Professional Documents
Culture Documents
Ncm106 Notes 2012 ABC
Uploaded by
Marie Frances Lalican-RingelOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ncm106 Notes 2012 ABC
Uploaded by
Marie Frances Lalican-RingelCopyright:
Available Formats
NCM106 notes Acute Biologic Crisis
Archeans 2012
SHOCK AND INTERNAL INJURIES Shock is the common denominator in a wide variety of disease processes that presents as an immediate threat to life Simply defined, shock is inadequate tissue perfusion This inadequate tissue perfusion is the result of failure of one or more of the ff: The heart (pump failure) Blood Volume Arterial Resistance Vessels The capacity of the venous beds Any condition that significantly affects any of the above may precipitate a shock state
c.
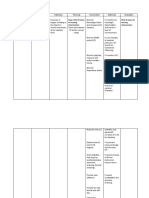
CLASSIFICATIONS OF SHOCK 1. Hypovolemic Shock Occurs when a significant amount of fluid is lost from intravascular space This fluid may be blood, plasma, or electrolyte solution May result from hemorrhage, burns, GI losses or fluid shifts. Cardiogenic Shock Occurs when the heart fails as a pump Primary causes of this failure are myocardial infarction (MI), serious cardiac dysrhythmias, and myocardial depression Secondary causes include mechanical restriction of cardiac function or venous obstruction (cardiac tamponade, vena cava obstruction, tension pneumothorax) Distributive Shock Septic Anaphylactic (systemic vasodilation) Neurogenic a. Septic Shock caused by infection characterized by symptoms of sepsis plus hypotension and hypoperfusion despite adequate fluid volume replacement Anaphylactic Shock A severe, whole body allergic reaction After being exposed to a substance like bee sting venom, the persons Ayie/Trix/Rheiz/Noemi/Faye*
immune system becomes sensitized to that allergen On a later exposure, an allergic reaction may occur. This reaction is sudden, and involves the whole body Anaphylaxis can occur in response to any allergen Neurogenic Shock Sometimes called vasogenic shock, results from the disruption of ANS control over vasoconstriction The veins and arteries immediately dilate, drastically expanding the volume of the circulatory system, with a corresponding reduction of BP
Other classifications (rare types): Spinal Shock Insulin Shock
Primary Assessment and Interventions Rapid recognition and prompt intervention are essential to increase the chance of survival because a downward spiral of physiologic responses will occur if shock is not treated The initial priorities in the assessment are the same for all types of shock Is the airway open? Is the patient breathing? Is there a circulation problem? Initiate immediate interventions as indicated. Resuscitate as necessary. Administer O2 Start cardiac monitoring Control hemorrhage Assess LOC (important indicator of shock because it reflects cerebral perfusion) Changes may include: Confusion Irritability Anxiety Agitation Inability to concentrate Watch for increasing lethargy progressing to obtundation and coma, indicating progression of shock Monitor arterial blood pressure. (Fall in the systolic pressure) There is no absolute value in BP that indicates a shock state
2.
3.
b.
