Professional Documents
Culture Documents
Artritis Reumatoide Integrativa
Uploaded by
drmacorOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Artritis Reumatoide Integrativa
Uploaded by
drmacorCopyright:
Available Formats
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Use of this content is subject to the Terms and Conditions
Page 1 of 11
Rakel: Integrative Medicine, 2nd ed.
Copyright 2007 Saunders, An Imprint of Elsevier
chapter 48 Rheumatoid Arthritis
Daniel Muller, MD, PhD Pathophysiology 531 Integrative Therapy 532 Exercise 532 Physical and Occupational Therapy 532 Mind-Body Therapy 532 Nutrition 532 Elimination of Tobacco Use 532 Supplements 532 Botanicals 533 Pharmaceuticals 533 Acupuncture 536 Low-Level Laser Therapy 536 Surgery 536 Therapies to Consider 536 Prevention Prescription 536 Therapeutic Review 537
Pathophysiology
Rheumatoid arthritis (RA) is likely caused by a pathologic immune response in a genetically predisposed person to an environmental insult, likely a viral or bacterial infection. [1] Epidemiologic studies show that genes encoding the class II major histocompatibility antigens are linked to clinical features of RA. The HLADR4 and DR1 proteins present foreign and self-antigens to T cells. These molecules are presumed to play a direct role in the etiology of this autoimmune disease by presenting an arthritogenic viral or bacterial antigen to T cells. However, no organism has been definitively linked to the etiology of RA. Antibiotic therapy with minocycline is helpful in mild disease. However, minocycline may act through direct immunomodulatory or anti-inflammatory effects rather than acting through antibacterial activity. Other genes of the immune, endocrine, and neural systems may contribute to the pathogenesis of RA. The precise pathophysiologic cascade is not yet defined. RA is an autoimmune inflammatory disease in which immunosuppressive drugs constitute the mainstay of therapy. Certain cytokines, such as tumor necrosis factor (TNF), interleukin (IL)-1 and IL-6, appear to play important roles, since inhibitors of these molecules decrease disease activity. [2] [3] [4] [5] Similarly, the importance of the roles of cell surface molecules on B and T cells can be shown when used as targets for immunomodulatory therapy. [2] [3] [4] [6] [7] Nonsteroidal anti-inflammatory drugs (NSAIDs) act to inhibit the enzymes that produce inflammatory prostaglandins, particularly thromboxanes and leukotrienes. The newer NSAIDs preferentially inhibit the cyclo-oxygenase (COX)-2 enzyme that produces certain of these inflammatory molecules. Unfortunately, these COX-2 inhibitors may have increased thrombotic and, hence, cardiovascular risks, and may not have any increased gastroprotection. [8] [9] Celecoxib (Celebrex) is still on the market, albeit with increased warnings; other COX-2 inhibitors have been withdrawn from the market. Omega-3 fatty acids and certain botanicals such as ginger and turmeric also may act through decreasing the production or activity of inflammatory prostaglandins. [10] [11] [12] [13] [14] The neural, endocrine, and immune systems all share communication molecules that interact extensively. Molecules from the hypothalamic-pituitary-adrenal axis, particularly cortisol and corticotropin-releasing
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Page 2 of 11
factor, and from the sympathetic-adrenal-medullary system are linked to disease activity in RA. [15] Corticosteroid drugs have powerful disease-suppressing activity, with equally powerful adverse side effects such as osteoporosis. [16] [17] Prolactin and the estrogenic and androgenic sex hormones have been postulated to play roles as well. Other environmental factors such as nutrition, coffee, and tobacco also may contribute to the increased risk of RA. [18] [19] [20] Stress and psychological factors have been linked to the etiology of RA and to disease exacerbations. [21] In one study, psychological factors and depression accounted for at least 20% of disability in patients with RA, greater than the 14% attributable to articular signs and symptoms. [22] In another study, helplessness had a direct effect on disease activity. [23]
Integrative Therapy
Exercise
Joint pain can inhibit activity, leading to muscle disuse and atrophy. In turn, muscle atrophy can lead to decreased stability of joints. Light weight training can maintain or even increase muscle strength around joints, leading to increased joint stability. Stretching muscles can help decrease flexion contractures. Aerobic exercise improves mood, decreases fatigue, and helps control weight gain. Water exercise can be helpful because it is less stressful on joints, but weight training and walking work better to decrease bone loss (osteoporosis). The Arthritis Foundation has information on programs (1-800-283-7800). Asian exercise disciplines such as Tai Chi and Yoga can also be beneficial. A form of Tai Chi called the range of motion (ROM) dance is particularly suited to persons with disabilities (www.romdance.com ; 1-800488-4940).
Physical and Occupational Therapy
Physical therapy and occupational therapy programs can be invaluable in the treatment of RA. Goals are to improve range of motion and strengthen muscles. Joint protection from deformities can be aided by education and use of splints, orthotics, ambulatory aids, and other devices. Massage and local heat and cold applications can decrease inflammation, increase circulation, and relax muscles.
