Professional Documents
Culture Documents
Alterations in Hematologic System Health
Uploaded by
Kelly HollenbeakOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alterations in Hematologic System Health
Uploaded by
Kelly HollenbeakCopyright:
Available Formats
Alterations
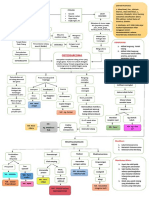
in Hematologic System Health Lymphatic System The lymph system is made up of vessels throughout the body that carry lymph - the colorless fluid, from body tissue, as well as organs such as lymph nodes, the spleen and the thymus. These tissues produce and store infection-fighting cells. Certain parts of other organs such as the tonsils, stomach, small intestine and skin are also part of the lymph system. Lymphatic System Function aids the immune system in destroying pathogens and filtering waste so that the lymph can be safely returned to the circulatory system. removes excess fluid, waste, debris, dead blood cells, pathogens, cancer cells, and toxins from these cells and the tissue spaces between them. works with the circulatory system to deliver nutrients, oxygen, and hormones from the blood to the cells that make up the tissues of the body. Lymphoma Lymphoma refers to a group of cancers of the lymph system. Lymphomas can start in almost any part of the body, but they usually begin in the primary lymphatic organs. Like other cancers, lymphomas can also spread to other body organs. Lymphomas are classified according to the appearance of the cancer cells under the microscope and how they behave when special laboratory tests are applied to them. Treatment decisions are based on the results of these and other studies. Lymphoma Hodgkins lymphoma Non-Hodgkins lymphoma Hodgkins Lymphoma
Hodgkin's lymphoma, previously known as Hodgkin's disease, is a type of lymphoma, which is a type of cancer originating from white blood cells - lymphocytes. Characterized by the orderly spread of disease from one lymph node group to another, and by the development of systemic symptoms with advanced disease. Hodgkin's lymphoma is a cancer of lymph tissue found in the lymph nodes, spleen, liver, bone marrow, and other sites Incidence: The disease occurrence shows two peaks: the first in young adulthood (age 1535) and the second in those over 55 years old More prevalent in young adult males than females The survival rate is generally 90% or higher when the disease is detected during early stages
Hodgkins Lymphoma Etiology Unicentric origin initiates in a single node ReedSternberg cells the malignant cell of Hodgkin's lymphoma, a gigantic tumor cell Suspected viral etiology Epstein-Barr virus (EBV) Familial pattern Hodgkins Lymphoma Presentation The first sign of this cancer is often an enlarged lymph node which appears without a known cause. The disease can spread to nearby lymph nodes Later it may spread to the spleen, liver, bone marrow, or other organs. Hodgkin's lymphoma is most common among people ages 15 - 35 and 50 - 70. Hodgkins Lymphoma Hodgkins Lymphoma Diagnostics Complete blood count (CBC) Blood chemistry Bone marrow biopsy Lymph node biopsy X-rays of the chest look for spread of the disease Ultrasound assess for the disease in the abdomen, kidney and pelvic area Bone scan assess if the disease has spread to the bones CT scan Hodgkins Lymphoma Staging Stage I: is involvement of a single lymph node region or single extralymphatic site
Hodgkins Lymphoma Treatment Treatment primarily depends on the following The type of Hodgkin's lymphoma The stage (where the disease is found) Whether the tumor is more than 4 inches (10 cm) wide The patient's age and other medical issues Treatment varies with the stage of the disease. Stages I and II (limited disease) can be treated with local radiation therapy, chemotherapy, or a combination of both. Stages III and IV (extensive disease) are treated with chemotherapy alone or a combination of radiation therapy and chemotherapy. Hodgkins Lymphoma Prognosis More than 80% of people with stage I or II Hodgkin's lymphoma survive for at least 10 years with the right treatment If the disease has spread, the treatment is more intense and the 5-year survival rate is about 60%. Possible complications Infertility Liver failure Respiratory complications Development of other cancers Side effects of radiation and chemotherapy Non-Hodgkin's Lymphoma (NHL) Lymphoid tissues become infiltrated with malignant cells, spread is unpredictable and localized disease is rare. Incidence increases with age, with average age being 50 to 60. Prognosis varies with type of NHL Treatment is determined by type and stage of disease, and may include interferon, chemotherapy, and/or radiation therapy. Nursing Process: Care of the Patient with Hodgkins and Non-Hodgkins Lymphoma refer to Nursing Process slides for Leukemia Multiple Myeloma Malignant disease of plasma cells in the bone marrow with destruction of bone malignant plasma cells produce increased amount of a specific immunoglobulin that is nonfunctional the specific immunoglobulin - M protein (monoclonal protein) also will have lower than normal quantity of functional immunoglobulins Malignant plasma cells may stimulate angiogenesis creation of new blood vessels to enhance growth of these clusters of plasma cells
