Professional Documents
Culture Documents
2nd Year Respiratory Phys-252807
Uploaded by
Christopher WytherOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2nd Year Respiratory Phys-252807
Uploaded by
Christopher WytherCopyright:
Available Formats
SS Passo, Ph.
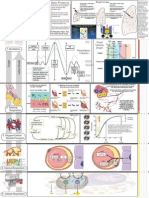
D Respiratory Physiology Review Mechanics Spirometry Tidal Volume Dead Space Alveolar Ventilation Functional Residual Capacity Vital Capacity Obstructive vs. Restrictive Disease Compliance Surfactant Flow-Volume Loops Gas Exchange PO2 Oxyhemoglobin Dissociation Curve Bohr Effect PCO2 CO2 Content Ventilation /Perfusion Ratio Normal Distribution of Ventilation Distribution of Perfusion VA/Qc mismatch A-a Gradient for O2 Causes of Hypoxemia VA/Qc mismatch Right-to left shunt Non-pulmonary hypoxemia Control of Ventilation Peripheral Chemoreceptors Central Chemoreceptors Anemia, CO poisoning Altitude
Spirometry Tidal Volume = VT = Volume of air that enters the lungs per breath Frequency of breathing/minute = f = 12/min Minute Volume = V = VT x f = 500 x 12 = 6000 ml/min
Dead Space (VD): air in the respiratory tree that does not engage in gas exchange Anatomical Dead Space (anat VD): Volume of air in the conducting airways (ml. of air in the anat VD ideal weight in lbs (70kg=150lbs).) Composition: End of inspiration (fresh air; 0% CO2) End of expiration ( used air; same as in alveoli) Alveolar Ventilation (VA) = Volume of fresh air that enters the alveoli/breath VA = V T - V D (500 -150) = 350ml Alveolar Ventilation/minute = VA = Volume of fresh air entering alveoli/min VA = (VT VD)f (500-150)12 = 4200 ml/min Alveolar Dead Space (alv.VD) : refers to air in alveoli that is supposed to engage in gas exchange but cant because there is a problem with perfusion (embolus). Physiological Dead Space (physiolVD)= Total VD = anat VD + alv VD Physiol.VD = anatVD = normal 2
PhysiolVD > anatVD = implies the presence of alv.VD Functional Residual Capacity: The FRC is the volume of air left in the lungs at the end of a passive expiration . It represents the equilibrium position that is achieved when the respiratory muscles are relaxed and the inward elastic recoil of the lungs is exactly balanced by the outward elastic recoil of the thorax Thus, the elastic properties of the lungs will determine the FRC. In highly elastic lungs (fibrosis) the FRC is decreased and the patient appears sunken-chested. In lungs that have lost their elasticity (emphysema; old age) the FRC is increased. The patient appears barrel-chested; the diaphragm is flattened. The diagram below, while not easily duplicated on human subjects, can be used to determine the FRC. .
Vital Capacity: The Vital Capacity (VC) is the maximum volume of air that an individual can move in a single breath. The most useful assessment of the VC is to do it as quickly and forcefully as possible, i.e. a "timed" or Forced Vital Capacity (FVC). During a FVC maneuver, the volume of air exhaled in the first second is called the Forced Expiratory Volume 1sec (FEV1sec). .
