Professional Documents
Culture Documents
Ineffective Airway Clearance
Uploaded by
Hanya Bint PotawanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ineffective Airway Clearance
Uploaded by
Hanya Bint PotawanCopyright:
Available Formats
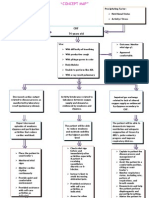
Problem Identified: Ineffective airway clearance Nursing Diagnoses: Ineffective Airway Clearance r/t bronchospasm, increased secretion production
and decreased energy. Cause Analysis: In COPD, smoke or other environmental pollutants irritate the airways, resulting in hypersecretion of mucus and inflammation. This constant irritation causes the mucus-secreting glands and goblet cells to increase in number, ciliary function is reduced, and more mucus is produced. The bronchial walls become thickened, the bronchial lumen is narrowed, and mucus may plug the airway. Fatigue, exhaustion, malaise eventually occurs and the patients ability to expectorate secretions is affected. (Brunner and Suddarth. MedicalSurgical Nursing, 10 ed, p 569-570).
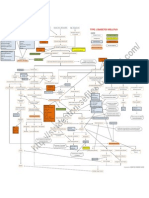
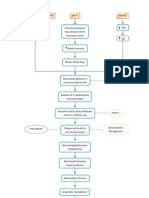
Cues Subjective: sakit akong dughan inig mu ubo ug muginhawa kug lalum. As verbalized by the patient P- when coughing and deep inhalation. Q- sharp pain R- RLQ of abdomen (with penrose drain) S- 3-4/10 T- brief flash pain. Objective: Presence of fine crackles over lung bases . Respiratory Rate 31bpm. Productive cough with white Assisted client to maintain a comfortable position to facilitate breathing by elevating the head of bed, leaning on or over bed table, or sitting on edge of Elevation of the head of the bed facilitates respiratory function using gravity; however, client in severe distress will seek the position that most eases breathing. Supporting arms LTO: Within 3 days of nursing interventions the patient will be free from adventitious sounds and will not manifest any signs or symptoms of respiratoy distress. STO: Within 8 hours of nursing interventions the patient will be able to maintain patent airway, discomfort upon coughing and deep inhalation will be relieved, and will demonstrate behaviors to improve airway clearance. Objectives Independent: Auscultated breath sounds. Noted adventitious breath sounds such as wheezes, crackles, or rhonchi. Some degree of bronchospasm is present with obstructions in airway and may or may not be manifested in adventitious breath sounds, such as scattered, moist crackles (bronchitis); faint sounds, with expiratory wheezes (emphysema); or absent breath sounds Assessed and monitored respiratory rate. (severe asthma). Tachypnea is usually present to some degree and may be pronounced on admission, during stress, or during concurrent acute infectious process. Respirations may be shallow and rapid, with prolonged expiration in comparison to inspiration. LTO: After 3 days of nursing interventions, the patients crackles is still present but no signs of respiratory distress were noted. Nursing Interventions Rationale STO: After 8 hours of nursing interventions, the patient was able to maintain patent airway, pain scale is reduced to 1/10, participated in activities in improving his ability to expectorate lung secretions. Evaluation
th
sputum. with O2 inhalation @2 L/min via nasal cannula (+) Dressing on abdomen, penrose drain and colostomy bag on LLQ. Chest PA View: (+) Minimal pleural thickening, left lower chest.
bed.
and legs with table, pillows, and so on helps reduce muscle fatigue and can aid chest expansion.
Provides client with some means to cope with Encouraged and assist with abdominal or pursedlip breathing exercises (use of spirometry). Cough can be persistent but ineffective, Observed for persistent, hacking, or moist cough. Assisted with measures to improve effectiveness of cough effort. especially if client is elderly, acutely ill, or debilitated. Coughing is most effective in an upright or in a head-down position after chest percussion. and control dyspnea and reduce air-trapping.
Collaborative: Administered medications as indicated: Pulmodual 5-6 drops Q6H RTC Inhaled anticholinergic agents are now considered the first-line drugs for clients with stable COPD because studies indicate they have a longer duration of action with less toxicity potential, whereas still providing the effective relief of the beta-agonists. Used to correct and prevent worsening of Administered 02 inhalation @ 2L/min via nasal cannula. hypoxemia, improve survival, and quality of life. Supplemental oxygen can be provided during exacerbations only, or as a long-term therapy.