Stage II: is involvement of two or more lymph node regions on the same side of the diaphragm or of one lymph node region and a contiguous extralymphatic site Stage III: is involvement of lymph node regions on both sides of the diaphragm, which may include the spleen and/or limited contiguous extralymphatic organ or site Stage IV: is disseminated involvement of one or more extralymphatic organs
Malignant plasma cells may infiltrate other tissues plasmacytomas can occur in the sinuses, spinal cord and soft tissues BenceJones protein Bence Jones protein is a monoclonal globulin protein found in the blood or urine finding this protein is often suggestive of multiple myeloma Median survival 3 to 5 years, no cure
Multiple Myeloma Clinical Manifestations bone pain osteoporosis fractures elevated serum protein hypocalcaemia renal damage renal failure symptoms of anemia, fatigue, weakness increased serum viscosity increased risk for bleeding and infection Any elderly patient whose chief complaint is back pain and has an elevated total protein level should be evaluated for possible myeloma. Multiple Myeloma Medical Treatment Plan chemotherapy corticosteroids radiation therapy biphosphonates strengthen bone and control bone pain and prevent potential fractures BMT or PBSCT to extend remission rather than provide a cure (refer to leukemia slides) plasmapheresis if sign and symptoms of blood hyperviscosity, lower immunoglobulin level Hematologic System The blood and the blood forming sites, including the bone marrow and the reticuloendothelial syst em Blood Plasma Blood cells Hematopoiesis - the complex process of the formation and maturation of blood cells Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell Leukemia Hematopoietic malignancy with unregulated proliferation of leukocytes (white blood cells) Types: Acute lymphocytic leukemia Chronic lymphocytic leukemia Acute myeloid leukemia Chronic myeloid leukemia
Most signs and symptoms of leukemia result from a shortage of normal blood cells occurs when the leukemia cells crowd out the normal blood-making cells in the bone marrow Results decreased production and function of normal: RBCs WBCs Platelets
Acute Leukemias Manifestations Sudden and dramatic onset manifestations that reflect a massive overload of leukemic lymphoblasts in the bone marrow Anemia fatigue and paleness Thrombocytopenia deficiency in blood platelets, can lead to petechiae, excess bruising, bleeding, frequent or severe epistaxis, and bleeding gums. Leukopenia - deficiency in normal white blood cells increases the risk of infections. Neutropenia - refers specifically to low levels of neutrophils, a type of granulocyte, infection develops when counts fall below 500/cu mm. Leukostasis - increased blood viscosity and tendency to clotting, blast count gets very high, cells clog up blood vessels and make it hard for normal red blood cells and oxygen to get to tissues. Spread to lymph nodes, liver, spleen lymphadenopathy, hepatomegaly, splenomegaly results in abdominal discomfort Weakness or fatigue. Swelling or discomfort in the abdomen. Unexpected weight loss or anorexia. Pain in the bones especially sternal area. Joint pain Signs and symptoms of CNS involvement INCREASED ICP, cranial nerve palsies, seizures and coma Acute Lymphocytic Leukemia (ALL) Uncontrolled proliferation of immature cells from lymphoid stem cell INCREASED number of lymphoblasts immature lymphocytes Aggressive type of leukemia without treatment, ALL usually progresses quickly Leukemic cell infiltration is more common with this leukemia ALL occurs in both children and adults accounts for 20% of all adult leukemia most common type of cancer in children twice more frequently in whites than blacks males more frequently than females Prognosis is good for children; 80% 5-year event-free survival, but drops with increased age ALL Causes and Risk Factors Cause remains unknown Small percentage associated with inherited genetic syndromes Anti-cancer drugs ALL Clinical Manifestations Sudden and dramatic onset: Weakness or fatigue. Fever or night sweats.
