Professional Documents
Culture Documents
Askep KMB
Uploaded by
Khuzaifah Bil Bilal Indra IIOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Askep KMB
Uploaded by
Khuzaifah Bil Bilal Indra IICopyright:
Available Formats
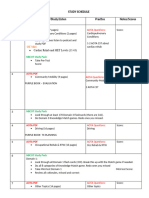
Hal 261 Nursing Diagnosis COMMON RELATED FACTORS Increased or decreased preload Increased afterload Decreased contractility Dysrhythmia
Impaired diastolic function Defining Characteristics Low blood pressure ( BP ) Increased heart rate ( HR ) Decreased urine output Decreased peripheral pulses Cold, clammy skin Crackles Dyspnea Fatigue Edema Restlessness Dysrhythmias Abnormal heart sound Decreased activity tolerance or fatigue Orthopnea or paroxysmal noctural dyspnea ( PND ) Common Expected Outcome Patiens maintains optimally compensated cardiac output, as evidenced by clear lung sounds, no shortness of breath, and absence of or reduced edema. NOC OUTCOMES Circulations status cardiac pump Infectivebess NIC INTERVENTIONS Hemodynamic regulation Dysmythmia management Hal 263 Therapeutic interventions Actions / interventions 1. Weight patient and evaluate trends in weight Rationale : body weight is a more sensitive indicator of fluid or sodium retention than intake and output. A 2- to 3- pound increase in weight usually indicates a need to adjust diuretic drug therapy. 2. administer or evaluate patients home compliance with prescribed medication. Rational :
HF therapy requires administration of several types of medication. The cornerstone of treatment is ACE inhibitors and -blockers. Quadruple therapy adds diutretics and aldesteronc antagonists. Polypharmacy is an ongoing challenge for HF patients. 3. ACE inhibitors ( or angiotensin II receptor blokers) Rationale : these decrease peripheral vascular resistance and venous tone and suppress aldosterone output. This category of drugs has been shown to increase exercise tolerance and survival in HF patients. 4. -Blockers ( e.g.,carvedilol ) Rationale : these drugs are used to decrease neurohormonal activity. They have been shown to reduce mortality, slow disease progression, and improve quality of life. Careful titration of starting doses is required because some patients exhibit fatigue, mood disturbances, or dizziness when medication is started or itrated up. These drugs should be given with food and separated from other vasodilators to reduce side effects ( e.g.,carvedilol with breakfast and dinner, ACE inhibitor with lunch) if side effects are troublesome. 5. Diuretics Rationale : these reduce volume and enhance sodium and water excretion.
6. aldosterone antagonists ( e.g.,spironolactone ) Rationale : these drugs are not given primarily for their diuretic effect, but rather for the beneficial effects on LV improvement in mortality. Patients need to be closely monitored for hyperkalemia. 7.vasdilators (e.g.,nitrates, hydralazine) Rationale : these reduce preload and afterload 8. positive inotropes ( e.g., digoxin, dapomine, dobutmine, milrinone ) Rationale : these improve myocardial contractility. In stable class III to IV patients, intravenous medication may be administreted intermittently in the outpatient or home setting. 9. Antidysrhythmics ( e.g.,amiodarone, -blockers, potassium and magnesium supplements ) Rationale : these correct dysrhythmias such as premature ventricular contractions, ventrikuler contractions, ventricular tachycardia, and atrial fibrillation. HF is one of the most arrhythmogenic disorders. Unfortunately, management of dysrhythmias in this population is usually unsuccessful or even.
Hal 265 Nursing diagnosis Excess fluid volume Common related factors Decreased cardiac output causing the following: Decreased renal perfusion, which stimulates the renin angiotensin-aldosterone sysytem and causes release of antidiuetic hormone. Altered renal hemodynmics ( diminished medullary blood flow ), which result in decreased capacity of nephron to excrete water. Defening Characteristics Weight gain Edema crackles jugular vein distention shortness of breath / orthopnea restlessness elevated cardiovascular pressure and pulmonary capilary wedge pressure ascites / hepatojugular reflux decreased urine output Common Expected Outcome Patient maintains optimal fluid balance, as evidenced by maintenance of stable weight, absence of or reduction in edema, and clear lung sounds. NOC OUTCOME Fluid Balance NIC INTERVENTIONS Fluid Monitoring Fluid Management ONGOING ASSESSMENT Action / intervention 1. monitoring patients char daily weight, assessing for a significant ( great than 2 pounds) weight change in 1 day or trend over several days. Verify that patient has weighed consistently ( e.g.,before breakfast, on the same scale, after voiding, in the same amount of clothing, without shoes). Rationale : such consistency facilitates accurate measurement and evaluation. Weight gain of 2 to 3 pounds indicates excess fluid volume. 2. evaluate weight in relation to nutritional status. Rationale : in some HF patients, weight may be a poor indicator of fluid volume status. Poor nutrition and decreased appetite over time result in a decrease in weight, which may be accompanied by fluid retention, although the net weight remains unchanged.
