Professional Documents
Culture Documents
Cutaneous Cysticercosis
Uploaded by
Deba P SarmaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cutaneous Cysticercosis
Uploaded by
Deba P SarmaCopyright:
Available Formats
Biopsy of a 1.
5-cm cystic lesion on the right cheek of a 28-year-old man
Deba P Sarma, MD Omaha
The patient is a 28-year-old male from Burma, who has been living in the United States for one year. He presented with a 1.5 cm tender non-erythematous subcutaneous nodule on the right cheek. The lesion is slightly mobile and has been present for the past three years. The patient states that the lesion has gotten progressively larger over the past three years. No other lesions were identified elsewhere on his body. The clinical impression was a cystic lesion with concern for a parasitic infection versus a sebaceous cyst. A local excision of the lesion was performed.
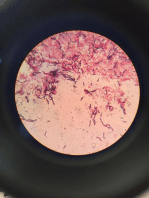
Diagnosis: Cutaneous cysticercosis Comment: Abstract: Biopsy of a subcutaneous cyst of the cheek from a 28-year-old man revealed cysticercosis. Such lesions primarily present as multiple, mobile, 1-2 cm nodules in the subcutaneous tissue. They may be painless or mildly tender. The overlying epidermal skin surface is usually normal and the nodular lesions are often clustered. Most commonly, they are seen on the trunk, upper extremities, and face. Definitive diagnosis of subcutaneous cysticercosis requires an excisional biopsy, which demonstrates the cysticercus. For uncomplicated subcutaneous nodules, treatment requires surgical excision. The primary significance of subcutaneous cysticercosis is that it may indicate involvement of the central nervous system (neurocysticercosis) that may need systemic anti-parasitic therapy. Discussion: Cysticercosis affects approximately 50 million people worldwide, and is endemic in Mexico and South America, sub-Saharan Africa, India, and East Asia. Approximately 1,000 new cases of cysticercosis are reported annually in the United States. It is a systemic illness due to dissemination of the larval form (Cysticercus cellulosae) of the pork tapeworm, Taenia solium [3]. The clinical
syndromes caused by Taenia solium are categorized as either neurocysticercosis (NCC) or extra-neural cysticercosis. The most frequently reported locations are skin, skeletal muscle, heart, eye, and the central nervous system (CNS). Subcutaneous cysticercosis primarily presents as multiple freely mobile nodules. These nodules are 12 cm in size and are deep-seated in the subcutaneous tissue [6]. They may be painless or mildly tender. The overlying skin surface is usually normal and the nodular lesions are often clustered [6]. Most commonly, they are seen on the trunk, upper extremities, and face. Gross examination findings for subcutaneous cysticercosis may reveal a solitary cystic lesion with white-colored, solid nodules that are adhered to the cyst wall. The differential diagnosis for subcutaneous cysticercosis includes: lipoma, neurofibroma, epidermoid cyst, sarcoidosis, scrofula, ganglion cyst, metastatic carcinoma, and lymphadenopathy. Definitive diagnosis of subcutaneous cysticercosis requires histological examination of the biopsy sample showing the cystericercus, that appears as an undulating laminated membranous wall of a cysticercus (the larvae of a tapeworm), with associated marked inflammatory reaction. The cyst is composed of a thick integument and an outer surface covered with microvilli. The tegumental cells may display degenerative changes in the inner layer of the cyst wall. The scolex may or may not be found in the specimen. Additionally, stool