook Ekg Plain and Simple 4Th Edition Ellis Test Bank Full Chapter PDFalexandercampbelldkcnzafgtw100% (6)
- Document PDFDocument273 pagesDocument PDFHNINNo ratings yet
- Clinical Instr Job DescriptionDocument2 pagesClinical Instr Job DescriptionAhmad Khalil Al SadiNo ratings yet
- Acceptance and Commitment Therapy in Cancer: Review of Applications and FindingsDocument27 pagesAcceptance and Commitment Therapy in Cancer: Review of Applications and FindingsJuan Alberto GonzálezNo ratings yet
- Znbjma1977@codental - Uobaghdad.edu - Iq: Ministry of Health Training Dentist 1 Ministry of Health Gradated Dentist 2Document28 pagesZnbjma1977@codental - Uobaghdad.edu - Iq: Ministry of Health Training Dentist 1 Ministry of Health Gradated Dentist 2maryam.saadNo ratings yet
- Placemaking As An Approach of Sustainable Urban Facilities ManagementDocument2 pagesPlacemaking As An Approach of Sustainable Urban Facilities ManagementKeziahjan ValenzuelaNo ratings yet
- Medical Mycosis Lecture on Fungal DiseasesDocument15 pagesMedical Mycosis Lecture on Fungal DiseasesIbraheem YesharNo ratings yet
- Why Abolishing The Insanity Defense Is Unconstitutional in DeathDocument23 pagesWhy Abolishing The Insanity Defense Is Unconstitutional in Deathtim radellNo ratings yet
- Speech TherapyDocument239 pagesSpeech Therapyanyush babayanNo ratings yet
- Uts Module 2Document20 pagesUts Module 2Elvis ViernesNo ratings yet
- The Power of Mental Toughness Building The Foundation For SuccessDocument129 pagesThe Power of Mental Toughness Building The Foundation For Successcontact.iptvviewNo ratings yet
- NRes1 Course Unit 1Document6 pagesNRes1 Course Unit 1Jamie NarcisoNo ratings yet
- Ma de 501Document3 pagesMa de 501Dương NguyễnNo ratings yet
- FluconazoleDocument4 pagesFluconazoleeucaNo ratings yet
- Section 2 PMPDocument69 pagesSection 2 PMPJISHNU SNo ratings yet
- ALLTEST Quotation Sheet-Globiome Society-Maimouna-Senegal-20231016Document2 pagesALLTEST Quotation Sheet-Globiome Society-Maimouna-Senegal-20231016globiomeNo ratings yet