3. Assess for presence of edema by palpating area over tibia, ankles, feet and sacrum Rationale : symmetrical dependent edema is characteristic in HF; it is graded on a trace to 4 +scale. Pitting edema is manifested by a depression that remains after the finger is pressed over an adematous area and then removed. 4. Auscultate lung sounds and assess for labored breathing. Rationale : elevated pulmonary pressures cause shifting of fluid into interstitial and alveolar spaces.
HAL 267 Actions / intervensions 1. administer or instruct patient to take diuretics as prescribed Rationale ; Diuretic therapy may include several different types of diuretic agents for optimal effect. Patient complaince is often difficult for patients trying to maintain a more normal lifestyle outside the home, who find frequent urination especially troublesome. Some patients prefer taking diuretics later in the day, after their activities. Such creative schedules can increase compliance. 2. instruct patient to notlfly health care provider, about any significant weight changes, leg swelling, or breathing changes. Rationale ; diuretic therapy may include several different types of diuretic agents for optimal effect. Patient compliance is often difficult for patients trying to maintain a more normal lifestyle outside the home, who find frequent urination especially troublesome. Some patient prefer taking diuretics later in the day, after their activities. Such creative schedules can increase compliance. 3. For significant fluid volume excess, consider admission to an acute care setting for hemofltration or ultafiltration. Rationale ; This is an effective method to draw off excess fluid, but patients should be reminded that compliance with medication regimens and sodium restriction will help keep their condition stable.
Nursing Diagnosis Risk for alteration in electrolyte balance Common risk Factors Increased total body fluid ( dilutes electrolyte concentration ) Decreased renal perfusion ( result in greater reabsorption of sodium and potassium ) Diuretic therapy ( enhances renal excreation of total body water and sodium and potassium ) Low sodium diet
Common expected outcome Patient maintains electrolytes within normal range when therapy is stable. Nonacute variation in electrolyte balance is recognized and treated early to prevent complications. Patient receives medication adjustments as needed if electrolyte imbalance is noted. NOC OUTCOME Electrolyte and acid base balance NIC INTERVENTIONS FLUID / ELECTROLYTE MANAGEMENT SPECIFY
Halaman 269 Actions / INTERVENSIONS 1. Encourage daily intake of potassium rich foods ( raisins, bananas, cantaloupe, dates and poatoes ) R = This will assist in correcting deficiency 2. administer magnesium replacement as indicated. R = this may be an oral IV supplement for by hypernatremia : 3. carefully replace water orally or intravenously R = HF patients have a precarious fluid balance status 4. anticipate reduction in diuretic dosage R = Diuretic are commonly the cause of the large water loss resulting in hypernatremia For nonacute hyperkalemia ; 5. Anticipate reduction in potassim supplement R = Some conditions may be easily corrected with reduced supplements 6. Provide diet with potassium restriction as prescribed R = Foods with high potassium nutrients can exacerbate the problem 7. discontinue potassium sparing diuretics as prescribed R = The poassium sparing class of diuretics is often used to counteract the potassium loss associated with loop or thlazide diuretics. However , they can easily lead to hyperkalemia. 8. Instruct the patient to avoid salt substitutes containing potassium : R = all sources of potassium need to be considered
For acute hyperkalemia ( serum potassium greater than 6mEq / L ) :
9.Place patient on ECG monitors R = Common ECG changes may include the following ; tall peaked T waves ; Widened QRS ; Prolonged PR interval ; Decreased amplitude and disappearance of P wave ; Or ventricular arrhythmia. 10.administer the folloing temporary measures as ordered : Regular IV insulin And ypertonic dextrose R = This causes a shift of potassium into the cells. Onset of action is 30 minutes, and duration is several hours. Sodium bicarbonate R = This causes rapid movenment of pottasium into the cells. Onset is within 15 minutes, and duration of action is 1 to 2 hours. Cation exchange resins R = these resins reduce serum potassium levels slowly but have the advantage of actually removing potassim from the body. They are often given with one of the other measures. IV calcium chloride R = Duration of action is 1 hour ; this imediately antagonizes the cardiac and neuromuscular toxicity of hyperkalemia. Dialysis R = this is an effective method for removing potassium but is reserved for situations in which more conservative measures fail. 11.anticipate admission to an acute care setting. R = vigilant monitoring and rapid interventions reduce consequences of hyperkalemia.