FEV1sec = 80% FVC Normal people can only exhale 80% of their VC in one second because during a forced expiration, IPP becomes positive and airways become compressed. Compression of the airways limits expiratory flow rates. Maximum expiratory flow rates are "effort independent". Obstructive Lung Disease FVC - decreased FEV1sec- decreased FEV1sec / FVC - decreased FEF25-75% - decreased Lung Volumes FRC increased RV- increased TLC- increased or normal Compliance curves Restrictive Lung Disease FVC - decreased FEV1sec - decreased FEV1sec / FVC - increased FEF25-75% - increased Lung Volumes: FRC decreased RV -decreased TLC decreased
Surfactant: At tidal volumes above FRC, most of the work of inspiration is expended to overcome the surface tension that exists at the gas - liquid interface of each alveoli. This work would be greater, if not for the presence of surfactant. Surfactant (dipalmitoylphosphatidyl choline) is produced by alveolar type II cells, Surfactant reduces the surface tension and thus increases lung compliance. A. In the absence of surfactant, the surface tension of the film lining the inside of the alveolus is constant and high. Thus, a small alveolus generates a greater pressure than a large alveolus and empties more rapidly (prone to collapse). This leads to progressive atelectasis. Psmall > Plarge
B. In the presence of surfactant, lung compliance is increased and lung stability is promoted, i.e., surfactant prevents progressive atelectasis. It does this by reducing the surface tension more in small alveoli than in large alveoli. . Psmall = Plarge Lung washings from infants with Respiratory Distress Syndrome of the Newborn (RDS) have a high surface tension that shows little variation in S.T. with area. Premature birth and maternal diabetes are risk factors. A lecithin/sphingomyelin ratio (L/S) of 2.0 or greater indicates lung maturity and a minimal risk for RDS. A gestational age of 34 weeks divides those with increased incidence and mortality from those relatively free of the disorder.
Flow-Volume loops found in obstructive and restrictive diseases are shown below. In obstructive disease, the flow-volume loop begins and ends at abnormally high lung volumes and the expiratory flow rate is lower than normal ( often exhibiting a scooped - out appearance ). In restrictive disease, the flow - volume loop begins and ends at unusually small lung volumes. When expiratory flow rates are compared at specific lung volumes, the rates in restrictive disease are somewhat greater than normal.
Gas Exchange Partial Pressure of Alveolar Gas: The partial pressure of alveolar gas depends on the ratio of alveolar ventilation (VA) to pulmonary capillary blood flow (QC). Ideal VA/QC = 0.8
Consequences of a change in VA/Qc : Low VA/Qc (<0.8)= decreased PAO2; increased PACO2 High VA/Qc (>0.8)= increased PAO2; decreased PACO2 O2 Transport Dissolved O2 PO2 reflects the concentration of O2 physically dissolved in the blood.. At a PO2 is 100 mmHg: 0.3 ml O2 is dissolved in 100 ml of blood (0.3 vol%). Maximum hyperventilation raises the PO2 to 130-135 mmHg (0.4 vol%).
Oxyhemoglobin: HbO2 % Saturation The PO2 in blood determines the percent of sites on Hb occupied by O2. When the PO2 is 100 mmHg, the Hb is 97.5% saturated. When the PO2 is 40 mmHg , the Hb is 75%. Same for anemia or polycythemia)
HbO2 Content: Each gram of Hb can combine with 1.34 ml. of O2. If the [Hb] is 15 gm/100ml, then the maximal amount of O2 per 100 ml. in combination with Hb: HbO2 content = (1.34 x Hb conc.)% satn HbO2 (1.34 x 15 )1.00 = 20 ml O2/100 ml blood = 20 vol%
When the PO2 is 100 mmHg, the Hb is 97.5% satd , carrying 19.5 out of a possible 20.0 ml of O2 in every 100 ml of blood (19.5 vol%). At a PO2 of 40 mmHg, the HbO2 content is 15 vol% (75% satd). Hyperventilation can significantly increase the PaO2 , but will have little effect on HbO2 content. Total O2 Content (vol%) = ml O2 dissolved + ml HbO2 PaO2 = 100 mmHg = PaO2 = 130 mmHg = 0.3 0.4 + + 19.5 19.5 = 19.8 vol% = 19.9 vol%
Thus, hyperventilation of healthy units does not add significant amounts of O2 to the blood leaving those units and cannot compensate for the low O2 of blood leaving units with a low VA/Qc Pulmonary disease always leads to hypoxemia Bohr Effect An increase in the PaCO2 , H+, or temperature of blood shifts HbO2 dissociation curve to the right, indicating a decrease in the affinity of O2 for Hb. Thus, the a-v O2 difference increases. A shift in the position of the oxyhemoglobin curve to the left indicates an increase in the affinity of O2 for Hb 2,3 DPG: An increase in 2,3, DPG shifts curve to right. Major stimulus is hypoxemia. 2,3 DPG decreases in outdated blood. Fetal Hb does not bind 2,3, DPG and is shifted to the left
Diffusing Capacity of the Lung for O2 The Diffusing Capacity indicates how many ml.O2 /min diffuse across the lungs Decreased in fibrosis, edema. Increased in exercise
CO2 Transport CO2 Gas Equation: PaCO2 = .86 VCO2 VA The equation predicts that doubling VA will halve the PaCO2
Hyperventilation of healthy lung units can compensate for the high CO2 in blood coming from diseased regions of the lung. Thus, in pulmonary disease the PCO2 can be high, low or normal (depending on degree of hyperventilation and/or severity of disease) CO2 , produced by cellular metabolism, diffuses into the blood where it is carried in 3 different forms:
1) Dissolved CO2 - responsible for the PCO2 2) Carbamino compounds - CO2 reacts with the free amino groups on Hb 3) Reduced Hb better buffer than oxyHb more free NH2 groups exposed 4) HCO3 -- Both in RBC and plasma. Most of the CO2 produced by metabolism is carried in the plasma in the form of HCO3
10
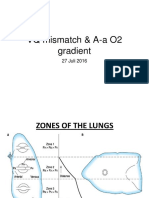
Ventilation - Perfusion Ratio Regional variation in the distribution of Ventilation.
