Professional Documents
Culture Documents
Branch Retinal Vein Occlusion (BRVO)
Uploaded by
Mahmoud Ahmed MahmoudOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Branch Retinal Vein Occlusion (BRVO)
Uploaded by
Mahmoud Ahmed MahmoudCopyright:
Available Formats
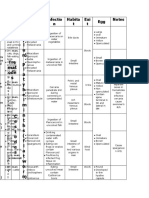
Classification
Branch retinal vein occlusion (BRVO)
CLASSIFICATION
1) Major BRVO: At the disc and/or away from the disc. 2) Macular BRVO: Involving only a macular branch. 3) Peripheral BRVO: Not involving the macular circulation.
DIAGNOSIS
Presentation:
It depends on the extent of macular circulation compromised by the occlusion. Patients with macular involvement often present with the sudden onset of blurred vision and metamorphopsia, or a relative visual field defect. Patients with peripheral occlusions may be asymptomatic.
Visual Acuity (VA):
It is very variable and is principally dependent on the extent of macular involvement.
Fundus Examination:
Dilatation and tortuosity of the affected venous segment. The site of occlusion is often identifiable as an arteriovenous crossing point. Flame-shaped and dot/blot haemorrhages, retinal edema, sometimes cotton wool spots affecting the sector of the retina drained by the obstructed vein.
Fluorescein Angiography (FA):
It shows variable delayed venous filling, blockage by blood, staining of the vessel wall, hypofluorescence due to capillary non-perfusion and pruning of vessels in the ischemic areas.
Optical coherence tomography (OCT):
It demonstrates and allows quantification of the severity of macular edema and is a useful way of monitoring its course and the response to treatment.
Branch Retinal Vein Occlusion
Prognosis
Course:
The acute features usually resolve within 612 months and may be replaced by the following: Exudates, venous sheathing and sclerosis peripheral to the site of obstruction, collaterals and variable residual haemorrhage. Collateral are characterized by slightly tortuous veins that develop locally or across the horizontal raphe between the inferior and superior vascular arcades and are best detected on FA. The severity of residual signs is highly variable and they may be only subtle.
PROGNOSIS
At 6 months about 50% of eyes achieve vision of 6/12 or better. Approximately 50% of untreated eyes with BRVO retain 6/12 or better whilst 25% will have vision of <6/60.
COMPLICATIONS:
The two main vision-threatening complications are:
Chronic macular edema:
It is the most common cause of persistent poor visual acuity after BRVO. Patients with visual acuity of 6/12 or worse may benefit from laser photocoagulation, provided the macula is not significantly ischemic.
Neovascularization:
Retinal neovascularization occurs in about 60% of eyes with more than 5 disc areas of nonperfusion and a third with less than 4 disc areas about 40% overall. NVE are considerably more common than NVD. NVE usually develops at the border of the triangular sector of ischemic retina drained by the occluded vein. New vessels usually appear within 612 months but may develop at any time; they can lead to recurrent vitreous and pre-retinal haemorrhage, and occasionally tractional retinal detachment.
Branch Retinal Vein Occlusion
Management
MANAGEMENT
Follow-up should be at about 3 months with FA: A) With good macular perfusion and improving visual acuity, no treatment is required. B) If macular edema is associated with good macular perfusion and visual acuity continues to be 6/12 or worse after 36 months, laser photocoagulation should be considered. Patients with visual acuity of less than 6/60 or those with symptoms for over a year are unlikely to benefit from laser. Prior to treatment, the FA should be studied carefully to identify leaking areas. C) If macular non-perfusion is present and visual acuity is poor, particularly if FA shows an incomplete foveal avascular zone (FAZ), laser treatment is unlikely to improve vision.
Treatment of macular edema
Grid laser photocoagulation
(50100 m, 0.1 second duration and spaced one burn width apart) to produce a gentle reaction in the area of leakage as identified on FA. The burns should extend no closer to the fovea than the edge of the FAZ and be no more peripheral than the major vascular arcades. Care should be taken to avoid treating over intraretinal haemorrhage. It is also very important to identify shunts/collaterals on FA, which do not leak fluorescein, because they must not be treated. Follow-up should take place after three months. If macular edema persists, retreatment may be considered although the results are frequently disappointing.
Intravitreal triamcinolone (IVT)
It is as effective as laser in eyes with macular edema, but may cause cataract and elevation of intraocular pressure. An average of 2 injections of 1 mg are given in the first year.