examination for ova and parasites should be performed to assess for a concomitant intestinal parasite infection. The primary significance of subcutaneous cysticercosis is that is a possible indicator of neurocysticercosis. In order to assess the involvement of the CNS, a CT scan of the head (with and without contrast) should be done on all patients suspected with neurocysticercosis or confirmed cysticercosis at another body location. Cases of neurocysticercosis will demonstrate multiple calcified cysts in the brain parenchyma on CT scan. The serious pathologic findings of neurocysticercosis include: seizures, encephalopathy, obstructive hydrocephalus, meningoencephalitis, and vascular accidents [2]. Clinical expression of NCC depends primarily on the number and location of CNS cysticerci and degree of the host immune response and resultant peri-cystic inflammation [5]. The ingestion of encysted pork does not directly cause cysticercosis. Rather, it produces an intestinal infection of the adult T. solium tapeworm and man becomes a carrier for the T. solium eggs. T. solium worms may reach a length of several meters. The morphology of a T. solium adult worm consists of a scolex with four suckers, and a double crown of prominent hooks. When the adult tapeworm reaches the small intestine, the scolex attaches to the intestinal mucosa and a proglottid chain grows. The adult tapeworm releases three to six proglottids per day, which bear 30,000 to 70,000 eggs per proglottid into the small intestine [4]. Nearly 250,000 eggs are passed daily into the human feces and
to the environment [4]. Infections with cysticercus larva occur after humans consume eggcontaminated food/water or through self-infection via the fecal-oral route [1]. Treatment depends on the location, number of cysts, and the patients clinical presentation. For uncomplicated subcutaneous nodules, surgical excision is sufficient. However, for symptomatic neurocysticercosis, anti-parasitic therapy (albendazole or praziquantel) should be given in combination with corticosteroids and anticonvulsants to reduce the inflammation surrounding the cysts and lower the risk of seizures [5]. Asymptomatic cysts may never lead to symptomatic disease and in many cases do not require therapy [5]. Education of person hygiene practices and proper food handling techniques should be performed. In our case, the patient was referred to an infectious disease specialist for further work-up; however the patient did not return for follow-up care and could not be reached. References:
1) Cysticercosis. http://www.dpd.cdc.gov/dpdx/HTML/cysticercosis.htm. 2) DeGiorgio CM, Medina MT, Durn R, Zee C, Escueta SP. Neurocysticercosis. Epilepsy Curr. 2004 MayJun; 4(3):107-11. PubMed PMID: 16059465.
3) Garca HH, Gonzalez AE, Evans CA, Gilman RH; Cysticercosis Working Group in Peru. Taenia solium cysticercosis. Lancet. 2003 Aug 16; 362(9383):547-56. PubMed PMID: 12932389.
4) Davis, LE. Neurocysticercosis Emerging Neurological Infections edited by Power, C and Johnson RT. Taylor & Francis Group, 2005. pp 261-287.
5) Riley T, White AC Jr. Management of neurocysticercosis. CNS Drugs.2003; 17(8):577-91. PubMed PMID: 12775194.
6) Uthida-Tanaka AM, Sampaio MC, Velho PE, Damasceno BP, Cintra ML, de Moraes AM, Zanardi V. Subcutaneous and cerebral cysticercosis. J Am Acad Dermatol. 2004 Feb;50(2 Suppl):S14-7. PubMed PMID: 14726858.
You might also like
- B R Robbins and Cotran: Pathologic Basis of Disease, 8th EditionDocument1 pageB R Robbins and Cotran: Pathologic Basis of Disease, 8th EditionabdallhNo ratings yet
- CellulitisDocument39 pagesCellulitisMary Jhane Villanueva50% (4)