The above diagram refers to a normal individual in the erect position: Because of the weight of the lung (gravity), the IPP is less negative at the base than at the apex. As a consequence, alveoli at the base of the lung are relatively more compressed at FRC, but expand better on inspiration than those at the apex Alveoli at base are more compliant than those at the apex. Upon inspiration, more air goes to the base of the lungs than to the apex. Regional variation in pulmonary blood flow.
The above diagram refers to a normal individual in the erect position. Because the right ventricle develops a low pressure, blood flow to the apex of the lung is compromised. Most of the blood ejected by the right ventricle goes to the base.
11
VA/Qc in the Erect Position (Normal) More air and more blood go to the base of the lungs than to the apex. However, more blood than air goes to the base. Low VA/QC at the base (low PaO2). Alveoli at the apex receive too much air for the amount of blood perfusing them High VA/QC at the apex (high PaO2). A - a Gradient for O2 Indicates the presence of a VA/Qc mismatch; the greater the mismatch, the larger the A -a gradient. If gas from an alveolus with a high PO2 mixes with gas from an alveolus with a low PO2, the PO2 in the resultant gas mixture is the arithmetic mean. If blood with a high PO2 mixes with blood with a low PO2, the PO2 in the resultant blood mixture is less than the arithmetic mean. This latter effect is a direct consequence of the shape of the HbO2 dissociation curve. A - a gradient for O2 Normal pulmonary function (5-10 mmHg): results from the VA/Qc mismatch between apex and base when the thorax is erect. Essentially disappears in the supine position. In the normal range in the hypoxemia associated with anemia and hypoxemia of non-pulmonary origin (coma, myasthenia gravis) Pulmonary disease: > 5-10 mmHg.
12
Causes of Hypoxemia VA/Qc mismatch: Some regions of the lung have VA/Qc < 0.8 but not 0.