Mind-Body Therapy
Self-help courses given through the Arthritis Foundation provide information about diseases and medication and can help in developing coping skills. Simply writing in a journal about positive and negative emotions for 15 minutes a day can be powerful medicine, relieving symptoms by 25% or more (see Chapter 98 , Journaling). [24] Meditation has been shown to be helpful for chronic pain. [25] A recent study of meditation in psoriasis, an autoimmune inflammatory skin disease, showed decreased time to clearing the skin disease. [26] There are no published studies investigating the role of meditation in RA. However, a study examining this question is underway (see Chapter 100 , Recommending Meditation).
Nutrition Food Triggers
Fasting clearly decreases symptoms in RA; however, symptoms rapidly recur with the resumption of food intake. [27] A small percentage of people with RA appear to have a food intolerance that exacerbates their disease. However, a much larger number believe that certain foods exacerbate symptoms, but this effect cannot be shown in blinded trials of food exposure. The offending foods are usually dairy products, wheat, citrus, or nuts. An elimination diet for 2 weeks with the reintroduction of the suspected food can be done with or without the supervision of a physician or a nutritionist (see Chapter 86 , Adverse Food Reactions and the Elimination Diet).
Omega-3 and Omega-9 Fatty Acids
Increased intake of omega-3 fatty acids from cold-water fish, such as salmon, and from nuts, such as walnuts, flaxseed, or hempseed, can provide modest improvement in the control of RA. [10] [11] [27] The role of saturated fatty acids (trans fats) in increasing symptoms is unproved; however, in view of their association with cardiovascular disease, reduction in intake is worthwhile (see Chapter 88 , The AntiInflammatory Diet).
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Page 3 of 11
Cooked vegetables and olive oil have been found to be independently protective for the development of RA. Omega-9 fatty acids in olive oil may confer anti-RA activity. [28]
Coffee
A high intake of coffee (four or more cups a day) has been linked to increased risk of RA. [18] [20] Intake should be decreased to below this level, or the patient can switch to green tea, for the possible benefit from its antioxidant polyphenols.
Elimination of Tobacco Use
Smoking causes oxidant stress on connective tissue, as evident from the increased wrinkles seen in longterm smokers. One study has shown an association between smoking and increased risk of RA; therefore, RA patients should be counseled to avoid tobacco. [19]
Supplements Essential Fatty Acids
Omega-3 fatty acids can be increased by dietary means or through supplementation. Approximate doses for supplementation are eicosapentaenoic acid 30 mg/kg/day and docosahexaenoic acid 50 mg/kg/day. [10] [27] Gamma-linolenic acid (GLA), 1.4 to 2.8 gm/day, the equivalent of 6 to 11 gm of borage oil daily, also has been shown to be helpful. [11] Effects may not be felt for 6 weeks or more, and continued improvement may occur after many months.
Antioxidants
Antioxidant vitamins may be helpful in RA, as they seem to be in osteoarthritis. Additionally, vitamin E has some analgesic effects. [12] Vitamin E should be taken at 800 IU daily as mixed tocopherols, and vitamin C at 250 mg twice per day. Selenium can be found in many foods, including nuts; intake should be at least 100 g daily, not to exceed 400 g daily. Recommended intake of calcium to prevent osteoporosis is 1500 mg daily. It is probably prudent to add magnesium at 400 to 750 mg daily and a vitamin D supplement at 800 IU per day. [29]
Botanicals Ginger
Ginger (Zingiber officinale) may have efficacy in RA by inhibiting inflammatory prostaglandins. [13]
Dosage
As the dried root, 1 gm two or three times per day to start; increase up to 4 gm daily. As a tea, 1 gm of dried root steeped in 150 mL of boiling water for 5 to 10 minutes and strained; use 1 cup up to four times daily. It can also be taken in 500-mg capsules for a dose of 1 gm two or three times a day.
Precautions
The stimulation of increased bile flow can cause pain in the presence of cholelithiasis. Other risks include bleeding, hypertension or hypotension, and hypoglycemia.
Turmeric
Turmeric (curcumin) in an open trial has been shown to be similar to NSAIDs in efficacy. [14]
Dosage
As powdered root, 0.5 to 1 gm two or three times daily
Precautions
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Page 4 of 11
Risks include bleeding, gastrointestinal intolerance, and impaired fertility
Echinacea should be avoided by patients with RA, since there have been anecdotal reports of increased symptoms in persons with autoimmune disease.