- Toxicology ReportDocument2 pagesToxicology Reportapi-457390058No ratings yet
- Med Surg QuizDocument91 pagesMed Surg QuizCharles Gerard B. Beluan0% (1)
- Major Internship DTR JulyandaugustDocument1 pageMajor Internship DTR JulyandaugustGeraldineMoletaGabutin100% (1)
- Cysticercosis - Clinical Manifestations and Diagnosis - UpToDateDocument26 pagesCysticercosis - Clinical Manifestations and Diagnosis - UpToDateAndréia GomesNo ratings yet
- Group 8 Parasitic CystsDocument47 pagesGroup 8 Parasitic CystsMariam Abd ElhadiNo ratings yet
- Neurocysticercosis. A Frequent Cause of Seizures, Epilepsy, and OtherDocument12 pagesNeurocysticercosis. A Frequent Cause of Seizures, Epilepsy, and OtherMaria Lucero Jinés TapiaNo ratings yet
- Oral Cysticercosis: Case Report and Review of The LiteratureDocument4 pagesOral Cysticercosis: Case Report and Review of The LiteraturePeiterGozaliNo ratings yet
- Echinococcosis 1Document38 pagesEchinococcosis 1Nadine SellersNo ratings yet
- Taenia SoliumDocument2 pagesTaenia SoliumGlazy Kim SecoNo ratings yet
- Pathogens 11 01212Document13 pagesPathogens 11 01212Bapa akuNo ratings yet
- Neurocisticercosis: Neurología - InfectologíaDocument7 pagesNeurocisticercosis: Neurología - Infectologíasanti gamer mNo ratings yet
- Neurocisticercosis PDFDocument7 pagesNeurocisticercosis PDFFiorella Alexandra HRNo ratings yet
- Mehu131 U1 T6 NeurocysticercosisDocument16 pagesMehu131 U1 T6 NeurocysticercosisGabriel OlivaresNo ratings yet
- Soft Tissue Infections English 3-Rd 2016Document39 pagesSoft Tissue Infections English 3-Rd 2016Stefi GrNo ratings yet
- CellulitisDocument5 pagesCellulitisaimigdragonNo ratings yet
- Rapidly Enlarging Axillary Cystic Hygroma in A 6-YDocument4 pagesRapidly Enlarging Axillary Cystic Hygroma in A 6-YmohammedNo ratings yet
- A Paracanalicular AbscessDocument3 pagesA Paracanalicular AbscessolipiaNo ratings yet
- Cystic HygromaDocument5 pagesCystic HygromaAde Triansyah EmsilNo ratings yet
- Cysticercosis Causes SeizuresDocument13 pagesCysticercosis Causes SeizuresGautam JoshNo ratings yet
- Dacryocystitis: Continuing Education ActivityDocument8 pagesDacryocystitis: Continuing Education Activityerna utamiNo ratings yet
- Kista Pada LeherDocument4 pagesKista Pada LeherKhairuman FitrahNo ratings yet
- December 2013 What Is Necrotizing Fasciitis? What Are Its Causes? How Will You Manage Such A Case?Document3 pagesDecember 2013 What Is Necrotizing Fasciitis? What Are Its Causes? How Will You Manage Such A Case?Vaibhav BharatNo ratings yet
- Diagnostic Imaging in Neurocysticercosis: Costantino SA, Capiel CA, Rossini SA, Landi M, Bouzas CADocument12 pagesDiagnostic Imaging in Neurocysticercosis: Costantino SA, Capiel CA, Rossini SA, Landi M, Bouzas CAMG LilliNo ratings yet
- Orbital Cellulitis: Causes, Symptoms and TreatmentDocument42 pagesOrbital Cellulitis: Causes, Symptoms and Treatmentmuhammad iqbalNo ratings yet
- Solitary Intramuscular Cysticercosis of Right Elbow RegionDocument7 pagesSolitary Intramuscular Cysticercosis of Right Elbow RegionIJAR JOURNALNo ratings yet
- Outcome of The Treatment of Hydatid Disease in Children Over A Period of 8 YearsDocument8 pagesOutcome of The Treatment of Hydatid Disease in Children Over A Period of 8 YearsSabrina JonesNo ratings yet
- OsteomyelitisDocument32 pagesOsteomyelitisAndi Wija Indrawan PangerangNo ratings yet
- Incision and Drainage of Scrotal AbscessDocument31 pagesIncision and Drainage of Scrotal AbscessRm LavariasNo ratings yet
- PR Dr. AriadneDocument8 pagesPR Dr. AriadneSofia KusumadewiNo ratings yet
- CYSTISERCOSISDocument15 pagesCYSTISERCOSIShelda dwianaNo ratings yet