Amenable to O2 therapy. A a gradient increased CO2 can be high, low or normal. CO2 retention occurs as severity of disease worsens Right-to-left shunt : Some regions of the lung have VA/QC = 0
Not amenable to O2 therapy A a gradient increased CO2 can be high, low or normal. CO2 retention occurs as severity of disease worsens Non-pulmonary hypoxemia: Entire lung VA/Qc < 0.8 (coma, myasthenia gravis, obesity) Amenable to O2 therapy A a gradient in the normal range CO2 always high
13
VA/Qc > 0.8
VA/Qc = infinity
VA/Qc = infinity represents alv. VD
14
Regulation of Respiration Mechanoreceptors Slowly-Adapting Stretch Receptors: Located in small airways and connected to respiratory centers by afferent fibers in both vagus nerves. Increased afferent vagal activity generated by lung stretch inhibits further inspiration. Bilateral section of both vagus nerves results in a slow, deep pattern of breathing (Hering-Breuer Reflex). J receptors: Free nerve endings in the lung parenchyma that cause a rapid, shallow pattern of breathing when interstitial fluid accumulates (pneumonia, congestive heart failure). Peripheral Chemoreceptors Carotid Body: afferents to CNS in glossopharyngeal nerve (IX) Aortic Body: afferents to CNS in vagus nerve (X) The carotid body is the most important peripheral chemoreceptor in man. It receives the most blood per gram of tissue in the body and can meet all of its requirements for O2 by utilizing the O2 dissolved in blood. Thus, the carotid body will be stimulated whenever the PaO2 falls to a low enough value. Stimuli Primary stimuli: Decrease in PaO2 Decrease in pH Decrease in blood flow Secondary stimulus : Rise in PaCO2;. Sensitivity Oxygen: Carotid body does not begin to fire significantly until the PaO2 falls to 50 - 60 mmHg. Carbon Dioxide: Only about 10-20% of the total ventilatory response to inhaled CO2 is the result of carotid body stimulation.. Hydrogen Ion: A decrease in the pH of blood perfusing the carotid body will lead to an extremely deep and rapid pattern of breathing. Kaussmauls breathing in individuals with a diabetic keto-acidosis Blood Flow: A severe fall in blood flow (anaphylactic or hypovolemic shock) can compromise O2 delivery to the carotid body. Adaptation; Do not adapt
15
Central Chemoreceptors Located on the ventrolateral surface of the medulla in contact with CSF. Stimulus:The hydration of CO2 and subsequent dissociation of H2CO3 in the CSF generates H+ . CSF H+ is the stimulus to central chemoreceptor. Sensitivity: Extremely sensitive. These receptors are responsible for the moment - to - moment control of breathing. Adaptation: The system does adapt; usually within 12-24 hours. Mechanism of adaptation may be the pumping of HC03 into or out of the CSF. Abnormal Situations: Chronic hypoventilation: Though the PaO2 is decreased and the PaCO2 is increased, only the peripheral chemoreceptors are driving respiration. Anemia: Total O2 content is decreased, but the PaO2 is normal. Therefore, there is no peripheral chemoreceptor response to this kind of hypoxia. CO is life - threatening because of the leftward shift in the HbO2 dissociation curve.
16
High altitude The fall in ambient PO2 caused by the decrease in TBP leads to a decrease in PaO2. The hypoxia-induced ventilatory response is due to peripheral chemoreceptor activation and leads to a decreased PaCO2 (respiratory alkalosis) . Other acclimatory responses include an increase in 2,3, DPG and an erythropoetin-stimulated increase in the hematocrit. Associated with the alveolar hypoxia at high altitude is pulmonary vasoconstriction (pulmonary hypertension and right ventricular hypertrophy). The same holds for the alveolar hypoxia associated with pulmonary disease (cor pulmonale). The central chemoreceptors adapt to the respiratory alkalosis so that there is an additional increase in ventilation 12-24 hours after arriving at a high altitude.