Reference: Doenges, M.E. (2008). Nursing Care Plan, 8th ed. p. 124-125
You might also like
- NCP 1 Ineffective Airway ClearanceDocument2 pagesNCP 1 Ineffective Airway ClearanceDivine Jane PurciaNo ratings yet
- NCP #2Document4 pagesNCP #2Nutz TolentinoNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway Clearanceapi-252726911No ratings yet
- 1 Ineffective Breathing PatternDocument8 pages1 Ineffective Breathing PatternNoel MontemayorNo ratings yet
- NCP CKDDocument3 pagesNCP CKDRiel TumandaNo ratings yet
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care Planapi-309251523No ratings yet
- Pleural Effusion FdarDocument1 pagePleural Effusion FdarvanessabdeveraNo ratings yet
- Pneumonia Case Study: Toddler Diagnosis and TreatmentDocument5 pagesPneumonia Case Study: Toddler Diagnosis and TreatmentcrisolandNo ratings yet
- Risk For Aspiration: Risk For Aspiration: at Risk For Entry of Gastrointestinal Secretions, Oropharyngeal SecretionDocument6 pagesRisk For Aspiration: Risk For Aspiration: at Risk For Entry of Gastrointestinal Secretions, Oropharyngeal SecretionAngie MandeoyaNo ratings yet
- CVA Impaired Physical MobilityDocument3 pagesCVA Impaired Physical MobilityJasmineNo ratings yet
- Oxygenation - NCPDocument5 pagesOxygenation - NCPCazze SunioNo ratings yet
- Ineffective Breathing PatternDocument185 pagesIneffective Breathing PatternSusi LambiyantiNo ratings yet
- NCP PTBDocument2 pagesNCP PTBMack Jhed AnarconNo ratings yet
- Drug StudyDocument4 pagesDrug StudyPam RomeroNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway Clearancejancel_bollaNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- (Patho) PTB COPDDocument1 page(Patho) PTB COPDKyle HannahNo ratings yet
- ETOPOSIDEDocument4 pagesETOPOSIDEkajal guptaNo ratings yet
- Risk For Bleeding - Cirrhosis NCPDocument2 pagesRisk For Bleeding - Cirrhosis NCPPaula AbadNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezNo ratings yet
- NCPDocument3 pagesNCPJezza RequilmeNo ratings yet
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocument2 pagesNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- NCP Copd4Document15 pagesNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- Drug StudyDocument20 pagesDrug StudydjanindNo ratings yet
- ANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationDocument2 pagesANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationEdrianne Tui100% (2)
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- Tissue PerfusionDocument2 pagesTissue PerfusionMichael John LeandichoNo ratings yet
- Ineffective Airway Clearance Nursing Care PlanDocument2 pagesIneffective Airway Clearance Nursing Care Planrois romaNo ratings yet
- NCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsDocument3 pagesNCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsSarah Ann Jamilla FaciolanNo ratings yet
- Week 10 Drug Card - Hydrochlorothiazide (HCTZ)Document2 pagesWeek 10 Drug Card - Hydrochlorothiazide (HCTZ)RCurry09No ratings yet
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Document20 pagesSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizNo ratings yet
- PathophysiologyDocument2 pagesPathophysiologyKarla Karina Dela CruzNo ratings yet
- Ineffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaDocument3 pagesIneffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaNiel MinatozakiNo ratings yet
- Nursing Care Plan For Heart Failure ChronicDocument26 pagesNursing Care Plan For Heart Failure ChronicbrantNo ratings yet
- NCP CopdDocument4 pagesNCP CopdJoshua ValdrizNo ratings yet
- Assessment Diagnosis Planning Intervention Evaluation for Impaired Gas ExchangeDocument2 pagesAssessment Diagnosis Planning Intervention Evaluation for Impaired Gas ExchangeCharissa Magistrado De LeonNo ratings yet
- Reduce Cardiac Workload and Chest Pain Nursing Care PlanDocument8 pagesReduce Cardiac Workload and Chest Pain Nursing Care PlanryzaimaliaNo ratings yet
- NCP MiDocument4 pagesNCP MiPitaca Madiam Annabehl PaulNo ratings yet