Pharmaceuticals Nonsteroidal Anti-inflammatory Drugs
NSAIDs can be used short term with minor risk of gastrointestinal toxicity. The long-term use of NSAIDs, particularly in the elderly, poses significant risks for gastrointestinal bleeding. There are many NSAIDs, and many of the newer ones are restricted on some formularies. The classic NSAIDs are ibuprofen (Motrin) used in a dose of 800 mg three times daily and naproxen (Naprosyn) in a dose of 500 mg twice daily. Both have antiplatelet activity. The advantage of using the COX-2 inhibitor, celecoxib, for possible decreased gastrointestinal toxicity has been called into question. [9] Note that celecoxib shares a lack of antiplatelet effects with other newer NSAIDs. These drugs also have the potential for renal toxicity and are no more effective than older NSAIDs. Recent data point to the risk of increased thrombosis in patients taking COX-2 inhibitors who have a preexisting increased risk of thrombosis or cardiovascular disease. [8] Two other COX-2 inhibitors have been withdrawn from the market. Celecoxib is used in a dose of 200 mg twice daily.
Corticosteroids
Corticosteroids can rapidly decrease RA symptoms, often within a few hours at high doses. However, both short- and long-term toxic effects are well known. High and even moderate doses can lead to avascular necrosis of joints such as the hip, knee, or shoulder; luckily, this is a rare occurrence. With proper care and early diagnosis of avascular necrosis, disability and joint replacement may be avoided. With long-term use, osteoporosis is a significant risk with doses above 7.5 mg daily of prednisone or equivalent. Other risks include atherosclerosis, diabetes mellitus, cushingoid features, acne, and infection. Often a minor disease flare can be treated with a moderately high dose such as 30 to 40 mg of prednisone orally and a rapid taper over the course of 1 to 2 weeks. In some patients, a low dose of corticosteroids appears necessary for optional function; prednisone 5 to 7.5 mg daily is often used for this purpose. [16] [17] A common method of treating a flare is to give a long-acting depot preparation such as triamcinolone acetonide (Kenalog) 80 mg intramuscularly. This approach can often control disease for 1 to 2 months, long enough for the slower acting disease-modifying antirheumatic drugs (DMARDs) to start working. For disease flares in isolated joints, once infection is ruled out, an intra-articular injection of triamcinolone 2.5 to 40 mg can be given to control local disease.
A single joint with severely decreased range of motion and increased pain is presumed to be infected until proven otherwise. The patient should be hospitalized overnight for joint aspiration to obtain culture specimens; blood should also be drawn for cultures, followed by administration of intravenous antibiotics until results of culture are known.
Antibiotics
Antibiotics, particularly minocycline (Minocin) in a twice-daily dose of 100 mg, may be useful in patients with less severe disease. [30] Side effects include gastrointestinal intolerance, dizziness, photosensitivity rash, vaginitis, skin and gingival discoloration, and, rarely, hepatic, lung, and kidney injury. The salutary effects of these agents may not be due to their antibacterial activity, because the tetracyclines also show immunomodulatory and anti-inflammatory activities.
Disease-Modifying Antirheumatic Drugs
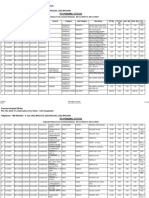
DMARDs are also referred to as slow-acting antirheumatic drugs (SAARDs) because they usually take 6 weeks to 3 months to show activity. Note, the use of all U.S. Food and Drug Administration (FDA) approved DMARDs is supported by Cochrane reviews including low-dose steroids, hydroxychloroquine, sulfasalazine, methotrexate (with folic acid), azathioprine, leflunomide, cyclophosphamide, etanercept, adalimumab, and infliximab ( Fig. 48-1 ).
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Page 5 of 11
FIGURE 48-1 Treatment algorithm for rheumatoid arthritis (RA) in adults. * When starting methotrexate (MTX), add 1 mg of folic acid by mouth daily to decrease side effects; warn patient to avoid alcohol; and schedule laboratory studies (complete blood count, differential, platelets, aspartate aminotransaminase, albumin, creatinine) before starting, then every 2 weeks for 6 weeks, then every 2 months if normal. When adding another diseaseremitting antirheumatic drug (DMARD) to MTX, decrease the dose of MTX to 10 to 15 mg once per week. Ca, calcium; HCQ, hydroxychloroquine; IM, intramuscular; FA, fatty acid; Mg, magnesium; Se, selenium; SSZ, sulfasalazine; SQ, subcutaneous; TB, tuberculosis; vits, vitamins.
HYDROXYCHLOROQUINE AND SULFASALAZINE
Hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine-EN) each are used early in disease when a diagnosis may not be clear or there is no characteristic erosive disease. Both drugs have little short- and long-term toxicity.
Dosage
The current accepted dose of hydroxychloroquine is 200 mg twice daily, which carries little risk of toxicity; nevertheless, an ophthalmologic examination to test for retinal toxicity is recommended every 6 to 12 months. To reduce gastrointestinal intolerance, sulfasalazine is usually used in an enteric-coated form; dosing is started at 500 mg a day and raised by 1 tablet every few days until a dose of 1 gm twice daily is reached.
Precautions
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Page 6 of 11
Hydroxychloroquine when used in high doses carries a risk of retinal toxicity due to deposition of the drug into the retina. Sulfasalazine can uncommonly cause rash, hepatotoxicity, and leukopenia.