17
You might also like
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- Respiratory Physiology: Dr. Okon MRCSDocument41 pagesRespiratory Physiology: Dr. Okon MRCSEdwin OkonNo ratings yet
- Pulmonary Function Tests in Clinical PracticeFrom EverandPulmonary Function Tests in Clinical PracticeAli AltalagRating: 5 out of 5 stars5/5 (1)
- Respiratory FailureDocument7 pagesRespiratory FailureJesse OnealNo ratings yet
- Lung Function in Health and Disease Basic Concepts of Respiratory Physiology and PathophysiologyFrom EverandLung Function in Health and Disease Basic Concepts of Respiratory Physiology and PathophysiologyNo ratings yet
- O2 CascadeDocument6 pagesO2 CascadeBharath NarasimhaNo ratings yet
- Respiratory ICU PDFDocument130 pagesRespiratory ICU PDFAhmed Shihab AhmedNo ratings yet
- Pulmonary Circulation: - The Blood Supply of The Lung Is Derived FromDocument52 pagesPulmonary Circulation: - The Blood Supply of The Lung Is Derived FromMoonAIRNo ratings yet
- Oxygen Delivery UpdateDocument6 pagesOxygen Delivery UpdateRahman Mukti AjiNo ratings yet
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- Measurement of RV, FRC, TLC: Abu Ahmed 2019Document21 pagesMeasurement of RV, FRC, TLC: Abu Ahmed 2019Khalid AbdullahNo ratings yet
- Ventilasi PerfusiDocument44 pagesVentilasi PerfusiIdahrachman515100% (1)
- Acute Respiratory Fauilr - PDF CVS PART 4Document61 pagesAcute Respiratory Fauilr - PDF CVS PART 4LexNo ratings yet
- Oxygen CascadeDocument12 pagesOxygen Cascadehy3pjb1984No ratings yet
- Kaynar2018 Medscape PDFDocument29 pagesKaynar2018 Medscape PDFberlianNo ratings yet
- Pulmonary Physiology - ACS CC Review Course - FinalDocument8 pagesPulmonary Physiology - ACS CC Review Course - FinalIvulik87No ratings yet
- Resp PhysiologyDocument45 pagesResp PhysiologyGirija BhamidiNo ratings yet
- CB (018) Gas Exchange - Influencing Factors QuestionsDocument9 pagesCB (018) Gas Exchange - Influencing Factors QuestionsAbdullah HassanNo ratings yet
- Respiration: Human Respiratory SystemDocument4 pagesRespiration: Human Respiratory SystemSheehan MathurNo ratings yet
- Structure and Function of The Respiratory SystemDocument74 pagesStructure and Function of The Respiratory SystemCasmin Claire Talledo LeonesNo ratings yet
- Oxygenation and Oxygen TherapyDocument11 pagesOxygenation and Oxygen TherapyJenn77x1No ratings yet
- Acute Respiratory FailureDocument11 pagesAcute Respiratory FailureRicardoOswaldoValdiviesoValdiviesoNo ratings yet
- Ventilation: Describe Alveolar and Pulmonary VentilationDocument6 pagesVentilation: Describe Alveolar and Pulmonary VentilationNorrifhan Akmal IsmailNo ratings yet
- (RS) Pneumonia With Severe HypoxiaDocument4 pages(RS) Pneumonia With Severe Hypoxiaapi-3769252100% (2)
- Transpulmonary Pressure Ppul - Pip: Decreased Volume Increased Pressure Increased Volume Decreased PressureDocument1 pageTranspulmonary Pressure Ppul - Pip: Decreased Volume Increased Pressure Increased Volume Decreased Pressurelovelyc95No ratings yet
- The Physiology of Oxygen Delivery: DR Rob Law, DR H BukwirwaDocument4 pagesThe Physiology of Oxygen Delivery: DR Rob Law, DR H BukwirwaPrabhakar KumarNo ratings yet
- Anatomi Fisiologi PernapasanDocument87 pagesAnatomi Fisiologi PernapasanAndre ChundawanNo ratings yet
- Anatomi Fisiologi Pernapasan Dr. MDocument87 pagesAnatomi Fisiologi Pernapasan Dr. MARIF BSNo ratings yet
- Arterial Blood GasDocument255 pagesArterial Blood GasMark Joshua S CruzNo ratings yet
- Report PhysioRes 1Document3 pagesReport PhysioRes 1Said Taysir AbdlJawadNo ratings yet
- M8 - Investigations and Monitoring in The ICUDocument68 pagesM8 - Investigations and Monitoring in The ICUVishal KumarNo ratings yet
- PathoPhyLUNG - Lec1 by CannanDocument13 pagesPathoPhyLUNG - Lec1 by CannanDeline KiruNo ratings yet
- Capnography ExplainedDocument22 pagesCapnography ExplainedmarceloNo ratings yet