NCM106 notes Acute Biologic Crisis
Archeans 2012
It is the deviation from normal that is important A systolic pressure below 80 mmHg or a MAP below 60 mmHg is indicative of shock Assess pulse quality and rate change. The rate is usually increased Weak, thread pulse due to decreased cardiac output and increased peripheral vascular resistance Assess urine output. A decrease in renal BF or pressure will result in decreased urine output Ideally in an adult, the urine output should be 30 to 60 mL/hour An output of less than 25 mL/hour may indicate shock Assess capillary perfusion. Pale, ashen, mottled, cold and sweaty skin indicates potent vasoconstriction Capillary refill greater than 2 seconds indicated vasoconstriction Also assess for: Subjective feeling of impending doom Metabolic acidosis due to anaerobic metabolism within the cells Excessive thirst
General Interventions Administer 100% O2 by nonbreather face mask to maintain the partial pressure of arterial oxygen at 90 to 100. Assist with intubation if the patient is unable to maintain airway. Fluid resuscitation. Two large bore IV lines should be established Ringers Lactate is the initial fluid choice (normal saline is the second choice because hyperchloremic acidosis may develop if massive amount of normal saline is infused) Rate of infusion depends on severity of blood loss and clinical evidence of hypovolemia Packed RBCs are infused when there is massive blood loss Additional platelets and coagulation factors are given when large
amounts of blood are needed because replacement blood is deficient in clotting factors. Warm the blood (commercial warmer) *massive blood replacement has a cooling effect that can cause cardiac dysrhythmias, paradoxical hypotension, decreased oxyhemoglobin dissociation, or cardiac arrest. Insert an indwelling urinary catheter. Record urine output every 15-30 minutes Urinary volume reveals adequacy of kidney and visceral perfusion Maintain patient in supine position with the legs elevated. This position is contraindicated in patients with head injuries ECG monitoring Dysrhythmias may contribute to shock Maintain ongoing nursing surveillance of total patient to assess patient response to treatment Color V/S CVP ABGs Urine output ECG decreased HCT and Hemoglobin decreased coagulation profile decreased electrolytes Immobilize fractures to minimize blood loss Maintain normothermia. Too much heat produces vasodilation can increase fluid loss through perspiration A patient who is in septic shock should be kept cool because high fever will increase the cellular metabolic effects of shock Pharmacologic Interventions Vasopressors (ADH) may be necessary, but not until volume is replaced Antibiotics (broad spectrum for septic shock)
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
NURSING ALERT! Trendelenburgs position is no longer recommended because of the potential respiratory compromise because of pressure on abdominal organs
HEAD INJURIES Can include fractures to the skull and face, direct injuries to the brain (as from a bullet), and indirect injuries to the brain (such as a concussion, contusion, or intracranial hemorrhage).
Specific Head Injuries Concussion: A temporary loss of consciousness that results from a transient interruption of the brains normal functioning Contusion: A bruising of the brain tissue. Actual small amounts of bleeding into the brain tissue Intracranial Hemorrhage: bleeding into a space or potential space between skull and brain Complications of a head injury are rising intracranial pressure (ICP) and brain herniation Can be classified as epidural hematomas, subdural hematomas, or subarachnoid hemorrhages depending on the site of bleeding NURSING ALERT! Assume a cervical spine fracture for any patient with a significant head injury, until proved otherwise PRIMARY ASSESSMENT Airway: assess for vomitus, bleeding and foreign objects. Ensure cervical spine immobilization, use jaw thrust technique without head tilt. Suction heavy vomitus. Do not stimulate the gag reflex as this can cause increase in ICP. Breathing: assess for abnormally slow or shallow respirations. An elevated CO2 partial pressure can worsen cerebral edema. Administer high flow O2, the most common
cause of death from head injury is cerebral anoxia. Assist inadequate respirations with a bag-valve mask as necessary. Prophylactic hyperventilation not indicated. Control bleeding Apply a bulky, loose dressing with no pressure to all head injuries. Do not attempt to stop the flow of blood or CSF from nose or ears Initiate two IV lines. The rate of flow should be determined by the patients hemodynamic status. Irreversible brain damage: 4 mins. Circulation: assess pulse and bleeding Disability: assess the patients neurologic status
SUBSEQUENT ASSESSMENT History LOC -
Mechanism of injury Duration of loss of consciousness Memory of the event Position found
Change in the LOC is the most sensitive indicator of a change in patients condition Glasgow Coma Scale Vital Signs HTN and bradycardia are late signs of increasing ICP. Head-injured patients may have associated cardiac dysrhythmias, noted by an irregular or rapid pulse Unequal or unresponsive pupils Confusion or personality changes Impaired vision One or both eyes appear sunken Seizure activity Periauricular ecchymosis (battles sign) Rhinorrhea or otorrhea (indicative of leakage of CSF) Periorbital ecchymosis
NURSING ALERT! If basilar skull fracture or severe midface fractures are suspected, a NGT is contraindicated. An orogastric tube may be considered for insertion
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
Keep the neck in a neutral position with the cervical spine immobilized Establish an IV line of normal saline or Lactated Ringers fluid volume should be restricted Be prepared to manage seizures- if seizures occur, they should be controlled immediately Maintain normothermia
Pharmacologic Interventions Anticonvulsants to control seizures Mannitol (Osmitrol) to reduce cerebral edema and decrease ICP Antibiotics Antipyretics to control hyperthermia.