Halaman 271 Therapeutic Intervensions Actions / interventions 1. establish guidelines and goals of activity with the patient and significant others. R = Motivation is enhanced if the patient participates in goal setting. Depending on the classification of HF, Some class I or II patients may be able to succesfully work outside the home on a part time or full time basis. However, other patients may be class III or IV and be relatively homebound. 2. use slow progression of activity ( e.g., walking in a room, walking short distance around the house , and then progressively increasing distance outside of the house ( saving energy for return trip ). R= slow progression prevents sudden increarse in cardiac workload. 3. Teach appropriate use of environmental aids ( e.g., bedside commode , chair in bathroom, hall rails )
R= Appropriate aids enable the patient to achieve optimal independence for self-care 4. Teach energy conservation techniques, for example: Setting to do tasks Pushing rather than pulling Sliding rather than lifting Storing frequently used items within easy reach Organizing a work-rest-workschedule R= these techniques reduce oxygen consumption, allowing for more prolonged activity 5. Recommend use of light weights (1 to 2 pouunds) for . Extremity strengthening. R = strength training can enhance endurance and facilitate performance of activities of daily living: such exercises can be performed while sitting in a chair. 6. Consult cardiac rehabilitation or physical therapy departments for assistance in increasing activity tolerance R = specialized therapy or cardiac monitoring may be necessary when initially increasing activity. Some exercises may be provided in the home. A structured program of lowintensity exercise can improve functional capacity, increase self-confidence to exert self, improve quality of life, and provide an environment for early triage of symptoms. 7. Instruct the patient to recognize signs of overexertion. R = this promotes awareness of when to reduce activity and provides data for activity progression. 8. Provide emotional support and encouragement while increasing activity levels. R = support reduces feeling of fear and anxiety. Nursing diagnosis Disturbed sleep pattern Common related factors Anxiety/ fear Physical discomfort or shortness of breath Medication schedule and effects of side effects. Defining characteristic Fatigue Frequent daytime dozing Irritability Inability to concentrate Complains of difficulty falling asleep Interrupted sleep 273 Nursing diagnosis Deficient knowledge
Common related factors with pathology and treatment . Misinterpretation . Medications . Of disease .. teaching or learning in past . Limitation .. Defining characteristics Questioning members of health care team Denial of need to learn Verbalizes incorrect or inaccurate information Development of avoidable complications Common expected outcome . significant others understand and verbalize ., treatment, and follow-up care related .. HF. Noc outcome Knowledge disease process Knowledge treatment regimen Nic intervention Teaching diseases process Teaching prescribed medications Teaching prescribed diet Teaching prescribed activity exercise Ongoing assessment . Knowledge of causes, treatment , and follow-up . To HF Information provides starting base for educstional sessions misconceptions regarding care Understanding any misconceptions the patient may have about the treatment or side effects will guide future interventions. Therapeutic interventions or significant others about the follow- Patients are better able to ask questions and seek assistance when they know basic information about disease and treatment and circulation This is helpful in understanding the diseases process . Process Knowledge of disease and disease process will promote adherence to suggested medical therapy.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Stages of LaborDocument51 pagesStages of LaborZeen_Zeen_Fern_3128100% (4)