- Anesthesia PointsDocument5 pagesAnesthesia PointsRedNo ratings yet
- Physiology of The Lateral Decubitus Position and One-Lung VentilationDocument31 pagesPhysiology of The Lateral Decubitus Position and One-Lung VentilationDebasis Sahoo100% (1)
- Respiratory FailureDocument38 pagesRespiratory Failuredrmithil100% (1)
- Respiratory PhysiologyDocument137 pagesRespiratory PhysiologysramvigneshNo ratings yet
- Respiratory Insufficiency - Pathophysiology,: Diagnosis, Oxygen TherapyDocument11 pagesRespiratory Insufficiency - Pathophysiology,: Diagnosis, Oxygen TherapyBintang UbamnataNo ratings yet
- Respiratory System 2Document26 pagesRespiratory System 2KelvinNo ratings yet
- 1.P Fetal, NeonatalDocument2 pages1.P Fetal, NeonatalWisnu Agung WiyanggaNo ratings yet
- Oxygen Therapy: Dr. Subhankar ChatterjeeDocument49 pagesOxygen Therapy: Dr. Subhankar ChatterjeesubhankarNo ratings yet
- Judul 1: 02 Max O2maxDocument3 pagesJudul 1: 02 Max O2maxwahyana mujari wahidNo ratings yet
- Respiratoryfunctionandimportancetoanesthesia Final 140103050711 Phpapp02Document62 pagesRespiratoryfunctionandimportancetoanesthesia Final 140103050711 Phpapp02rijjorajooNo ratings yet
- Measurement of Gas Exchange - Pulmonary Disorders - Merck Manuals Professional EditionDocument7 pagesMeasurement of Gas Exchange - Pulmonary Disorders - Merck Manuals Professional Editionpeterpavel112No ratings yet
- Functions of The Respiratory SystemDocument20 pagesFunctions of The Respiratory SystembettyNo ratings yet
- Respiratory PhysiologyDocument68 pagesRespiratory PhysiologyDjNo ratings yet
- Resp CH 2Document68 pagesResp CH 2Ahmed khanNo ratings yet
- VQ - O2 GradientDocument27 pagesVQ - O2 GradientIkbal NurNo ratings yet
- Resp Physio SAQsDocument25 pagesResp Physio SAQsanaeshkl100% (1)
- Mechvent Presentation MidtermDocument46 pagesMechvent Presentation Midtermfloremie carinoNo ratings yet
- 11 Respiratory SystemDocument19 pages11 Respiratory SystemSenthereng MoaisiNo ratings yet
- Mechanical Vent Training - Oplinger 11-2010Document5 pagesMechanical Vent Training - Oplinger 11-2010Marc LaBarberaNo ratings yet
- Principals of Mechanical Ventilation in Neonates: DR Mohd Maghayreh PRTH - IrbidDocument78 pagesPrincipals of Mechanical Ventilation in Neonates: DR Mohd Maghayreh PRTH - IrbidAnonymous 58LGc3No ratings yet
- Adeyomoye Respiratory PhysiologyOER6954487Document25 pagesAdeyomoye Respiratory PhysiologyOER6954487hminuwa3No ratings yet
- Breathing and Exchange of Gases: Respiratory OrgansDocument4 pagesBreathing and Exchange of Gases: Respiratory OrgansSreeyansu RajNo ratings yet
- Respiratory Physiology NOTESDocument3 pagesRespiratory Physiology NOTESJulienne Sanchez-Salazar100% (1)
- Pl1. DM Investigations in Pulmonary Diseases: 1. Tests of Pulmonary VentilationDocument6 pagesPl1. DM Investigations in Pulmonary Diseases: 1. Tests of Pulmonary VentilationVittorio Di PaoloNo ratings yet
- Case Studies: Restrictive and Obstructive Respiratory Conditions Case Study # 1Document5 pagesCase Studies: Restrictive and Obstructive Respiratory Conditions Case Study # 1psyarjavierNo ratings yet
- Medical Tasac New - Iso - 1Document11 pagesMedical Tasac New - Iso - 1Mustafa JumaNo ratings yet
- Indian Journal of Physiotherapy and Occupational TherapyDocument8 pagesIndian Journal of Physiotherapy and Occupational TherapygulbudNo ratings yet
- At-A-Glance Outpatient Management Reference For Chronic Obstructive Pulmonary Disease (COPD)Document8 pagesAt-A-Glance Outpatient Management Reference For Chronic Obstructive Pulmonary Disease (COPD)RushdaNo ratings yet
- 5-Pulmonary Function TestsDocument35 pages5-Pulmonary Function TestsDoha JKNo ratings yet
- Libro VM Obeso 2018 PDFDocument305 pagesLibro VM Obeso 2018 PDFNataly Osorio MarínNo ratings yet
- Nirali Final Synopsis PDFDocument31 pagesNirali Final Synopsis PDFNIRALI MISTRYNo ratings yet