CERVICAL SPINE INJURIES Serious injuries because the crushing, stretching and rotational shear forces exerted on the cord at the time of trauma can produce severe neurologic deficits Edema and cord swelling contribute further to the loff of spinal cord function Any person with a head, neck or back injury or fractures to the upper leg bones or to the pelvis should be suspected of having a potential spinal cord injury until proved otherwise.
Forearms flexed across the chest C6 injury Arms stretched out above the head cervical injury Hypotension and bradycardia accompanied by warm, dry skin suggests spinal shock Neck and back pain/extremity pain or burning sensation to the skin History of unconsciousness Total sensory loss and motor paralysis below level of injury Loss of bowel and bladder control; usually urinary retention and bladder distention Loss of sweating and vasomotor tone below level of cord lesion Priapism persistent erection of penis. Hypothermia due to inability to constrict peripheral blood vessels and conserve body heat Loss of rectal tone
NURSING ALERT! A spinal cord injury can be made worse during the acute phase of injury, resulting in permanent neurologic damage. Proper handling is priority.
GENERAL INTERVENTIONS Insert an NG tube Keep the patient warm Initiate IV access Insert an indwelling urinary catheter to avoid bladder distention Monitor for hypotension, hyperthermia and bradycardia Continue with repeated neurologic examinations to determine if there is deterioration of spinal cord injury Be prepared to manage seizures Pharmacologic interventions: high dose steroids (Methylprednisolone) The standard regimen is 30 mg/kg IV loading dose over 15 mins followed by a 5.4 mg/kg/hr infusion to be initiated 45 mins later Continue the infusion for 23 hours.
Primary Assessment Provide immediate immobilization of the spine while performing assessment Airway. Breathing. Intercostal paralysis with diaphragmatic breathing Shortness of breath produces increased respiratory rate and difficulty in speaking Circulation Disability assess neurologic status
Subsequent Assessment Immobilize the cervical spine Open the airway using the jaw-thrust technique without head tilt If the patient needs to be intubated, it may be done nasally If respirations are shallow, assist with bag-valve mask (ambu bag) Assess the position of the patient when found; this may indicate the type of injury incurred
MAXILLOFACIAL TRAUMA Injuries to the head frequently resulting in the facial lacerations and fractures to the facial bones (i.e. nasal fractures, orbital fractures, maxillary fractures, and mandibular fractures)
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
PRIMARY ASSESSMENT Initiate immobilization of the spine while performing assessment Airway obstruction can occur due to tongue swelling (fractured jaw), bleeding, or broken or missing teeth Breathing may be impaired due to an obstructed airway Circulation control bleeding Disability
Gently apply ice to areas of swelling or ecchymosis. This may reduce further swelling and pain However, if you suspect an injury to the eye itself, do not apply ice If other injuries permit, elevate head of bed With the potential for a CSF leak, the patient should be instructed not to blow the nose, cough, sneeze
PRIMARY INTERVENTIONS Establish and maintain an airway This includes having high flow O2 Inserting an oral airway, or assisting with intubation A nasopharyngeal airway should be used only if there is no evidence of nasal fractures or CSF leakage from nose Control bleeding do not apply pressure to the injury site Apply a bulky, loose dressing Do not attempt to stop the flow of blood or CSF from the nose or ears
Nursing Alert! Nursing Tip Do not use chemical ice packs near a victims eye; chemical ice packs could leak and burn ice. Do not apply pressure on an injured eye
Possible pharmacologic interventions MSO4 (Duramorph) Pain Management Diazepam (Valium) Sedation
SUBSEQUENT ASSESSMENT Examine the mouth for broken or missing teeth Assess for a potential eye injury, vision loss, double vision or pain in the eye Examine the eye for dysconjugate gazeincoordination of eye movements Paralysis of the upward gaze is indicative of an inferior orbit fracture (blowout fracture) Crepitus or a cracking feeling on palpation around the nose usually indicates a nasal fracture Malocclusion of the teeth is indicative of a maxilla or mandible fracture
ABDOMINAL INJURIES Account for a large percentage of trauma-related injuries and deaths The visceral organs contained within the abdomen can be classified as either hollow or solid. Damage to a hollow organ can result in acute peritonitis leading to shock within a few hours Penetrating abdominal injury Usually the result of gunshot wounds or stab wounds Blunt abdominal injuries Usually caused by motor vehicle accidents of falls Trauma to the abdomen is frequently associated with extra-abdominal injuries (i.e. chest, head, and extremity injuries) and severe concomitant trauma to multiple intraperitoneal organs Causes more delayed complications, especially if there is injury to liver, spleen or blood vessels which can lead to substantial blood loss into the peritoneal cavity
*Zygoma (cheekbone) fracture A palpable flattening of the cheek and a loss of sensation below the orbit
Spasms of the jaw (trismus) and mobility of the jaw indicate a maxilla fracture Rhinorrhea or otorrhea (indicative of leakage of CSF).