Bruises or bleeds easily - bleeding gums, petechiae Shortness of breath. Unexpected weight loss or anorexia. Pain in the bones or joints. Swollen lymph nodes, particularly lymph nodes in the neck, armpit, or groin, which are usually painless. Swelling or discomfort in the abdomen. Frequent infections.
ALL Diagnostics Complete blood count with differential INCREASED WBC DECREASED Hgb/Hct Bone marrow biopsy Chemistry panel - including uric acid, creatinine, blood urea nitrogen, potassium, phosphate, calcium, bilirubin, and hepatic transaminases (system involvement) Fibrinogen and tests of coagulation as a screen for disseminated intravascular coagulation. A careful screen for evidence of active infection. Acute Lymphocytic Leukemia Treatment Treatment: Chemotherapy Imatinib Mestylate - if Philadelphia chromosome positive Bone marrow transplant Monoclonal antibody therapy PBSCT peripheral blood stem cell transplant Monoclonal Antibody Therapy Monoclonal antibody - molecule that's carefully engineered to attach to specific defects in your cancer cells. Monoclonal antibodies mimic the antibodies the body naturally produces as part of the bodys immune system make the cancer cell more visible to the immune system - Rituxan block growth signals - Erbitux stop new blood vessels from forming Avastin deliver radiation to cancer cells - Zevalin PBSCT - peripheral blood stem cell transplant Three types of stem cell transplant: Autologous transplants: when patients receive their own stem cells. Allogeneic transplants: when patients receive stem cells from their brother, sister, or parent. An unrelated donor also may be used. Syngeneic transplants: when patients receive stem cells from their identical twin Chronic Lymphocytic Leukemia Malignant B lymphocytes, most of which are mature, may escape apoptosis (programmed cell death) resulting in excessive accumulation of cells Most common form of leukemia
More common in older adults, effects men more often Survival varies from 2 to 14 years depending upon stage
Chronic Lymphocytic Leukemia Clinical Manifestations Lymphadenopathy Hepatomegaly Splenomegaly Later stages anemias and thrombocytopenia autoimmune complications with reticuloendothelial (RES) system destroying RBCs and platelets may occur B symptoms (group of symptoms) include fever, drenching night sweats, weight loss Chronic Lymphocytic Leukemia Treatment Early stage may require no treatment Chemotherapy Monoclonal antibody therapy (refer to Leukemia slides) Acute Myeloid Leukemia (AML) Defect in stem cell that differentiate into all myeloid cells: Monocytes Granulocytes, Erythrocytes Platelets Most common nonlymphocytic leukemia Affects all ages with peak incidence at age 60 Prognosis is variable AML Clinical Manifestations fever and infection weakness and fatigue bleeding tendencies pain from enlarged liver or spleen hyperplasia of gums bone pain Acute Myeloid Leukemia (AML) Treatment Aggressive chemotherapy to achieve complete remission Induction therapy Bone Marrow Transplant PBSCT Chronic Myeloid Leukemia (CML) Mutation in myeloid stem cell with uncontrolled proliferation of cellsPhiladelphia chromosome Stages chronic phase transformational phase blast crisis
Uncommon in people under 20, with increased incidence with age. Mean age: 5560 Life expectancy of 35 years
CML Clinical Manifestations Initially may be asymptomatic Malaise Anorexia, weight loss Confusion or shortness of breath due to leukostasis Enlarged tender spleen, or enlarged liver CML Treatment Imatinib mestylate Gleevec, blocks signals in leukemic cells that express BCR-ABL protein Chemotherapy Bone marrow transplants PBSCT Nursing Process: The Care of the Patient with LeukemiaAssessment Health history Assess symptoms of leukemia, and for complications of anemia, infection, and bleeding weakness and fatigue Laboratory tests Leukocyte count, ANC, hematocrit, platelets, electrolytes, culture reports Nursing Process: The Care of the Patient with LeukemiaDiagnoses Risk for bleeding Risk for impaired skin integrity Impaired gas exchange Impaired mucous membrane Imbalanced nutrition Acute pain Hyperthermia Fatigue and activity intolerance Impaired physical mobility Nursing Process: The Care of the Patient with Leukemia Diagnoses Risk for excess fluid volume Diarrhea Risk for deficient fluid volume Self-care deficit Anxiety Disturbed body image Potential for spiritual distress Grieving diagnoses Deficient knowledge Leukemia Collaborative Problems/Potential Complications Infection Bleeding Renal dysfunction