Periocular steroid injection
It is less invasive, although probably less effective, than the intravitreal route.
Intravitreal anti-VEGF agents.
Bevacizumab (Avastin) 0.05 mL/1.25 mg) in a regimen of 23 injections over 56 months has shown promising effects on macular edema and vision, including in patients resistant to laser.
Branch Retinal Vein Occlusion
Management
Arteriovenous sheathotomy.
Some positive results have been reported both for sheathotomy and for vitrectomy alone; a randomized controlled trial showed similar benefit from IVT.
Treatment of neovascularization
Neovascularization is not normally treated unless vitreous haemorrhage occurs because early treatment does not appear to affect the visual prognosis. If appropriate, scatter laser photocoagulation (200500 m size, 0.050.1 s duration and spaced one burn width apart) is performed with sufficient energy to achieve a medium reaction covering the entire involved sector as defined by the colour photograph and FA. A quadrant usually requires 400500 burns. Follow-up should be after 46 weeks. If neovascularization persists re-treatment can be considered, and is usually effective in inducing regression.
Branch Retinal Vein Occlusion
You might also like
- Clinical Ophthalmology for UndergraduatesFrom EverandClinical Ophthalmology for UndergraduatesRating: 4 out of 5 stars4/5 (5)
- Non-Ischemic Central Retinal Vein OcclusionDocument6 pagesNon-Ischemic Central Retinal Vein OcclusionMahmoud Ahmed MahmoudNo ratings yet
- Management of Macular HemorrhageFrom EverandManagement of Macular HemorrhageLars-Olof HattenbachNo ratings yet
- Vitreous Hemorrhage: Major ReviewDocument4 pagesVitreous Hemorrhage: Major Reviewmutya yulindaNo ratings yet
- Branch Retinal Vein Occlusion (BRVO) : How Does BRVO Occur?Document3 pagesBranch Retinal Vein Occlusion (BRVO) : How Does BRVO Occur?merizNo ratings yet
- Visual Field Loss in the Real World: A Book of Static Perimetry Test Targets for Eye Health ProfessionalsFrom EverandVisual Field Loss in the Real World: A Book of Static Perimetry Test Targets for Eye Health ProfessionalsNo ratings yet
- Retinal Vein Occlusion (RVO) Guideline: Executive Summary: EditorialDocument4 pagesRetinal Vein Occlusion (RVO) Guideline: Executive Summary: EditorialAna NietoNo ratings yet
- Central Retinal Vein Occlusion and Branch Retinal Vein OcclusionDocument5 pagesCentral Retinal Vein Occlusion and Branch Retinal Vein OcclusionPOPPYNo ratings yet
- BRVO PPT by Dr. Chinmay KharadeDocument31 pagesBRVO PPT by Dr. Chinmay KharadeChinmay KharadeNo ratings yet
- Retinal Vein Occlusion (RVO)Document5 pagesRetinal Vein Occlusion (RVO)Rana PandaNo ratings yet
- Central Serous RetinopathyDocument7 pagesCentral Serous RetinopathyshintasissyNo ratings yet
- Retinal DetachmentDocument21 pagesRetinal Detachmentณัช เกษมNo ratings yet
- Advances in The Treatment of Central Serous ChorioretinopathyDocument9 pagesAdvances in The Treatment of Central Serous ChorioretinopathyAlyani Akramah BasarNo ratings yet
- Laser 2Document2 pagesLaser 2kavitasugumaranNo ratings yet
- Retinal Vascular Occlusions: Moderator:Dr Madhurimanayak Presenter:Dr PoojaDocument62 pagesRetinal Vascular Occlusions: Moderator:Dr Madhurimanayak Presenter:Dr PoojaUlquiorra SchifferNo ratings yet
- Penjelasan Dan Jawaban CRVODocument4 pagesPenjelasan Dan Jawaban CRVONuruel SazaNo ratings yet
- Vitreous HemorrhageDocument7 pagesVitreous HemorrhageindahNo ratings yet