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
PRIMARY ASSESSMENT & INTERVENTIONS Assess airway, breathing and circulation Initiate resuscitation as indicated Control bleeding, and prepare to treat shock If there is an impaled object in the abdomen, leave it there Stabilize the object in place with bulky dressings along the sides of the object. Obtain history of mechanism of the injury, type of weapon, and estimated amount of blood loss If the patient was stabbed, how long was the blade? Was the person who stabbed the patient a man or a woman? Men usually hold a knife underhand & stab/thrust upward Women usually will stab/thrust downward with an overhand motion If the patient sustained a gunshot wound, attempt to ascertain the type of gun and range at which shot Time of onset of symptoms Passenger location (driver frequently sustains spleen/liver rupture). Were safety belts worn? Did the airbag deploy? Inspect the abdomen for obvious signs of injury (penetrating injury, bruises) Evaluate for signs and symptoms of hemorrhage frequently accompanies abdominal injury, especially if the liver and spleen have been traumatized Note tenderness, rebound tenderness, guarding, rigidity and spasm Press area of maximal tenderness (let patient point the area) Remove fingers quickly to check for rebound tenderness (pain suspected point indicates peritoneal irritation) Ask about referred pain: Kehrs sign pain radiating to the left shoulder may be a sign of blood beneath the left diaphragm pain in right shoulder can result from laceration of liver Looking for increasing abdominal distention Measure abdominal girth at umbilical level in early assessment Serves as a baseline from which changes can be determined
Auscultate for bowel sounds A silent abdomen accompanies peritoneal irritation Auscultate for loss of dullness over solid organs (liver, spleen) Indicates presence of free air; dullness over regions normally containing gas may indicate presence of blood Look for chest injuries, which frequently accompany intra-abdominal injuries Cullens sign A slight bluish discoloration around the navel, a sign of hemoperitoneum Pain is a poor indicator of an abdominal injury Rebound tenderness and boardlike rigidity are indicative of a significant intra-abdominal injury A rectal exam and examination of the perineum should be done on all patients The presence of blood may be indicative of trauma.
GENERAL INTERVENTIONS Goals are to control bleeding, maintain blood volume and prevent infection Keep the patient quiet and on the stretcher (movement may fragment or dislodge a clot in a large vessel and produce massive hemorrhage) Cut the clothing away from the wound Do not cut through bullet holes or stab marks, this will be needed by law enforcement authorities as forensic evidence Count the number of wounds Look for entrance and exit of wounds If the patient is comatose, immobilize the cervical spine until after cervical films are taken and cleared Apply compression to external bleeding Insert two large bore IV lines and infuse Ringers Lactate If possible, one of the lines should be in a central venous location Insert an NG tube to decompress the abdomen This will serve to empty the stomach, relieve gastric distention and facilitate abdominal assessment
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
If blood is found, it may indicate stomach injury or esophageal injury Do not attempt to replace the protruding organs into the abdomen Use sterile saline dressings to protect viscera from drying Cover open wounds with dry dressings Withhold oral fluids to prevent increased peristalsis and vomiting Insert an indwelling urethral catheter to ascertain the presence of hematuria and to monitor urine output If the fracture of the pelvis is suspected, a catheter should not be placed until the integrity of the urethra is ensured Prepare for peritoneal lavage when there is uncertainty about intraperitoneal bleeding Prepare for surgery if the patient shows evidence of: Unexplained shock Unstable VS Peritoneal irritation
Broad spectrum antibiotics because bacterial contamination is a frequent complication (depending on history and nature of wound)
INJURIES TO THE BONE AND JOINTS Common Usually obvious injuries and may be dramatic in nature Rarely are these injuries life-threatening
Fractures may be caused by: Direct trauma Projectiles, crush injuries Indirect trauma Bones being pulled apart or rotational forces Pathologic reasons Weakness in the bone s/t disease process such as metastatic cancer