METHOTREXATE
Of all of the so-called DMARDs, methotrexate (Rheumatrex) has been shown to be tolerated for longer periods of treatment than any other drug. [31] Methotrexate is a folate antagonist and has a multitude of immunomodulatory activities, but its exact mechanism of action in RA is unknown. Doses of methotrexate for RA are usually between 5 and 25 mg given once a week. The dose is usually given orally in tablet form; however, the liquid form can be used orally and is sometimes less expensive. A common practice is to start with 7.5 mg orally once per week, although many practitioners, including myself, recommend starting higher doses such as 10 to 15 mg/week. With use of higher doses of 20 mg and more, patients are often taught to self-administer the dose subcutaneously once per week to avoid possible problems with gastrointestinal absorption. To decrease side effects, I always prescribe folic acid 1 to 2 mg to be taken each day. A decision to start methotrexate therapy or to raise or decrease the dose should be placed in the hands of a practitioner with extensive experience. Methotrexate is the standard by which all other drugs are judged, yet few patients achieve remission, and less than a majority achieve a 50% improvement on composite scores. Contraindications to use of methotrexate include preexisting hepatic, renal, or pulmonary disease; unwillingness to discontinue alcoholic beverages; and recent malignancy. There are many side effects, the most prominent being hepatitis, bone marrow suppression, pneumonitis, mouth sores, nausea, and headache. A complete blood count, platelet count, and determination of aspartate transaminase, albumin, and creatinine levels are done initially and then every 2 weeks for 6 weeks after methotrexate therapy is begun. Thereafter, monitoring can be done every 4 to 8 weeks. A baseline hepatitis screen and chest radiography are recommended. Tuberculosis skin testing is reserved for patients with strong risk factors or abnormal appearance on chest radiograph.
Other Immunosuppressive Drugs
Many other immunosuppressive drugs are used in RA. Leflunomide (Arava) is a newer drug that is similar in efficacy to methotrexate. [32] Leflunomide interferes with pyrimidine synthesis, whereas methotrexate interferes with purine synthesis. Leflunomide has fewer hepatotoxic effects and possibly little bone marrow toxicity but is much more likely to cause diarrhea. Azathioprine (Imuran) is metabolized to 6mercaptopurine and interferes with inosinic acid synthesis. It is often is substituted for methotrexate; however, its use is associated with gastrointestinal and bone marrow toxicity. Other immunosuppressive drugs less commonly used are mycophenolate mofetil (CellCept), cyclosporine (Neoral), tacrolimus (Prograf), and chlorambucil (Leukeran). Cyclophosphamide (Cytoxan) is often used to treat rheumatoid vasculitis.
Recombinant Biologics
Recent advances in the therapy of RA targets cytokines and cell surface molecules used to communicate between cells of the immune system. [2] [3] [4] Etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade) are TNF inhibitors. [33] [34] [35] Etanercept is given subcutaneously once or twice per week, adalimumab is given subcutaneously once every 2 weeks, whereas infliximab is usually given intravenously once every 2 months. These drugs are most often used with another DMARD, usually methotrexate, to reduce the development of autoantibodies. Short-term safety is very high, with little toxicity. As many as 30% of patients may show almost complete remission of symptoms with the combination of methotrexate and an anti-TNF agent. There are no data on long-term safety and efficacy. Use of these agents carries a risk of life-threatening exacerbations of severe infections, especially sepsis. Patients should temporarily discontinue the anti-TNF therapy during presumed infections and restart the therapy when the infection has resolved. All patients must be tested for latent tuberculosis using the PPD skin test before beginning therapy. These drugs also may exacerbate demyelinating disorders; therefore, they should be avoided in patients with suspected or proven multiple sclerosis or optic neuritis. An IL-1 receptor antagonist, anakinra (Kineret), is approved for the treatment of RA. It is given subcutaneously daily and also increases the risk of serious infection. Agents directed toward a cell surface molecule on Bcells (rituximal, Ritoxin), [6] and a costimulatory molecule on T cells (abatacept), [7] have been recently approved for use in RA. An additional biologic directed toward another cytokine FL-6 (tocilizumab) is nearing final testing and approval for use in RA.
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Acupuncture
Page 7 of 11
A single small controlled trial of acupuncture in RA showed decreased knee pain for an average of 1 to 3 months. [36]
Low-Level Laser Therapy
Low-level laser therapy (LLLT) uses a single wavelength laser source that likely has photochemical effects, and not thermal effects, on cells. A recent Cochrane review suggests that LLLT could be considered for short-term relief of pain and morning stiffness for RA patients, particularly since it has few side effects. [37]
Surgery
Loss of joint function and intractable pain may be indications for surgical intervention. Synovectomy can be helpful when systemic therapy and intra-articular corticosteroids are ineffective. Joint replacement can help restore function and increase independent activity. Patients with RA have an increased risk of surgical and postoperative complications. Cervical spine disease can lead to spinal instability and risk of neurologic injury. Replacement of one joint can result in increased stress on other joints during recovery and rehabilitation. Note that long-term corticosteroid use can cause fragility of vessels and connective tissue, hence, increasing the risks of surgery.