Tumor lysis syndrome Nutritional depletion Mucositis Depression
Nursing Process: The Care of the Patient with Leukemia- Planning Major goals: absence of complications attainment and maintenance of adequate nutrition activity tolerance ability for self-care and to cope with the diagnosis and prognosis positive body image understanding of the disease process and its treatment Nursing Process: The Care of the Patient with Leukemia - Interventions Interventions related to risk of infection and bleeding Mucositis Frequent, gentle oral hygiene Soft toothbrush, or if counts are low, sponge-tipped applicators Rinse only with NS, NS and baking soda, or prescribed solutions Perineal and rectal care Nursing Process: The Care of the Patient with Leukemia- Improving Nutrition Oral care before and after meals Administer analgesics before meals Appropriate treatment of nausea Small, frequent feedings Soft foods that are moderate in temperature Low-microbial diet Nutritional supplements Blood Product Administration Essential Information: Only two units per filter. Two qualified healthcare professionals must verify units. the major cause of acute transfusion related death is error in identification. Use within four hours after removal from blood bank. Use 20 gauge IV catheter or larger catheter. Obtain Informed consent. PRBC replaces RBCs only. If more than 6-8 units of PRBC are given then give FFP with every other unit. Give platelets one for every unit of PRBC after eight units. Blood Product Administration Obtain and record patients baseline vital signs. Conduct patient teaching and instruct patient to alert staff to the following symptoms: Chest pain. Flushing. Shivering. Abdominal discomfort.
During infusion Continue to monitor the patient for signs and symptoms of adverse reaction during transfusion and 1 hour post- transfusion. If patient experiences a transfusion reaction while transfusion is in progress, immediately stop the transfusion. Maintain patency of line with normal saline and notify MD. Complete transfusion as ordered not to exceed four hours. Tubing sets can be used for second unit of blood if used within four hours. Blood Product Administration Adverse Reactions Pyrexia a temperature of more than 38 C might be due to: Pyrogens resulting from bacterial contamination. Reaction to white cells or platelets which can also be accompanied by chills or rigors. Haemolytic blood reaction (see following slides) The appropriate action is to stop the transfusion and to seek medical advice. Allergic reactions can present as an urticarial rash or a mild pyrexia. can also develop into oedema around the eyes or larynx and cause dyspnoea. full anaphylaxis is uncommon appropriate action is to stop the transfusion and to seek medical advice. subsequent transfusions might require pre-medication with a prescription for an antihistamine Infection although donated blood is screened for major viruses and bacteria (including HIV, hepatitis B, hepatitis C and syphilis), infections, although very rare, do occasionally occur. much more common, however, is local phlebitis which occurs if a cannula remains in situ for too long
Rashes. Shortness of breath. Pain in the loins or extremities. Blood in urine. A feeling of restlessness or anxiety. Feeling generally unwell Febrile patients destroy cells rapidly. If febrile, notify physician to decide if transfusion can wait or if patient should receive acetaminophen as a pre- medication. Adjust the rate of flow for first few minutes, for adults: Platelets or plasma - 2-5 cc/min for 5 minutes Whole blood, RBC or granulocytes - 2cc/min for 15 minutes Patient should be observed closely for the first 15 minutes At the end of the first 15 minutes obtain and record TPR and BP if vital signs are within normal range and the patient has no signs/symptoms of an adverse reaction, change the rate to the desirable rate of infusion infuse the unit within the time period specified in the physicians order.