- Diabetic Retinopathy Presentations (Can Still Use The Older Classification)Document6 pagesDiabetic Retinopathy Presentations (Can Still Use The Older Classification)gdudex118811No ratings yet
- This Site Is Intended For Healthcare ProfessionalsDocument10 pagesThis Site Is Intended For Healthcare ProfessionalssudheervermaNo ratings yet
- Holy 3Document3 pagesHoly 3Holy Fitria ArianiNo ratings yet
- Retina/Vitreous: Question 1 of 130Document51 pagesRetina/Vitreous: Question 1 of 130safasayedNo ratings yet
- AAO Network OculoplasticsDocument53 pagesAAO Network OculoplasticsSafa Abdualrahaman Ali HamadNo ratings yet
- AAO MCQ Recent Web PDFDocument510 pagesAAO MCQ Recent Web PDFNoorNo ratings yet
- Note DRDocument2 pagesNote DRZuhair Al-JaffalNo ratings yet
- Retinal Detachment and HomoeopathyDocument7 pagesRetinal Detachment and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- Retinal DetachmentDocument32 pagesRetinal Detachmentc/risaaq yuusuf ColoowNo ratings yet
- Jorge G Arroyo, MD, MPH Jonathan Trobe, MD Howard Libman, MD Contributor Disclosures Peer Review ProcessDocument13 pagesJorge G Arroyo, MD, MPH Jonathan Trobe, MD Howard Libman, MD Contributor Disclosures Peer Review ProcessLis Borda MuñozNo ratings yet
- Complications Associated With Cataract SurgeryDocument24 pagesComplications Associated With Cataract SurgeryEvenjelina EveNo ratings yet
- Fact Sheet Central Retinal Vein OcclusionDocument2 pagesFact Sheet Central Retinal Vein OcclusionAini Nur Syafa'ahNo ratings yet
- Spontaneous Association of Macular Hole and Choroidal Neovascularization: A Case ReportDocument4 pagesSpontaneous Association of Macular Hole and Choroidal Neovascularization: A Case ReportIJAR JOURNALNo ratings yet
- Central Serous ChoroidopathyDocument14 pagesCentral Serous Choroidopathyapi-19916399No ratings yet
- AAO Network CorneaDocument60 pagesAAO Network CorneaLydia Angelia YanitaNo ratings yet
- FIQ - Retinal Vein OcclusionDocument31 pagesFIQ - Retinal Vein OcclusionHikban FiqhiNo ratings yet
- ManagementDocument3 pagesManagementElison J PanggaloNo ratings yet
- Retinal DetachmentDocument31 pagesRetinal DetachmentEko KunaryagiNo ratings yet
- Injeksi Intravitreal Bevacizumab Dan Laser Fotokoagulasi Pada Branch RetinalDocument8 pagesInjeksi Intravitreal Bevacizumab Dan Laser Fotokoagulasi Pada Branch RetinalDwi MasrokhahNo ratings yet
- Retinal DetachmentDocument14 pagesRetinal DetachmentPui_Yee_Siow_6303No ratings yet
- Diabetic RetinopathyDocument18 pagesDiabetic Retinopathymohelshiekh100% (3)
- Case 29.07.09Document51 pagesCase 29.07.09kanavgNo ratings yet
- MyopiaDocument11 pagesMyopiablueiceNo ratings yet
- 12 Kasper Notes 2020 OphthalmologyDocument33 pages12 Kasper Notes 2020 OphthalmologyMohamed Rikarz Ahamed RikarzNo ratings yet
- Yag Laser CapsulotomyDocument5 pagesYag Laser CapsulotomyinhaNo ratings yet
- Retinal Vascular DisordersDocument52 pagesRetinal Vascular Disorderssushma shresthaNo ratings yet
- Acquired Peripheral RetinoschisisDocument6 pagesAcquired Peripheral RetinoschisisSebaNo ratings yet
- Diabetic RetinopathyDocument5 pagesDiabetic RetinopathyJayvee CornelioNo ratings yet
- Refractive Management v1m1Document30 pagesRefractive Management v1m1Faisal AwaluddinNo ratings yet
- L5 AMD & DR LectureDocument44 pagesL5 AMD & DR LectureSofíaGriggsNo ratings yet
- 60 FTPDocument5 pages60 FTPCarlo RiveliNo ratings yet
- Retinal DetachmentDocument8 pagesRetinal DetachmentJohanLazuardiNo ratings yet
- Retinal DiseasesDocument22 pagesRetinal Diseasesz7gcdfbctfNo ratings yet
- RvoDocument43 pagesRvoOrchlon LkNo ratings yet