Therapies to Consider
There have not been adequate studies on the role of traditional Chinese medicine or Ayurvedic, homeopathy, or spiritual therapies in the management of RA. Patients should learn about several different modalities and then record their feelings about these modalities in a journal. They may then choose to visit a practitioner of a selected modality for a trial of the techniques. If the economic burden is not too great, further exploration of that therapeutic modality may be in order. PREVENTION PRESCRIPTION There are no proven methods of preventing RA. However, the following can be recommended: Laugh as much as possible. Watch funny movies, read funny books, get up every morning and force yourself to laugh. You'll find it is awkward at first, but it works anyway! Journal about stressful events. Make a list of 25 things for which you are grateful. Be creative. Do art, dance, play an instrument, beat a drum, write poetry or prose. Meditate; I recommend mindfulness meditation. Find meaning in life. Ask what gives you the energy to get up in the morning. Investigate your personality. [38] Try new things that you are afraid to do. If you feel stuck, find a good psychotherapist. Exercise. Combine aerobics, strength training, and stretching. Make it a time to play! Love people. Hang out with positive people, make sure they outweigh the negative people in your life. Find positive support groups. Eat well. Try a vegetarian diet. Make sure to balance your protein intake, and make sure you have an adequate vitamin intake. Eliminate coffee, smoking, and alcohol. Make high-sugar desserts a small, rare treat.
THERAPEUTIC REVIEW
Evidence is accumulating that current allopathic treatments are successful in slowing joint destruction and in decreasing the mortality associated with RA. [31] [33] [34] [35] [39] In addition, the rates of extraarticular manifestations of RA, such as Felty's syndrome and rheumatoid vasculitis, seem to be decreasing. Therefore, in any but the mildest cases of RA, an integrated approach should include the
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
so-called DMARDs, usually starting with methotrexate. Exercise
Page 8 of 11
Muscle strengthening and stretching can be invaluable for maintaining function. Physical therapy can be used initially for instruction; Tai Chi in the form of the range-of-motion dance can be helpful.
Mind-Body Techniques Meditation is highly recommended for RA patients willing to devote the daily time to looking more closely at the connection among body, mind, and spirit. Also recommended are relaxation exercises and the development of methods to cope with stress. Tai Chi and Yoga also may include a meditative component to the training. Journaling should be encouraged (see Chapter 98 , Journaling).
Removal of Exacerbating Factors Use of coffee, tobacco, and alcohol should be eliminated. With suspected intolerance to dairy products, wheat, citrus, or nuts, a trial of an elimination diet for 2 weeks with the reintroduction of the suspected food can be undertaken. (see Chapter 86 , Adverse Food Reactions and the Elimination Diet).
Nutrition A diet rich in omega-3 fatty acids is achieved by increasing intake of cold-water fish or adding flaxseed meal or flaxseed oil. Olive oil should be increased in the diet as well. An antiinflammatory diet is also recommended (see Chapter 88 , The Anti-Inflammatory Diet).
Supplements Omega-3 fatty acids are recommended; doses for supplementation are eicosapentaenoic acid 30 mg/kg/day and docosahexaenoic acid 50 mg/kg/day, along with GLA 1.4-2.8 gm/day, the equivalent of 6-11 gm of borage oil daily. Vitamin E should be taken in a dose of 800 IU daily as mixed tocopherols, and vitamin C in a dose of 250 mg bid. Selenium intake as nuts or supplements should be at least 100 g daily, not to exceed 400 g daily. Recommended intake of calcium is 1.5 gm daily; magnesium 400-750 mg daily and a vitamin D supplement of 800 IU/day are also recommended. Botanicals Start with ginger at 1 gm bid to a maximum of 4 gm daily. If no effect is seen after 6-8 weeks, turmeric 0.5-1 gm bid-tid can be tried.
Pharmaceuticals NSAIDs are used as little as possible owing to gastrointestinal toxicity. The classic NSAIDs are ibuprofen 800 mg tid and naproxen 500 mg bid. The COX-2 inhibitors decrease but do not eliminate the risk of gastrointestinal bleeding. Celecoxib dose is 200 mg bid. Most patients with RA are receiving combinations of drugs. Most patients are given methotrexate therapy unless there are contraindications or side effects.
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
Page 9 of 11
A common combination is methotrexate and hydroxychloroquine. Corticosteroids in moderately high doses with a rapid taper are often used for exacerbations. Commonly, a TNF inhibitor such as etanercept, adalimumab, or infliximab is added if methotrexate is only partially effective. Leflunomide or azathioprine is often substituted for methotrexate if there are intolerable side effects with methotrexate. Methotrexate and leflunomide can be used together with only a modest increase in risk of side effects. The DMARDs and the recombinant biologics have many varied side effects, some of which are only now being defined. The newest biologics are on the verge of FDA approval. The immunosuppressive pharmaceuticals should be used only with input from a subspecialist rheumatologist.