- Brain AbscessDocument17 pagesBrain AbscessLaura Fernanda Soto BNo ratings yet
- 2006 Gosche Vick SemPedSurgeryDocument8 pages2006 Gosche Vick SemPedSurgeryResya I. NoerNo ratings yet
- The History Holds The Key in This Gardener With A Skin InfectionDocument4 pagesThe History Holds The Key in This Gardener With A Skin InfectionPercy Ureta SierraNo ratings yet
- Cellulitis: Clinical PracticeDocument9 pagesCellulitis: Clinical PracticeBobby S PromondoNo ratings yet
- Cellulitis Definition, Etiology, and Clinical FeaturesDocument10 pagesCellulitis Definition, Etiology, and Clinical Featuresrosscharles1006869No ratings yet
- Neck Mass ProtocolDocument8 pagesNeck Mass ProtocolCharlene FernándezNo ratings yet
- Neck Masses and Lesions in PediatricsDocument63 pagesNeck Masses and Lesions in PediatricsRanj B. AshrafNo ratings yet
- Celulitis PDFDocument9 pagesCelulitis PDFGazade GarciaNo ratings yet
- Thyroglossal CystsDocument4 pagesThyroglossal CystsCondurache Ilie-AndreiNo ratings yet
- Arthritis: Frequency United StatesDocument7 pagesArthritis: Frequency United StateskamilahfernandezNo ratings yet
- Review of Aetiology and Management of Testicular Abscess and Case Reports On Testicle Sparing Management of Testicular AbscessDocument5 pagesReview of Aetiology and Management of Testicular Abscess and Case Reports On Testicle Sparing Management of Testicular AbscessBodat BodatsNo ratings yet
- Osteomyelitis: Hendy Buana VijayaDocument18 pagesOsteomyelitis: Hendy Buana VijayadrhendyjuniorNo ratings yet
- Makalah SelulitisDocument26 pagesMakalah Selulitisdr WiyogoNo ratings yet
- Cystic ThyroidDocument4 pagesCystic ThyroidabhishekbmcNo ratings yet
- Necrotizing SialometaplasiaDocument33 pagesNecrotizing SialometaplasiaJessica GreenNo ratings yet
- Strategies For The Elimination of Taeniasis/cysticercosis: A, B, C, E, B, D, e F B, E, G B, H B B A, B, eDocument5 pagesStrategies For The Elimination of Taeniasis/cysticercosis: A, B, C, E, B, D, e F B, E, G B, H B B A, B, eSandraOsorioOrellanaNo ratings yet
- MolluscumDocument11 pagesMolluscumAstari Pratiwi NuhrintamaNo ratings yet
- Haematogenous OsteomyelitisDocument6 pagesHaematogenous OsteomyelitisbilafarNo ratings yet
- Jurnal 3 MoluskumDocument2 pagesJurnal 3 MoluskumFausiah Ulva MNo ratings yet
- Title: Latent Primary Papillary Micro Tumor in Thyroglossal Duct Cyst Wall - A Rare Case Report With Review of LiteratureDocument9 pagesTitle: Latent Primary Papillary Micro Tumor in Thyroglossal Duct Cyst Wall - A Rare Case Report With Review of LiteratureRathinaKumarNo ratings yet
- Brain Abscess PDFDocument28 pagesBrain Abscess PDFdoctordilafrozaNo ratings yet
- 1 Septic Arthritis: Sydney NadeDocument18 pages1 Septic Arthritis: Sydney NadeLeonardo BarrosoNo ratings yet
- Imaging Findings of Intraventricular and Ependymal LesionsDocument16 pagesImaging Findings of Intraventricular and Ependymal Lesionsanggi abNo ratings yet
- Radiology Case Report - Splenic AbscessDocument6 pagesRadiology Case Report - Splenic AbscessAbeebNo ratings yet
- 1.1 BackgroundDocument13 pages1.1 BackgroundmayawjyNo ratings yet
- Case Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureDocument6 pagesCase Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureIrsalinaHusnaAzwirNo ratings yet
- Cryptococcosis - WikipediaDocument35 pagesCryptococcosis - Wikipedianoveva cenoNo ratings yet
- 8 Pseudocyst of Pinna and Its Treatment With Surgical Deroofing - An Experience at Tertiary Hospitals 2013Document13 pages8 Pseudocyst of Pinna and Its Treatment With Surgical Deroofing - An Experience at Tertiary Hospitals 2013solikin ikinNo ratings yet