- Drug Study NitroglycerinDocument2 pagesDrug Study NitroglycerinJoseph Rodney de LeonNo ratings yet
- Manage Bronchiectasis Nursing Care PlanDocument5 pagesManage Bronchiectasis Nursing Care PlanPaola Marie VenusNo ratings yet
- Nursing Care PlanDocument11 pagesNursing Care Planaycee0316100% (1)
- Doxofylline: D 400 MG TabletsDocument33 pagesDoxofylline: D 400 MG TabletsBibek Singh Mahat100% (2)
- Ncp-Ineffective Airway ClearanceDocument3 pagesNcp-Ineffective Airway Clearancelouanne0550% (2)
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanNo ratings yet
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway ClearanceImation DataNo ratings yet
- Pulmonary Rehabilitation GuideDocument61 pagesPulmonary Rehabilitation GuideNur akilaNo ratings yet
- Asthma Nursing Care Plan - NCP - Ineffective Airway ClearanceDocument2 pagesAsthma Nursing Care Plan - NCP - Ineffective Airway ClearanceCyrus De Asis92% (24)
- Impaired Breathing PatternDocument1 pageImpaired Breathing PatternHanya Bint PotawanNo ratings yet
- NCPDocument9 pagesNCPEjie Boy Isaga67% (3)
- Diagnostic Tests and Treatments for Pulmonary DiseasesDocument7 pagesDiagnostic Tests and Treatments for Pulmonary DiseasesKushan SenanayakaNo ratings yet
- NCP TBDocument6 pagesNCP TBGrhace Aquino100% (3)
- Tuberculosis Nursing Care Plan - Ineffective Airway ClearanceDocument2 pagesTuberculosis Nursing Care Plan - Ineffective Airway ClearanceCyrus De Asis86% (36)
- Emphysema Case Study AnalysisDocument10 pagesEmphysema Case Study AnalysisEfren VisteNo ratings yet
- COPD Introduction: Types, Risk Factors, and Nursing CareDocument36 pagesCOPD Introduction: Types, Risk Factors, and Nursing Carejho_No ratings yet
- What Is COPD? Chronic Obstructive Pulmonary Disease (COPD) : Signs and SymptomsDocument11 pagesWhat Is COPD? Chronic Obstructive Pulmonary Disease (COPD) : Signs and SymptomsCecil Bhang-i Cacay - PabloNo ratings yet
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityHanya Bint PotawanNo ratings yet
- MSHC Ordr PRC FormatDocument4 pagesMSHC Ordr PRC FormatHanya Bint PotawanNo ratings yet
- Impaired Verbal and or Written CommunicationDocument2 pagesImpaired Verbal and or Written CommunicationHanya Bint Potawan100% (1)
- Ineffective Cerebral Tissue PerfusionDocument3 pagesIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- Hanieyah Guro OR DR PRC FormatDocument4 pagesHanieyah Guro OR DR PRC FormatHanya Bint PotawanNo ratings yet
- Rhu Day 1 RequirementsDocument4 pagesRhu Day 1 RequirementsHanya Bint PotawanNo ratings yet
- Herbal MedicinesDocument6 pagesHerbal MedicinesHanya Bint PotawanNo ratings yet
- BSN - 4C: PresentorsDocument52 pagesBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- Herbal MedicinesDocument6 pagesHerbal MedicinesHanya Bint PotawanNo ratings yet
- Rhu Day 1 RequirementsDocument4 pagesRhu Day 1 RequirementsHanya Bint PotawanNo ratings yet
- Schizophrenia UndifferentiatedDocument88 pagesSchizophrenia UndifferentiatedHanya Bint Potawan75% (4)
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanNo ratings yet
- Rhu Day 1 RequirementsDocument4 pagesRhu Day 1 RequirementsHanya Bint PotawanNo ratings yet
- Psychotropic DrugsDocument49 pagesPsychotropic DrugsHanya Bint PotawanNo ratings yet
- Pa Tho Physiology - Type 1 Diabetes (Hanieyah Guro)Document1 pagePa Tho Physiology - Type 1 Diabetes (Hanieyah Guro)Hanya Bint PotawanNo ratings yet
- Impaired Skin IntegrityDocument1 pageImpaired Skin IntegrityHanya Bint PotawanNo ratings yet
- DOH Officials Directory Execom MembersDocument2 pagesDOH Officials Directory Execom MembersHanya Bint PotawanNo ratings yet
- Impaired Breathing PatternDocument1 pageImpaired Breathing PatternHanya Bint PotawanNo ratings yet
- Dopamine HydrochlorideDocument1 pageDopamine HydrochlorideJoannes SanchezNo ratings yet
- Angina PectorisDocument2 pagesAngina PectorisHanya Bint PotawanNo ratings yet
- Akiya - DiphtheriaDocument52 pagesAkiya - DiphtheriaHanya Bint PotawanNo ratings yet