Acupuncture Acupuncture can be tried for any patient with RA. This modality may be less effective in patients taking corticosteroids.
Low-Level Laser Therapy LLLT can be tried with little risk of side effects.
Surgery Loss of joint function and intractable pain may be indications for surgical intervention. Synovectomy can be helpful when systemic therapy and intra-articular corticosteroids are ineffective. Joint replacement can help restore function and increase independent activity.
Caution: Studies have not been done on the possible additive effects of ginger, turmeric, vitamin E, and an NSAID for increased risk of hemorrhage. Other commonly used supplements or botanicals such as ginkgo may add further risk. Particular care must be used in patients taking other antiplatelet agents or warfarin sodium (Coumadin). In addition, the interactions of supplements and botanicals on allopathic pharmaceuticals are not fully understood. All health care professionals involved in the patient's care must be aware of all therapies being used. The addition of any new treatment should prompt increased laboratory monitoring for patients receiving immunosuppressive pharmaceuticals.
REFERENCES
1. Muller D: The molecular biology of autoimmunity. Immunol Allergy Clin North Am 1996; 16:659-682. 2. Choy E, Panayi G: Cytokine pathways and inflammation in rheumatoid arthritis. N Engl J Med 2001; 344:907-916. 3. Olsen N, Stein CM: New drugs for rheumatoid arthritis. N Engl J Med 2004; 350:2167-2179. 4. Singh R, Robinson DB, El-Gabalawy HS: Emerging biologic therapies in rheumatoid arthritis: Cell targets and cytokines. Curr Opin Rheumatol 2005; 17:274-279. 5. Choy E: Clinical experience with inhibition of interleukin-6. Rheum Dis Clin North Am 2004; 30:405-415. 6. Edwards J, Szczepanski L, Szechinski J, et al: Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med 2004; 350:2572-2581. 7. Genovese M, Becker J, Schiff M, et al: Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med 2005; 353:1114-1123. 8. Kimmel S, Berlin J, Reilly M, et al: Patients exposed to rofecoxib and celecoxib have different odds of
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
nonfatal myocardial infarction. Ann Intern Med 2005; 142:157-164.
Page 10 of 11
9. Stockl K, Cypren L, Chang E: Gastrointestinal bleeding rates among managed care patients newly started on COX-2 inhibitors or nonselective NSAIDs. J Manage Care Pharm 2005; 11:550-558. 10. Mangge H, Herman J, Schauenstein K: Diet and rheumatoid arthritis: A review. Scand J Rheumatol 1999; 28:201-209. 11. Ernst E, Chrubasik S: Phyto-anti-inflammatories: A systemic review of randomized, placebo-controlled, double-blind trials. Rheum Dis Clin North Am 2000; 26:13-27. 12. Edmonds SE, Winyard PG, Guo R, et al: Putative analgesic activity of repeated doses of vitamin E in the treatment of rheumatoid arthritis. Results of a placebo-controlled double-blind trial. Ann Rheum Dis 1997; 56:649-655. 13. Sirivastava KC, Mustafa T: Ginger (Zingiber officinale) and rheumatic disorders. Med Hypotheses 1989; 29:25-28. 14. Deodhar SD, Sethi R, Srimal RC: Preliminary studies on antirheumatic activity of curcumin (deferaloyl methane). Indian J Med Res 1980; 71:632-634. 15. Straub R, Cutolo M: Involvement of the hypothalamic-pituitary-adrenal/gonadal axis and the peripheral nervous system in rheumatoid arthritis. Arthritis Rheum 2001; 44:493-507. 16. Kirwan JR and the Arthritis and Rheumatism Council Low-Dose Glucocorticoid Study Group : The effect of glucocorticoids on joint destruction in rheumatoid arthritis. N Engl J Med 1995; 333:142-146. 17. van Everdingen A, Jacobs J, van Reesema D, Bijlsma J: Low-dose prednisone therapy for patients with early active rheumatoid arthritis: Clinical efficacy, disease-modifying properties, and side effects. Ann Intern Med 2002; 136:1-12. 18. Heliovaara M, Aho K, Knekt P, et al: Coffee consumption, rheumatoid factor, and the risk of rheumatoid arthritis. Ann Rheum Dis 2000; 59:631-635. 19. Hutchinson D, Shepstone L, Moots R, et al: Heavy cigarette smoking is strongly associated with rheumatoid arthritis (RA), particularly in patients without a family history of RA. Ann Rheum Dis 2001; 60:223-227. 20. Mikuls T, Cerhan J, Criswell L, et al: Coffee, tea, and caffeine consumption and risk of rheumatoid arthritis: Results from the Iowa Women's Health Study. Arthritis Rheum 2002; 46:83-91. 21. Huyser B, Parker J: Stress and rheumatoid arthritis: An integrated review. Arthritis Care Res 1998; 11:135-145. 22. Escalante A, Del Rincon I: How much disability in rheumatoid arthritis is explained by rheumatoid arthritis?. Arthritis Rheum 1999; 42:1712-1721. 23. Parker J, Smarr K, Angelone E, et al: Psychological factors, immunologic activation, and disease activity in rheumatoid arthritis. Arthritis Care Res 1992; 5:196-201. 24. Smyth J, Stone AA, Hurewitz A, Kaell A: Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. JAMA 1999; 281:1304-1309. 25. Kabat-Zinn J, Lipworth L, Burney R: The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985; 8:163-190. 26. Kabat-Zinn J, Wheeler W, Light T, et al: Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy. Psychosom Med 1998; 60:625-632. 27. Henderson CJ, Panush RS: Diets, nutritional supplements, and nutritional therapies in rheumatic diseases. Rheum Dis Clin North Am 1999; 25:937-968. 28. Linos A, Kaklamani VG, Kaklamani E, et al: Dietary factors in relation to rheumatoid arthritis: A role for
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
chapter 48 - Rheumatoid Arthritis from Rakel: Integrative Medicine on MD Consult
olive oil and cooked vegetables?. Am J Clin Nutr 1999; 70:1077-1082.