- Results of Staged Combined Laser Treatment of Neovascular GlaucomaDocument4 pagesResults of Staged Combined Laser Treatment of Neovascular GlaucomaCentral Asian StudiesNo ratings yet
- EURETINA. Management of - Retinal Vein Occlusion.Document40 pagesEURETINA. Management of - Retinal Vein Occlusion.Javier Infantes MolinaNo ratings yet
- Optical Coherence Tomography in Branch Retinal Vein Occlusion at Tertiary Care Center-A Cross Sectional StudyDocument7 pagesOptical Coherence Tomography in Branch Retinal Vein Occlusion at Tertiary Care Center-A Cross Sectional StudyMurali Krishna DNo ratings yet
- Ectasia Corneal y Cirugía RefractivaDocument13 pagesEctasia Corneal y Cirugía RefractivapachisfmbNo ratings yet
- Glaucoma OverviewDocument33 pagesGlaucoma Overviewc/risaaq yuusuf ColoowNo ratings yet
- Principles of Vitreoretinal Surgery - Scleral Buckle: Dr. Sumit Kumar MishraDocument49 pagesPrinciples of Vitreoretinal Surgery - Scleral Buckle: Dr. Sumit Kumar MishraSriniwasNo ratings yet
- Anti-VEGF Treatment Is The Key Strategy For Neovascular Glaucoma Management in The Short TermDocument8 pagesAnti-VEGF Treatment Is The Key Strategy For Neovascular Glaucoma Management in The Short TermhellowNo ratings yet
- Pemicu 1 Pengindraan c2Document113 pagesPemicu 1 Pengindraan c2CcNo ratings yet
- Anti-Microbial Therapy Final With AlarmsDocument245 pagesAnti-Microbial Therapy Final With AlarmsMahmoud Ahmed MahmoudNo ratings yet
- Fetal Malnutrition: DR. Mahmoud Ahmed Mahmoud Ahmed Faculty of Medicine Alexandria UniversityDocument11 pagesFetal Malnutrition: DR. Mahmoud Ahmed Mahmoud Ahmed Faculty of Medicine Alexandria UniversityMahmoud Ahmed MahmoudNo ratings yet
- Investigative HepatologyDocument24 pagesInvestigative HepatologyMahmoud Ahmed MahmoudNo ratings yet
- Fetal MalnutritionDocument2 pagesFetal MalnutritionMahmoud Ahmed MahmoudNo ratings yet
- Ovarian Hyperstimulation SyndromeDocument3 pagesOvarian Hyperstimulation SyndromeMahmoud Ahmed MahmoudNo ratings yet
- Non-Ischemic Central Retinal Vein OcclusionDocument17 pagesNon-Ischemic Central Retinal Vein OcclusionMahmoud Ahmed MahmoudNo ratings yet
- Investigative HepatologyDocument6 pagesInvestigative HepatologyMahmoud Ahmed MahmoudNo ratings yet
- Livor MortisDocument5 pagesLivor MortisMahmoud Ahmed MahmoudNo ratings yet
- Drug Management of AgitationDocument14 pagesDrug Management of AgitationMahmoud Ahmed MahmoudNo ratings yet
- Livor MortisDocument16 pagesLivor MortisMahmoud Ahmed MahmoudNo ratings yet
- Diphtheria VaccineDocument5 pagesDiphtheria VaccineMahmoud Ahmed MahmoudNo ratings yet
- Management of AgitationDocument8 pagesManagement of AgitationMahmoud Ahmed MahmoudNo ratings yet
- Iphtheria Accine Oxoid: Mahmoud Ahmed Mahmoud 846Document23 pagesIphtheria Accine Oxoid: Mahmoud Ahmed Mahmoud 846Mahmoud Ahmed MahmoudNo ratings yet
- Phylum Platyhelminths (Flat Worms)Document2 pagesPhylum Platyhelminths (Flat Worms)Mahmoud Ahmed MahmoudNo ratings yet
- Endoscopic Surgery For Cancer LarynxDocument11 pagesEndoscopic Surgery For Cancer LarynxMahmoud Ahmed MahmoudNo ratings yet
- Endoscopic Surgery For Cancer LarynxDocument13 pagesEndoscopic Surgery For Cancer LarynxMahmoud Ahmed MahmoudNo ratings yet
- A-Autonomic Drugs: 1) CholinergicDocument28 pagesA-Autonomic Drugs: 1) CholinergicMahmoud Ahmed MahmoudNo ratings yet
- Adi Setya Frida Utami - FIKES PDFDocument108 pagesAdi Setya Frida Utami - FIKES PDFZyy VyeNo ratings yet
- Listening ComprehensionDocument5 pagesListening ComprehensionLaura michell Núñez SuarezNo ratings yet