- Fast Facts: Advanced Cutaneous Squamous Cell Carcinoma for Patients and their Supporters: Information + Taking Control = Best OutcomeFrom EverandFast Facts: Advanced Cutaneous Squamous Cell Carcinoma for Patients and their Supporters: Information + Taking Control = Best OutcomeNo ratings yet
- Acantholytic Acanthoma. M 60, ScrotumDocument8 pagesAcantholytic Acanthoma. M 60, ScrotumDeba P SarmaNo ratings yet
- Acantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDocument5 pagesAcantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDeba P SarmaNo ratings yet
- Acantholytic Solar Keratosis, M 67, Forehead PDFDocument6 pagesAcantholytic Solar Keratosis, M 67, Forehead PDFDeba P SarmaNo ratings yet
- Acantholytic Bullous Disease (Darier's Disease, Keratosis Follicularis)Document3 pagesAcantholytic Bullous Disease (Darier's Disease, Keratosis Follicularis)Deba P SarmaNo ratings yet
- Deba P Sarma, MD Publications 1974 To 2010 DSDocument12 pagesDeba P Sarma, MD Publications 1974 To 2010 DSDeba P SarmaNo ratings yet
- Acantholytic Actinic Keratosis, M 67, ForeheadDocument6 pagesAcantholytic Actinic Keratosis, M 67, ForeheadDeba P SarmaNo ratings yet
- Accessory TragusDocument3 pagesAccessory TragusDeba P SarmaNo ratings yet
- Pilar Cyst With Crystals. Deba P Sarma, MDDocument2 pagesPilar Cyst With Crystals. Deba P Sarma, MDDeba P SarmaNo ratings yet
- Pilar Cyst With CrystalsDocument2 pagesPilar Cyst With CrystalsDeba P SarmaNo ratings yet
- Accessory Tragus, M, 1 MonthDocument3 pagesAccessory Tragus, M, 1 MonthDeba P SarmaNo ratings yet
- Acantholytic Bullous DiseaseDocument4 pagesAcantholytic Bullous DiseaseDeba P SarmaNo ratings yet
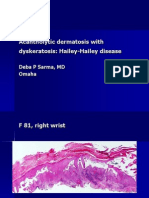
- Acantholytic Dermatosis With DyskeratosisDocument11 pagesAcantholytic Dermatosis With DyskeratosisDeba P SarmaNo ratings yet
- Acantholytic Acanthoma. M 60, ScrotumDocument8 pagesAcantholytic Acanthoma. M 60, ScrotumDeba P SarmaNo ratings yet
- Acantholytic Actinic KeratosisDocument4 pagesAcantholytic Actinic KeratosisDeba P SarmaNo ratings yet
- Deba P Sarma's Publication With Bryan Teruya, Creighton University Medical School, 2006-2012Document1 pageDeba P Sarma's Publication With Bryan Teruya, Creighton University Medical School, 2006-2012Deba P SarmaNo ratings yet
- Publications of Deba P Sarma With The Pathology Residents and Medical Students, CUMC 2006-12Document14 pagesPublications of Deba P Sarma With The Pathology Residents and Medical Students, CUMC 2006-12Deba P SarmaNo ratings yet
- DR Sarma's Melanoma Template 2013Document1 pageDR Sarma's Melanoma Template 2013Deba P SarmaNo ratings yet
- Acantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDocument5 pagesAcantholytic Acanthoma (Epidermolytic Acanthoma), M 65, NeckDeba P SarmaNo ratings yet
- Deba P Sarma's Dermatology Publications1975-2012Document8 pagesDeba P Sarma's Dermatology Publications1975-2012Deba P SarmaNo ratings yet
- Results of Search in Google Scholar On 'Deba P Sarma'Document28 pagesResults of Search in Google Scholar On 'Deba P Sarma'Deba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument6 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Balanitis Circumscripta Plasmacellularis (Zoon's Balanitis, Plasma Cell Balanitis)Document6 pagesBalanitis Circumscripta Plasmacellularis (Zoon's Balanitis, Plasma Cell Balanitis)Deba P SarmaNo ratings yet
- Xanthogranuloma, M 30, Right ElbowDocument4 pagesXanthogranuloma, M 30, Right ElbowDeba P SarmaNo ratings yet