Page 11 of 11
29. Merlino L, Curtis J, Mikuls T, Cerhan J, et al: Vitamin D intake is inversely associated with rheumatoid arthritis: Results from the Iowa Women's Health Study. Arthritis Rheum 2004; 50:72-77. 30. Alarcon GS: Minocycline for the treatment of rheumatoid arthritis. Rheum Dis Clin North Am 1998; 24:489-499. 31. Pincus T: Assessment of long-term outcomes of rheumatoid arthritis. Rheum Dis Clin North Am 1995; 21:619-654. 32. Breedveld FC, Dayer JM: Leflunomide: Mode of action in the treatment of rheumatoid arthritis. Ann Rheum Dis 2000; 59:841-849. 33. Blumenauer B, Judd M, Cranney A, et al: Etanercept for the treatment of rheumatoid arthritis. Cochrane Musculoskeletal Group Cochrane Database Syst Rev 2005; 3: 34. Navarro-Sarabia F, Ariza-Ariza R, Hernandez-Cruz B, Villanueva I: Adalimumab for treating rheumatoid arthritis. Cochrane Musculoskeletal Group Cochrane Database Syst Rev 2005; 3: 35. Blumenauer B, Judd M, Cranney A, et al: Infliximab for the treatment of rheumatoid arthritis. Cochrane Musculoskeletal Group Cochrane Database Syst Rev 2005; 3: 36. Man SC, Baragar FD: Preliminary clinical study of acupuncture in rheumatoid arthritis. J Rheumatol 1974; 1:126-129. 37. Brosseau L, Welch V, Wells G, et al: Low-level laser therapy (classes I, II, and III) for treating rheumatoid arthritis. Cochrane Musculoskeletal Group Cochrane Database Syst Rev 2005; 3: 38. Keirsey D: Please Understand Me: II. Temperament Character Intelligence. Del Mar, CA, Prometheus Nemesis, 1998. 39. Krause D, Schleusser B, Herborn G, Rau R: Response to methotrexate treatment is associated with reduced mortality in patients with severe rheumatoid arthritis. Arthritis Rheum 2000; 43:14-21.