10
Haemolytic reaction is indicated by: Breathlessness. Collapse. Tachycardia. Hypertension followed by hypotension. Chest or loin pain. Subsequently, the patient might develop: Disseminated intravascular coagulation (DIC) Circulatory and respiratory failure Renal failure. Haemolytic reaction appropriate actions are: 1. stop the transfusion 2. disconnect the pack and giving set 3. maintain the intravenous line with normal saline 4. seek urgent medical advice. Haemolytic reaction This is an emergency, life-threatening situation. Haemolytic reaction is most likely to be due to a patient receiving the wrong blood from one or more errors in the chain of events from taking a cross-match sample, the laboratory processes, the collection of blood for transfusion and administration into the recipient. All blood must be returned to the blood bank and an investigation must be carried out to ascertain the source(s) of the error. Blood Product Administration Adverse Reactions Circulatory overload Circulatory overload causes less of a problem now that concentrated red cells are used more frequently than whole blood. Problems can occur with older people, neonates or patients with megaloblastic anemia. The action to take is to give diuretic therapy as prescribed, slow the rate of transfusion and observe closely for pulmonary and peripheral oedema.
platelets are stored at room temperature and so can act as an ideal medium for bacterial growth. the appropriate action is to check cannula insertion sites regularly for inflammation and infection, and to change the insertion site routinely every 72 hours. when using platelets, bags should be checked for discoloration, which may indicate the presence of bacteria. Haemolytic reaction - a haemolytic reaction is caused by destruction of the donor red blood cells by antibodies in the recipients plasma. It can occur after only a few milliliters of blood are transfused, Although a delayed reaction can occur up to two hours later. Haemolytic reactions can be fatal and as such, a suspected haemolytic reaction must always be responded to as a medical emergency. Blood Product Administration Adverse Reactions
11
Iron overload Patients who receive multiple transfusions have an increased serum ferritin. At a level greater than 1,000mg per liter, the iron infiltrates organs such as the liver, heart and kidneys, which can lead to organ failure or even be fatal. In patients on multiple transfusion programs, an iron chelater such as desferrioxamine can be prescribed to regulate the level of serum ferritin.
12
You might also like
- LymphomaDocument46 pagesLymphomashapan biswaNo ratings yet
- WBC DisordersDocument45 pagesWBC DisordersyalahopaNo ratings yet
- Non-Hodgkin Lymphoma Rhabdomyosarcoma Retinoblastoma: by Derrota, Keith Angelo CDocument39 pagesNon-Hodgkin Lymphoma Rhabdomyosarcoma Retinoblastoma: by Derrota, Keith Angelo CKeith Angelo Canete DerrotaNo ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument30 pagesDisorders of White Blood Cells and Lymphoid Tissuesammar amerNo ratings yet