Other injuries include: Dislocation Complete displacement or separation of a bone from its normal place of articulation It may be associated with a tearing of the ligaments Example, shoulder, elbow, finger, hips, and ankles are the joints most frequently affected Subluxation Partial disruption of the articulating surfaces Can cause minimal transition problems Sprains Injuries in which ligaments are partially torn or stretched Usually caused by a twisting of a joint beyond its normal range of motion The severity can range from mild-severe
*Prepare the patient for diagnostic procedures 1. 2. 3. 4. 5. Catheterization and urinalysis As a guide to possible urinary tract injury and to monitor urine output Type and crossmatch and serial Hgb and Hct levels Their trend reflects presence or absence of bleeding Complete Blood Count (CBC) WBC is generally elevated with trauma Serum Amylase Elevation Indicates pancreatic injury or perforations of GI tract CT Scan Permit detailed evaluation of abdominal and retroperitoneal injuries Abdominal and Chest Xrays May reveal free air beneath diagram
6.
Pharmacologic Interventions Tetanus prophylaxis
Strains Stretching or tearing of muscle and tendon fibers Usually caused by overexertion or overextension Ex. Hamstrings muscle tear PRIMARY ASSESSMENT Always ensure the adequacy of airway, breathing and circulation before initiating treatment Occult blood loss into a closed space from the fracture may be significant enough to produce Hypovolemic shock death by exsanguination can occur from pelvic and femoral fracture
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
Estimated blood loss from closed fractures in L Tibia 1.5 L Femur 2 L Pelvis 6 L Humerus 2 L A fractured cervical spine, pelvic fracture of fractured femur may produce life threatening injuries Posterior dislocations of the hip are life and limbthreatening emergencies due to the potential for blood loss and disruption in blood supply to the head of the femur The patient may develop avascular necrosis of the femoral head and subsequently may require a hip replacement Support airway, breathing, circulation if compromised Initiate IV line and treat for shock if evident Protect injured part from movement or further trauma. Splinting in position may be helpful Seek information on the mechanism of injury How did the injury occur? In what position was the limb after the injury? Did the person fall? How many feet did the person fall? What was the direction and amount of force? Certain musculoskeletal injuries commonly occur together. Assess for the presence of concomitant injuries. A fractured calcaneus as a result of a fall from a great height may also include a compression fracture of the spine Perform neurovascular assessment to include the area above and below the injury Assess for ischemia to the extremity Pallor suggests poor arterial perfusion, cyanosis suggests venous congestion Assess neurologic supply of the injured extremity to determine peripheral nerve insult. Damage to a peripheral nerve can be the result of a direct injury, compression or edema Test sensory, motor function Numbness or paralysis may require immediate medical intervention Examine the bones and joints adjacent to the injury If there was enough force to produce one injury, there may be other injuries Signs and symptoms of fractures Pain & tenderness over the site Grating or Crepitus over the fracture site Swelling due to internal bleeding and edema Deformity, unnatural position, or movement where there is no joint Loss of use or guarding Discoloration due to bleeding in the surrounding tissue Shortening of an extremity or rotation of extremity Loss of joint motion may appear frozen Obvious deformity lump, ridge, excavation Severe pain Signs and symptoms of sprain Pain in the joint area Swelling
Limited use or movement Elevate to prevent or limit swelling Apply ice packs or cold compresses; ice should not be placed directly on skin Cover open fractures with sterile dressings Splint the extremities Handle the part gently and as little as possible Provide pain management Assess for compartment syndrome