- Jose Rizal: 'Those Who Cannot See Where They Came From Will Never Get To Where They Are Going.'Document55 pagesJose Rizal: 'Those Who Cannot See Where They Came From Will Never Get To Where They Are Going.'Anne Ginez BilledoNo ratings yet
- Mr. Bean's diagnostic blood test resultsDocument2 pagesMr. Bean's diagnostic blood test resultsHanya Bint PotawanNo ratings yet
- Wearable and Implantable Sensors For Biomedical ApplicationsDocument22 pagesWearable and Implantable Sensors For Biomedical ApplicationsEsteban MuñozNo ratings yet
- Dental Management of Patients With Respiratory Disease: (Copd)Document12 pagesDental Management of Patients With Respiratory Disease: (Copd)Fahd AlahaidebNo ratings yet
- ACCP Ambulatory CareDocument50 pagesACCP Ambulatory CareJim DansNo ratings yet
- Clinical Practice GuidelinesDocument9 pagesClinical Practice GuidelinesIntel AtomNo ratings yet
- Lung Disease and Copd Seminar PresentationDocument14 pagesLung Disease and Copd Seminar Presentationapi-402325622No ratings yet
- Copd EssayDocument6 pagesCopd Essayapi-384539985No ratings yet
- Respiratory System Mechanics Lab Report SummaryDocument8 pagesRespiratory System Mechanics Lab Report SummaryRara ArifahNo ratings yet
- Prepared By: Mylene Karen B. Pueblas, RNDocument136 pagesPrepared By: Mylene Karen B. Pueblas, RNmylene_karen100% (2)
- NCA1Document12 pagesNCA1Ley BeltranNo ratings yet
- CRT Exam Test QuestionsDocument4 pagesCRT Exam Test QuestionsDharlyn MungcalNo ratings yet
- Diagnosis, Management, and Prevention of Pulmonary Barotrauma During Invasive Mechanical Ventilation in Adults - UpToDateDocument34 pagesDiagnosis, Management, and Prevention of Pulmonary Barotrauma During Invasive Mechanical Ventilation in Adults - UpToDatevmdcabanillaNo ratings yet
- Effect of Treadmill Exercise Training On VO Peak in Chronic Obstructive Pulmonary DiseaseDocument7 pagesEffect of Treadmill Exercise Training On VO Peak in Chronic Obstructive Pulmonary DiseaseAqila Zefanya AriefmanNo ratings yet
- Perioperative NursingDocument32 pagesPerioperative NursingMaria Garcia Pimentel Vanguardia II100% (2)
- Respirology 2023 FinalDocument127 pagesRespirology 2023 FinalBelinda ELISHANo ratings yet
- BAUTISTA, Ryza - 093224Document16 pagesBAUTISTA, Ryza - 093224Charles AtolbaNo ratings yet
- Blue ProtocolDocument11 pagesBlue Protocoloana florianaNo ratings yet
- Borg ScaleDocument2 pagesBorg ScaleAnand LaNo ratings yet
- Physical Assessment Part 2 AssignmentDocument15 pagesPhysical Assessment Part 2 AssignmentKyra Bianca R. FamacionNo ratings yet
- Jurnal 1Document8 pagesJurnal 1Dela Amelia Nur SalehaNo ratings yet
- Keystone Owners Manual 2019 PDFDocument104 pagesKeystone Owners Manual 2019 PDFBreNo ratings yet
- Bronkiolitis AkutDocument10 pagesBronkiolitis AkutNamira Firdha KNo ratings yet
- Merging Result PDFDocument267 pagesMerging Result PDFMuzamil RiasatNo ratings yet
- Obstructive Airways Disease: Asthma and COPDDocument29 pagesObstructive Airways Disease: Asthma and COPDRaxter ErNo ratings yet
- Handling Inhaler Devices Practical Guide Pharmacists 2011Document88 pagesHandling Inhaler Devices Practical Guide Pharmacists 2011Hannah HalimNo ratings yet
- Peter J. Barnes - Tobacco DocumentsDocument55 pagesPeter J. Barnes - Tobacco DocumentsDavid LeloupNo ratings yet
- Manual: ST George'S Respiratory Questionnaire For Copd Patients (SGRQ-C)Document17 pagesManual: ST George'S Respiratory Questionnaire For Copd Patients (SGRQ-C)lion5835No ratings yet
- English4 q1 Mod1of7 Partsofsimpleparagraph v2 QuinoDocument26 pagesEnglish4 q1 Mod1of7 Partsofsimpleparagraph v2 QuinoCyril Joy MorcisaNo ratings yet
- Long-Acting Bronchodilator Use After Hospitalization For COPD: An Observational Study of Health Insurance Claims DataDocument9 pagesLong-Acting Bronchodilator Use After Hospitalization For COPD: An Observational Study of Health Insurance Claims DataSantiFaridKalukuNo ratings yet
- Emergency MedicineDocument150 pagesEmergency MedicineDev MartelNo ratings yet
- Complex Ventral Hernias ReviewedDocument6 pagesComplex Ventral Hernias ReviewedMusdalipaNo ratings yet