- Fast Facts: Sézary Syndrome: What Is Lymphoma?Document6 pagesFast Facts: Sézary Syndrome: What Is Lymphoma?Pramita SariNo ratings yet
- Lymphoma: By: Angel R. AggabaoDocument11 pagesLymphoma: By: Angel R. AggabaoSecretNo ratings yet
- LymphomaDocument69 pagesLymphomaDawit g/kidanNo ratings yet
- Hodgkein and Nonhodgkein LymphomaDocument57 pagesHodgkein and Nonhodgkein Lymphomasamar yousif mohamedNo ratings yet
- Disorders of The Lymphatic SystemDocument37 pagesDisorders of The Lymphatic SystemJSeasharkNo ratings yet
- Lymphoma: Pro - Dr.Ahmed EisaDocument45 pagesLymphoma: Pro - Dr.Ahmed EisaOmar Mohammed100% (1)
- LHYMPHOMADocument24 pagesLHYMPHOMACryptic LadyNo ratings yet
- Hodgkin'S LymphomaDocument7 pagesHodgkin'S LymphomaHarish Kumar KumawatNo ratings yet
- Cancer Nursing CareDocument36 pagesCancer Nursing CareSanvar Mal SoniNo ratings yet
- LymphomaDocument37 pagesLymphomaMohammed T. Abdul Razak100% (2)
- Hodgkin Disease: Section 4Document53 pagesHodgkin Disease: Section 4habeba yasserNo ratings yet
- Non Hodgkin's LymphomaDocument27 pagesNon Hodgkin's LymphomaAnsu MaliyakalNo ratings yet
- Non Hodgkin LymphomaDocument16 pagesNon Hodgkin LymphomaadnajaniNo ratings yet
- Hodgkin's LymphomaDocument33 pagesHodgkin's LymphomaAnsu MaliyakalNo ratings yet
- Overview of LymphomasDocument44 pagesOverview of LymphomasHarsha MaheshwariNo ratings yet
- Hodgkin's Dise A Se: CompanyDocument10 pagesHodgkin's Dise A Se: CompanyMahmood SaeedNo ratings yet
- Dr. Ahmed Fawzi Elshaieb Professor of PathologyDocument163 pagesDr. Ahmed Fawzi Elshaieb Professor of PathologyashrafarafaNo ratings yet
- LymphomaDocument20 pagesLymphomaChairul Adilla Ardy100% (1)
- Lymphomas and LeukemiasDocument27 pagesLymphomas and LeukemiasgraceNo ratings yet
- Introduction To LymphomaDocument3 pagesIntroduction To Lymphomalyrad11No ratings yet
- Conditions of The Lymph SystemDocument37 pagesConditions of The Lymph Systemkurage_07No ratings yet
- Malignancy DR RashaDocument29 pagesMalignancy DR RashaRasha TelebNo ratings yet
- 3 Final Lymphoma and MyelomaDocument16 pages3 Final Lymphoma and MyelomaRumela Chakraborty100% (1)
- LymphomasDocument34 pagesLymphomasanimesh vaidyaNo ratings yet
- Hemopoietic SystemDocument28 pagesHemopoietic Systemyfzzhgv676No ratings yet
- L14 Medicine Leukemia (Word)Document6 pagesL14 Medicine Leukemia (Word)Eslam Ibrahiem IbrahiemNo ratings yet
- Lymphoma SignsDocument7 pagesLymphoma SignsDr Keerti MadhukarNo ratings yet
- Bone Cancer (Osteosarcoma) : Carolea Casas & Brittany HogueDocument222 pagesBone Cancer (Osteosarcoma) : Carolea Casas & Brittany Hoguegiggs_libraNo ratings yet
- Medicine Seminar Combined-1Document30 pagesMedicine Seminar Combined-1Deepanshu KumarNo ratings yet
- Non Hodgkin Lymphoma by Dr. AnumDocument43 pagesNon Hodgkin Lymphoma by Dr. AnumHumar HaiderNo ratings yet
- Leukemias 2Document56 pagesLeukemias 2Y. Beatrice AbigailNo ratings yet
- LymphomaDocument5 pagesLymphomaBlossom Wawa IINo ratings yet
- European Day of The Prevention of The Cardiovascular Risk by SlidesgoDocument76 pagesEuropean Day of The Prevention of The Cardiovascular Risk by Slidesgobinojdaniel17No ratings yet