- Company Briefing: - Ritika Rastogi - Reg - No. 35-1967Document7 pagesCompany Briefing: - Ritika Rastogi - Reg - No. 35-1967Ritika RastogiNo ratings yet
- Abnormal Lie: - Abnormal Lie Consists of Two Types: Transverse Lie Oblique LieDocument21 pagesAbnormal Lie: - Abnormal Lie Consists of Two Types: Transverse Lie Oblique LieBharat ThapaNo ratings yet
- COVID-19: Vaccine Management SolutionDocument7 pagesCOVID-19: Vaccine Management Solutionhussein99No ratings yet
- Dapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument18 pagesDapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsVictoria Maya ChyntiaNo ratings yet
- Malaria Case AnalysisDocument1 pageMalaria Case AnalysisANGELA MARIE VILLENANo ratings yet
- Level 2 Unit 39 Assist in The Administration of MedicationDocument7 pagesLevel 2 Unit 39 Assist in The Administration of MedicationSzabolcs LehotaNo ratings yet
- Wiri 08 - Zambia Trip Application FormDocument11 pagesWiri 08 - Zambia Trip Application Forminfo@zcfcanada.orgNo ratings yet
- Time Management StrategiesDocument3 pagesTime Management Strategiesأحمد عبدالمحسنNo ratings yet
- Article in Press: Age-Related Hair Changes in Men: Mechanisms and Management of Alopecia and GrayingDocument5 pagesArticle in Press: Age-Related Hair Changes in Men: Mechanisms and Management of Alopecia and Grayingpasid harlisaNo ratings yet
- Pinnacle Tecnica Quirurgica 2Document49 pagesPinnacle Tecnica Quirurgica 2Saenz Guzman LauraNo ratings yet
- Ujian Akhir SekolahDocument7 pagesUjian Akhir SekolahAhmad andis ArifinNo ratings yet
- To The Philosophy of The Human Person: Quarter 1 - Module 4.2: Care For The EnvironmentDocument21 pagesTo The Philosophy of The Human Person: Quarter 1 - Module 4.2: Care For The EnvironmentDustin EsguerraNo ratings yet
- Ulvac Ulvoil r7Document5 pagesUlvac Ulvoil r7Hiskia Benindo PurbaNo ratings yet
- PE and Health 11Document67 pagesPE and Health 11Janafaye Krisha100% (1)
- FAQ Mid Day MealsDocument7 pagesFAQ Mid Day Mealsvikramhegde87No ratings yet
- Can Celebrities Be Good Role Models For UsDocument2 pagesCan Celebrities Be Good Role Models For UsSamira MusayevaNo ratings yet
- SSB201 Group Assigment 1 - Design ThinkingDocument3 pagesSSB201 Group Assigment 1 - Design ThinkingLe CuongNo ratings yet
- Professional AdvancementDocument51 pagesProfessional AdvancementReshma AnilkumarNo ratings yet
- Washington D.C. Afro-American Newspaper, July 24, 2010Document20 pagesWashington D.C. Afro-American Newspaper, July 24, 2010The AFRO-American NewspapersNo ratings yet
- Villa La Paws Operations Manual-Detail 03-26-2014Document167 pagesVilla La Paws Operations Manual-Detail 03-26-2014Anonymous JKqvy986U100% (1)
- Revised BizTown PPDocument16 pagesRevised BizTown PPRene BrathwaiteNo ratings yet
- Farfalle With Creamy Bacon Sauce - Spend With PenniesDocument2 pagesFarfalle With Creamy Bacon Sauce - Spend With PenniesrectagleNo ratings yet
- Gn-31 Qms Cad (Dec 2012) FinalDocument19 pagesGn-31 Qms Cad (Dec 2012) FinalSeanNo ratings yet
- Study Plan FinalDocument5 pagesStudy Plan FinalMd IslamNo ratings yet
- Pathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun MengDocument20 pagesPathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun Mengbanteng wibisonoNo ratings yet
- Blood Component PreparationDocument24 pagesBlood Component PreparationLaiba ArshadNo ratings yet
- 017-2013 - MR (MOA Kalahi Cidss)Document3 pages017-2013 - MR (MOA Kalahi Cidss)SbGuinobatanNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (26)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)