- Xanthomatous Synovial Cyst (Xanthomatous Ganglion Cyst), M 74, Left PalmDocument7 pagesXanthomatous Synovial Cyst (Xanthomatous Ganglion Cyst), M 74, Left PalmDeba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument4 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Xanthogranuloma CasesDocument38 pagesXanthogranuloma CasesDeba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument9 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- Xanthogranuloma: Deba P Sarma, MD OmahaDocument7 pagesXanthogranuloma: Deba P Sarma, MD OmahaDeba P SarmaNo ratings yet
- XanthogranulomaDocument9 pagesXanthogranulomaDeba P SarmaNo ratings yet
- Xanthogranuloma PPT DSDocument9 pagesXanthogranuloma PPT DSDeba P SarmaNo ratings yet
- Homeopathic Remedy Pictures Alexander Gothe Julia Drinnenberg.04000 1Document6 pagesHomeopathic Remedy Pictures Alexander Gothe Julia Drinnenberg.04000 1BhargavaNo ratings yet
- RSVDocument8 pagesRSVilyas9558No ratings yet
- Olimpiada Engleza 2017 CL A 8A PDFDocument4 pagesOlimpiada Engleza 2017 CL A 8A PDFAnthony AdamsNo ratings yet
- RespiratoryDocument4 pagesRespiratoryDara Krishna Bantugan100% (1)
- SeqdumpDocument7 pagesSeqdumpAnayantzin AyalaNo ratings yet
- Libro de InmunohematologiaDocument44 pagesLibro de InmunohematologiaMijael Edgar Guadalupe MagnoNo ratings yet
- DigoxinDocument4 pagesDigoxinapi-379794167% (3)
- Chapter 9: Opinions On Professional Self-RegulationDocument27 pagesChapter 9: Opinions On Professional Self-RegulationSISIRA MOHANNo ratings yet
- Sepsis Pathophysiology Cheat Sheet 2 September 13 2018 Fall 2018 PDFDocument2 pagesSepsis Pathophysiology Cheat Sheet 2 September 13 2018 Fall 2018 PDFsophia onuNo ratings yet
- RLE Manual EditedDocument68 pagesRLE Manual EditedReymondNo ratings yet
- Manajemen Pre-Operatif Pasien Dengan DMDocument12 pagesManajemen Pre-Operatif Pasien Dengan DMyanayas28No ratings yet
- Hipocrates - VOLUME 1Document452 pagesHipocrates - VOLUME 1Heitor Murillo CarnioNo ratings yet
- Centenarian Gut Microbiota Effects On Bile AcidDocument32 pagesCentenarian Gut Microbiota Effects On Bile Acidjl18904lamNo ratings yet
- Jurnal InsomniaDocument9 pagesJurnal InsomniaMarie Obrien100% (1)
- 17 Ways To Beat Erectile DysfunctionDocument21 pages17 Ways To Beat Erectile Dysfunctionrlscott50% (2)
- Mis NotesDocument12 pagesMis NotesVasundharaNo ratings yet
- BPHS - 2010 - Final - Master Signed - PDF LatestDocument90 pagesBPHS - 2010 - Final - Master Signed - PDF LatestZakia RafiqNo ratings yet
- PFR Standardsمعايير حقوق المرضى سباهي مترجمة pdfDocument15 pagesPFR Standardsمعايير حقوق المرضى سباهي مترجمة pdfMohammed YounisNo ratings yet
- Henrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILDocument13 pagesHenrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILRoz IasilloNo ratings yet
- Medicine of The Future Digital Technologies in HeaDocument10 pagesMedicine of The Future Digital Technologies in Heaeva kacanjaNo ratings yet
- Expanding Options: For Hemodynamic MonitoringDocument2 pagesExpanding Options: For Hemodynamic MonitoringDr.Jihan HammadNo ratings yet
- Sexual Health After MenopauseDocument98 pagesSexual Health After MenopauseWirelessWomanNo ratings yet
- Komplikasi Persalinan Kala IIIDocument27 pagesKomplikasi Persalinan Kala IIIfebryana wulandariNo ratings yet
- Excerpt From "Diabetes: A Lifetime of Being Too Sweet"Document9 pagesExcerpt From "Diabetes: A Lifetime of Being Too Sweet"waltcrockerNo ratings yet
- VBAC Guide: Risks, Benefits & ManagementDocument12 pagesVBAC Guide: Risks, Benefits & Managementnyangara50% (2)
- NCP Risk For Impaired Skin Integrity Related To Ongoing Phototherapy Secondary To Increased Bilirubin LevelsDocument2 pagesNCP Risk For Impaired Skin Integrity Related To Ongoing Phototherapy Secondary To Increased Bilirubin LevelsIrish Bantolo100% (1)