- L-3 Introduction To LeukemiaDocument26 pagesL-3 Introduction To LeukemiaAbood dot netNo ratings yet
- Hodgkin's Lymphoma, Previously Known As Hodgkin's Disease, Is A Type ofDocument9 pagesHodgkin's Lymphoma, Previously Known As Hodgkin's Disease, Is A Type ofMarilou PadillaNo ratings yet
- Limfoma PPT MonceDocument65 pagesLimfoma PPT MonceSylvia PertiwiNo ratings yet
- LymphomaDocument53 pagesLymphomaRobert ChristevenNo ratings yet
- Submitted To:-Submitted By: Ms Jahanara Maam MS - Meena Asst. Professor M.SC (Nursing) 2 YrDocument55 pagesSubmitted To:-Submitted By: Ms Jahanara Maam MS - Meena Asst. Professor M.SC (Nursing) 2 YrMeena KoushalNo ratings yet
- Non Hodgkin LymphomaDocument53 pagesNon Hodgkin LymphomaMeilina Elin WardhaniNo ratings yet
- Pediatric Tumors 1Document35 pagesPediatric Tumors 1SarahNo ratings yet
- LeukemiaDocument37 pagesLeukemiaVikkineshwaran Siva SubramaniamNo ratings yet
- LeukemiaDocument23 pagesLeukemiaAli Ismail86% (7)
- WBC Disorder Chap#4Document41 pagesWBC Disorder Chap#4MuhammadNo ratings yet
- Blockxiv Neoplasms Lymphoid 2006Document54 pagesBlockxiv Neoplasms Lymphoid 2006Ryo RyozNo ratings yet
- Leukemia 2018 For GNM 2ndDocument36 pagesLeukemia 2018 For GNM 2ndshapan biswaNo ratings yet
- LEUKAEMIADocument40 pagesLEUKAEMIADoc HamsNo ratings yet
- Lymphoma by AbrarDocument11 pagesLymphoma by AbrarZain HadiNo ratings yet
- LYMPHOMADocument12 pagesLYMPHOMAश्रीकृष्ण हेङ्गजूNo ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument6 pagesDisorders of White Blood Cells and Lymphoid Tissuesبنين عقيل كاظمNo ratings yet
- Lymphomas: Dr. Y.A. AdelabuDocument28 pagesLymphomas: Dr. Y.A. Adelabuadamu mohammadNo ratings yet
- LeukemiaDocument23 pagesLeukemiaMrnj MelorinNo ratings yet
- 4th Yr GM WBC 3er and 4th Lec.Document43 pages4th Yr GM WBC 3er and 4th Lec.lanasalah.mNo ratings yet
- Lymphoreticular FinalDocument42 pagesLymphoreticular FinalNafis Fuad SheikhNo ratings yet
- Hematological DisordersDocument19 pagesHematological DisordersEZHIL NNo ratings yet
- Surviving Leukemia and Hodgkin's Lymphoma: An Overview Of Effective Treatment MethodsFrom EverandSurviving Leukemia and Hodgkin's Lymphoma: An Overview Of Effective Treatment MethodsNo ratings yet
- Unraveling Cancer: Progress and Future Directions in Cancer ResearchFrom EverandUnraveling Cancer: Progress and Future Directions in Cancer ResearchNo ratings yet
- Kubie, L. (1971) - The Destructive Potential of Humor in PsychotherapyDocument6 pagesKubie, L. (1971) - The Destructive Potential of Humor in PsychotherapyMikaelaMundell100% (1)
- SelectionList R1 Web (MBBS BDS)Document569 pagesSelectionList R1 Web (MBBS BDS)kaushikraj42starNo ratings yet
- 1 A Randomized Clinical Trial of Manual Therapy For Cervico Brachial Pain Syndrome A Pilot StudyDocument8 pages1 A Randomized Clinical Trial of Manual Therapy For Cervico Brachial Pain Syndrome A Pilot StudyCassie RodriguezNo ratings yet
- Abdominal TuberculosisDocument9 pagesAbdominal TuberculosisImmanuelNo ratings yet
- Presentation Resuscitation - Power PointDocument45 pagesPresentation Resuscitation - Power PointRouquia ManzoorNo ratings yet