- Padhle 10th - Life ProcessesDocument74 pagesPadhle 10th - Life ProcessesBhumik HingveNo ratings yet
- Pierre Beaunegre Resume 08142020Document2 pagesPierre Beaunegre Resume 08142020api-520872874No ratings yet
- Urine Specimen Types and CollectionDocument7 pagesUrine Specimen Types and CollectionRyan KadavilNo ratings yet
- Influence of Diet On The Gut Microbiome and Implications For Human HealthDocument17 pagesInfluence of Diet On The Gut Microbiome and Implications For Human HealthDiana Maria Amaya CruzNo ratings yet
- Vomiting BirdsDocument2 pagesVomiting BirdsJumbosizeNo ratings yet
- Interpretation of The Lab Result (Except Urinalysis) : (Adiba)Document4 pagesInterpretation of The Lab Result (Except Urinalysis) : (Adiba)EkahBaikCantikNo ratings yet
- Your Lab Focus: Cellular Sedimentation and Barrier Formation Under Centrifugal Force in Blood Collection TubesDocument5 pagesYour Lab Focus: Cellular Sedimentation and Barrier Formation Under Centrifugal Force in Blood Collection TubesMichalis PolydorouNo ratings yet
- Hepatitis B QuizDocument2 pagesHepatitis B QuizBianca Watanabe - RatillaNo ratings yet
- Initial Treatment Factors Associated With Feline Urethral Obstruction Recurrence RateDocument8 pagesInitial Treatment Factors Associated With Feline Urethral Obstruction Recurrence RateWilliam ChandlerNo ratings yet
- Factors Affecting Mental HealthDocument4 pagesFactors Affecting Mental HealthSamantha CorpuzNo ratings yet
- Opalescence Boost 40 PercentDocument4 pagesOpalescence Boost 40 PercentAnthony GamarraNo ratings yet
- Bio PoemDocument3 pagesBio Poemapi-4039173890% (1)
- Can Postoperative Nutrition Be Favourably Maintained by Oral Diet in Patients With Emergency Temporary Ileostomy? A Tertiary Hospital Based StudyDocument5 pagesCan Postoperative Nutrition Be Favourably Maintained by Oral Diet in Patients With Emergency Temporary Ileostomy? A Tertiary Hospital Based StudydwirizqillahNo ratings yet
- Evidenced-Based Nursing I. Clinical QuestionDocument3 pagesEvidenced-Based Nursing I. Clinical QuestionLemuel Glenn BautistaNo ratings yet
- NBCOT Study GuideDocument6 pagesNBCOT Study GuideAlainaNo ratings yet
- Test Bank For Prescotts Microbiology 11th Edition Joanne Willey Kathleen Sandman Dorothy WoodDocument29 pagesTest Bank For Prescotts Microbiology 11th Edition Joanne Willey Kathleen Sandman Dorothy WoodJesseFarrellqojgf100% (22)
- UNIT II MedicalDocument34 pagesUNIT II Medicalangelax1.1No ratings yet
- Final Announcement Liver UpdateDocument13 pagesFinal Announcement Liver Updatenerissa arvianaNo ratings yet
- Types of TextDocument2 pagesTypes of TextRodriguez OscarNo ratings yet
- Pleomorphic AdenomaDocument4 pagesPleomorphic AdenomaRobins DhakalNo ratings yet
- Swine Flu InfoDocument20 pagesSwine Flu InfoUdit SinghNo ratings yet
- Aki Ola Shs Text BookDocument1 pageAki Ola Shs Text BookmargaretboronsumNo ratings yet
- Public Health Group AssignmentDocument7 pagesPublic Health Group AssignmentNANNYONGA OLGANo ratings yet
- Biology C - Lesson 1 - Circulatory SystemDocument46 pagesBiology C - Lesson 1 - Circulatory SystemMuhammad Azrie0% (1)
- Acute Suppurative Otitis MediaDocument41 pagesAcute Suppurative Otitis Mediarani suwadjiNo ratings yet
- Cell Tissue Technology SDN BHDDocument5 pagesCell Tissue Technology SDN BHDRaffandi RolandoNo ratings yet
- Monospot LatexDocument12 pagesMonospot Latexlai cruzNo ratings yet
- Adrians H MahajiDocument8 pagesAdrians H MahajiRhara A'nna MardjukuNo ratings yet
- Herbal Medicine and The Gastrointestinal SystemDocument79 pagesHerbal Medicine and The Gastrointestinal Systemryanti adlanNo ratings yet