Copyright 2009 Elsevier Inc. All rights reserved. - www.mdconsult.com
Bookmark URL: /das/book/0/view/1494/95.html
http://0-www.mdconsult.com.millenium.itesm.mx/das/book/body/149218586-2/0/149... 11/07/2009
You might also like
- Complementary and Alternative Medicine in OncologyDocument15 pagesComplementary and Alternative Medicine in OncologydrmacorNo ratings yet
- Acupuncture For HeadachesDocument7 pagesAcupuncture For HeadachesdrmacorNo ratings yet
- MenopausiaDocument26 pagesMenopausiadrmacorNo ratings yet
- Efficacy of LLLT in OsteoarthritisDocument9 pagesEfficacy of LLLT in OsteoarthritisdrmacorNo ratings yet
- Qigong Externo Estudios en ChinaDocument13 pagesQigong Externo Estudios en Chinadrmacor100% (1)
- Dieta AntiinflamatoriaDocument16 pagesDieta AntiinflamatoriadrmacorNo ratings yet
- Cancer Integrative MedicieDocument15 pagesCancer Integrative MediciedrmacorNo ratings yet
- Therapeutic Effects of - I - Hominis Placenta - I - Injection Into An Acupuncture Point On The Inflammatory Responses in Subchondral Bone Region of Adjuvant-Induced Polyarthritic RatDocument2 pagesTherapeutic Effects of - I - Hominis Placenta - I - Injection Into An Acupuncture Point On The Inflammatory Responses in Subchondral Bone Region of Adjuvant-Induced Polyarthritic RatdrmacorNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- AndrogensDocument63 pagesAndrogensSantu Prashu0% (1)
- POPending Status ReportDocument26 pagesPOPending Status ReportronynoorNo ratings yet
- Drug Prefixes Roots SuffixesDocument4 pagesDrug Prefixes Roots SuffixesElla LopezNo ratings yet
- Obat ObatDocument8 pagesObat ObatMuhammad Aulia KurniawanNo ratings yet
- Histamine and Antihistaminic Agents: Pharmaceutical Chemistry 2Document45 pagesHistamine and Antihistaminic Agents: Pharmaceutical Chemistry 2د. أبجًملNo ratings yet
- Chapter 9 - Adrenergic AgonistsDocument4 pagesChapter 9 - Adrenergic AgonistsJoseph Campos SanchezNo ratings yet
- Remar Nurse Pharmacology Review: Brought To You by Regina M. Callion MSN, RN Creator of The NCLEX Virtual TrainerDocument50 pagesRemar Nurse Pharmacology Review: Brought To You by Regina M. Callion MSN, RN Creator of The NCLEX Virtual TrainerMonalizaSantos100% (2)
- 1 PBDocument12 pages1 PBLela MaelaNo ratings yet
- 29.4 Sleep Neurology.2023Document317 pages29.4 Sleep Neurology.2023velto anjosNo ratings yet
- Protogyl PDFDocument5 pagesProtogyl PDFpushkar078No ratings yet
- Cology Final McqsDocument33 pagesCology Final McqsSameer AliNo ratings yet
- School of Nursing & Midwifery Clinical Module 3 300NAS209 Adult Branch Numeracy TestDocument6 pagesSchool of Nursing & Midwifery Clinical Module 3 300NAS209 Adult Branch Numeracy Testnananana1230% (1)
- Test Bank For Pharmacology Clear and Simple A Guide To Drug Classifications and Dosage Calculations 3rd Edition WatkinsDocument6 pagesTest Bank For Pharmacology Clear and Simple A Guide To Drug Classifications and Dosage Calculations 3rd Edition WatkinsJean Taylor100% (39)
- Over The Counter DrugsDocument28 pagesOver The Counter DrugsManjusha KondepudiNo ratings yet
- Ostuzzi Et Al-2015-The Cochrane Library - Sup-2Document63 pagesOstuzzi Et Al-2015-The Cochrane Library - Sup-2Pepe Serrano RodríguezNo ratings yet
- Fphar 12 684162Document15 pagesFphar 12 684162ade 119260170No ratings yet
- Volume1 Eng BioavaiDocument148 pagesVolume1 Eng Bioavaihugoboss_dark100% (1)
- Bicillin C-R Penicillin G: Drug StudyDocument1 pageBicillin C-R Penicillin G: Drug StudyChristine Pialan Salimbagat100% (1)
- 1760Document11 pages1760AnggunNo ratings yet
- COVID 19 Vaccine Comparison ChartDocument2 pagesCOVID 19 Vaccine Comparison ChartNuklear AdiwenaNo ratings yet
- Pharmacology NotesDocument1 pagePharmacology NotesKlare TyNo ratings yet
- Front PageDocument11 pagesFront PageJake PaduaNo ratings yet
- Pharmacology Mnemonics (Part 01) by M IhtishamDocument32 pagesPharmacology Mnemonics (Part 01) by M Ihtishammuhammad ihtisham ul hassan100% (1)
- Drugs Producing Uterine CONTRACTIONS (Oxytocic Drugs) : Oxytocin Ergot Alkaloids ProstaglandinsDocument9 pagesDrugs Producing Uterine CONTRACTIONS (Oxytocic Drugs) : Oxytocin Ergot Alkaloids ProstaglandinsFaris Jamal Abu Za'nounehNo ratings yet
- Psycho Specific Side Effects Edit 1-1Document3 pagesPsycho Specific Side Effects Edit 1-1Jeffrey ViernesNo ratings yet
- Risk ManagmentDocument5 pagesRisk ManagmentRhodora Benipayo100% (3)
- Toxicologie Clinica 1Document29 pagesToxicologie Clinica 1Andrei Marica100% (1)
- Cough Syrup Detail:: Prodactive or Expectorant and Suppressant or Dry CoughDocument3 pagesCough Syrup Detail:: Prodactive or Expectorant and Suppressant or Dry CoughFarhadullah KhanNo ratings yet
- 1st Prelims Pharmacology Special ExamDocument5 pages1st Prelims Pharmacology Special ExamMayvonne SapaenNo ratings yet
- Monoamine Oxidase InhibitorsDocument14 pagesMonoamine Oxidase InhibitorsMary Ann DimayugaNo ratings yet