- Hypersexual DisorderDocument8 pagesHypersexual DisorderAndra ComanNo ratings yet
- Impact of Measles Immunization in Children Less Than Five Years of AgeDocument79 pagesImpact of Measles Immunization in Children Less Than Five Years of AgeUsman Ahmad TijjaniNo ratings yet
- Thesis OsteopathyDocument6 pagesThesis Osteopathygbv8rcfq100% (1)
- CME Trunk, Abdomen, and Pressure Sore ReconstructionDocument15 pagesCME Trunk, Abdomen, and Pressure Sore ReconstructionVeronica TomaselloNo ratings yet
- Amls Als Pretest Version 1.11Document10 pagesAmls Als Pretest Version 1.11ArlanosaurusNo ratings yet
- SwotDocument25 pagesSwotkanikatekriwal126No ratings yet
- A-Plus Multi Criticalcare Brochure Full 20130529 FinalDocument14 pagesA-Plus Multi Criticalcare Brochure Full 20130529 Finalnusthe2745No ratings yet
- The Scoop On Brain Healt Dietary Supplement Products Containing Huperzine ADocument7 pagesThe Scoop On Brain Healt Dietary Supplement Products Containing Huperzine Avasilyi IvanenkoNo ratings yet
- Total Gastrectomy ConsentDocument18 pagesTotal Gastrectomy ConsentTanyaNganNo ratings yet
- KNH 411 Final ExamDocument12 pagesKNH 411 Final Examapi-301897220No ratings yet
- List of Medical AbbreviationsDocument16 pagesList of Medical AbbreviationsClaire Nimor VentulanNo ratings yet
- Allergy Clinic Policy and ProceduresDocument4 pagesAllergy Clinic Policy and ProceduresMiselonNo ratings yet
- Drug Study: Carbocisteine, Paracetamol, Ampicillin. GentamicinDocument4 pagesDrug Study: Carbocisteine, Paracetamol, Ampicillin. Gentamicinpammy28No ratings yet
- Woc Osteosarcoma WidyaDocument1 pageWoc Osteosarcoma WidyaWidya Agustiani0% (1)
- Case Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeDocument5 pagesCase Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeSuci Triana PutriNo ratings yet
- Neurologic ProblemsDocument11 pagesNeurologic ProblemsFilipino Nurses Central67% (3)
- Edwin R. Fisher (Auth.), Prof. Dr. J. Zander, Prof. Dr. J. Baltzer (Eds.) - Early Breast Cancer - Histopathology, Diagnosis and Treatment-Springer-Verlag Berlin Heidelberg (1985) PDFDocument330 pagesEdwin R. Fisher (Auth.), Prof. Dr. J. Zander, Prof. Dr. J. Baltzer (Eds.) - Early Breast Cancer - Histopathology, Diagnosis and Treatment-Springer-Verlag Berlin Heidelberg (1985) PDFMaria MarasteanuNo ratings yet
- Corazon Aquino Delivery RoomDocument5 pagesCorazon Aquino Delivery RoomJustine CagatanNo ratings yet
- Essays Expository TextsDocument5 pagesEssays Expository TextsEddie BaezNo ratings yet
- Pharmaceutical Pakistan PPT 2019Document20 pagesPharmaceutical Pakistan PPT 2019Syed Haider Ali50% (2)
- ACMEDocument15 pagesACMEMony MstNo ratings yet
- CHAPTER 8. AdmissionsDocument9 pagesCHAPTER 8. AdmissionsKumala MadurahayunirwanaNo ratings yet
- Materi WS EWS 2018 - Dr. Habibi - ICU ADMISSION CRITERIADocument22 pagesMateri WS EWS 2018 - Dr. Habibi - ICU ADMISSION CRITERIAIndrati TRNo ratings yet
- An Introduction To Corneal TransplantationDocument2 pagesAn Introduction To Corneal TransplantationNovii NoviiNo ratings yet
- Pts (Peroneal Tendon Strain)Document15 pagesPts (Peroneal Tendon Strain)Yuni FridayaniNo ratings yet