- Haad Combined Panel 1-6Document148 pagesHaad Combined Panel 1-6dr reham samirNo ratings yet
- Bronchiolitis ObliteranDocument8 pagesBronchiolitis ObliteranFranciscus BuwanaNo ratings yet
- Body Plethysmography AvneetDocument54 pagesBody Plethysmography Avneetsalimtajamul100% (3)
- Dietary Counselling and Food Fortification in Stable COPD: A Randomised TrialDocument7 pagesDietary Counselling and Food Fortification in Stable COPD: A Randomised TrialJames Cojab SacalNo ratings yet
- Pulmonary Function TestDocument39 pagesPulmonary Function TestLuqman AlwiNo ratings yet
- Bronchial Asthma and ManagementDocument43 pagesBronchial Asthma and ManagementMarius-Sorin CionteaNo ratings yet
- Alpha 3 - 081052Document26 pagesAlpha 3 - 081052Nicolas BerrospiNo ratings yet
- Carestation 620: Key FeaturesDocument10 pagesCarestation 620: Key FeaturesFernandoNo ratings yet
- Ace FinalDocument11 pagesAce FinalJude Andrian CasugayNo ratings yet
- University of Guyana School of Medicine Med 1106 - Physiology I DR Kalima ThompsonDocument66 pagesUniversity of Guyana School of Medicine Med 1106 - Physiology I DR Kalima ThompsonKNo ratings yet
- Journal of Regenerative Medicine & Biology ResearchDocument10 pagesJournal of Regenerative Medicine & Biology ResearchAthenaeum Scientific PublishersNo ratings yet
- Severe Asthma: Definition, Diagnosis and TreatmentDocument9 pagesSevere Asthma: Definition, Diagnosis and TreatmentHalim Muhammad SatriaNo ratings yet
- Therapeutic Potential of Pranayama: Dr. Ananda Balayogi BhavananiDocument13 pagesTherapeutic Potential of Pranayama: Dr. Ananda Balayogi BhavananiArchuNo ratings yet
- Pulmonary Function TestsDocument29 pagesPulmonary Function TestsOrion JohnNo ratings yet
- Spiro ScoutDocument2 pagesSpiro ScoutskyperxNo ratings yet
- Yoga For Bronchial AsthmaDocument208 pagesYoga For Bronchial AsthmabijorajNo ratings yet
- Canmedaj01540 0049Document4 pagesCanmedaj01540 0049ImanNo ratings yet
- Slow Deep Pursed-Lips Breathing Exercise On Vital Lung Capacity in Post-Extubation Patients in The Intensive Care UnitDocument10 pagesSlow Deep Pursed-Lips Breathing Exercise On Vital Lung Capacity in Post-Extubation Patients in The Intensive Care Unitanggi rahmawatiNo ratings yet
- Pulmonary (Notes)Document18 pagesPulmonary (Notes)Jenn CaoNo ratings yet
- COPD Assessment and DiagnosisDocument20 pagesCOPD Assessment and DiagnosisTony LeeNo ratings yet
- Icu and PhysiotherapyDocument81 pagesIcu and PhysiotherapyLakshmi Prasanna100% (2)
- Dissertation Report SpirometerDocument40 pagesDissertation Report SpirometerAbhishek RajanNo ratings yet
- SpiroDocument31 pagesSpiroMoh Arif KurniawanNo ratings yet
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (3)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodFrom EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNo ratings yet
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (351)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- The End of Craving: Recovering the Lost Wisdom of Eating WellFrom EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellRating: 4.5 out of 5 stars4.5/5 (82)
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (411)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisFrom EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisRating: 3 out of 5 stars3/5 (2)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- The Complete Beck Diet for Life: The 5-Stage Program for Permanent Weight LossFrom EverandThe Complete Beck Diet for Life: The 5-Stage Program for Permanent Weight LossRating: 3.5 out of 5 stars3.5/5 (6)
- How Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseFrom EverandHow Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseRating: 4.5 out of 5 stars4.5/5 (84)
- Molecules of Emotion: Why You Feel the Way You FeelFrom EverandMolecules of Emotion: Why You Feel the Way You FeelRating: 4 out of 5 stars4/5 (128)