Six Ps of CS Pain Development of a different type of pain or the return of pain after tx/splinting had caused pain relief Pallor Pulselessness Paresthesias Paralysis late sign Puffiness late sign If CS is suspected, do not elevate limb above the level of the heart, this may decrease perfusion to compromised extremity SOFT TISSUE INJURIES Involve the skin and underlying subQ tissue and muscles Can be classified as open or closed injuries A closed wound is an injury to the soft tissue but without a break in the skin Closed wounds include: Contusion bleeding beneath the skin into the soft tissue. Bleeding can be minor or extensive. Extensive bleeding can cause severe pain and swelling, leading to a compromised vital structures Hematoma An open wound is an injury to soft tissue with a break in the skin generally they are more serious than closed injuries due to the potential for blood loss and infections. Open wounds include: Abrasion superficial loss of skin resulting from rubbing/scraping the skin over a rough surface Laceration Puncture occurs when skin is penetrated by a pointed object, can be penetrating (entrance wound only) or perforating (entrance and exit wound). Do not cause external bleeding but there may be significant internal bleeding and damage Avulsion involves a tearing off or loss of a flap of skin Amputation PRIMARY ASSESSMENT Always ensure the adequacy of ABC before initiating treatment If bleeding from injury is significant, be aware of the clinical symptoms and signs of shock Skin pale, mottled, cold diaphoretic Tachypnea, tachycardia, hypotension, restlessness (confusion and anxiety) -
Ayie/Trix/Rheiz/Noemi/Faye*
NCM106 notes Acute Biologic Crisis
Archeans 2012
Assess for arterial or venous bleeding Arterial bleeding (bright red, spurts from wound) Venous bleeding (darker red, will flow steadily from a wound) Wounds that result in severe arterial bleeding should be considered life threatening. Tx is second only to CPR Primary goal: Control severe bleeding Direct Pressure Cover injury with sterile dressings Apply firm, direct pressure to the site of injury Should be maintained until bleeding stops, pressure dressing applied, definitive tx undertaken If dressing becomes unsaturated, reinforce dressing After bleeding has stopped, apply pressure dressing. A pressure bandage is made by securing several gauze pads with a rolled gauze bandage Allows the nurse freedom to assess the injury site Elevate injured area. Do not elevated if there is a presence of pain Pressure points Used when direct pressure and elevation cannot control bleeding alone or when DP cannot be applied to a bleeding site due to a protruding bone Locate pressure point, apply firm steady pressure If heavy bleeding is still not controlled and patient may exsanguinate, tourniquet and vascular clamp may be applied to the artery, torniquet is the last option Expose the wound, cut away clothing as necessary, do not removed impaled objects Assess vascular status Perform neurologic assessment Determine tetanus immunization History of injury, including when and how wound occurred: any wound that is more than 6hrs old is considered high risk for infection, and primary closure by suturing may not be an option Wound prep Shave the area necessary, eyebrows are never shaved Irrigate gently with isotonic sterile saline solution or sterile water to remove dirt and debris Catheter tip syringe may be used General rules (wound irrigation) Irrigate with 50mL/inch of wound per hour of age of wound. Use more irrigant for grossly contaminated wounds, clean with a surgical scrub sponge and irrigate The wound may first be anesthesized if patient cannot tolerate wound irrigation Infiltrated with local anesthetic IV thru wound margins or by regional nerve block Devitalized tissue and foreign matter are removed (inhibits wound healing and enhances chance of bacterial infection) Wound closure Closure by primary intent Wound is repaired without delay after injury, yields the fastest healing
Primary closure may be with sutures, skin tapes, staples and adhesives Closure by secondary intent Wound is allowed to granulate on its own without surgical closure Wound is cleaned & covered with a sterile dressing Closure by secondary intent with surgical closure Wound is cleaned and dressed Patient returns in 3-4 days for definitive closure Wound dressing Should be applied in 3 layers. 1st layer: contact layer. Ex. Adaptic, petroleum gauze, xeroform gauze 2nd layer: absorbent layer, dressing pads, 4 x 4 gauze dressings 3rd layer: outer wrap, holds dressing in place. Consists of rolled gauze and tape PHARMA INTERVENTIONS Give antimicrobial tx as directed depending on infection potential: how injury occurred, age of wound, presence of soil Give tetanus prophylaxis based on patients immunization status and wound. Tetanus toxoid with diphtheria and TIG PATIENT EDUCATION Inform patient that pain should subside within 24hours Acetaminophen (Tylenol) or prescribed analgesic, taken for the first 24hrs after a simple laceration Elevate extremity for 1st 28hours Sleep with the head elevated if facial lacerations are present Recommend that the wound would be elevated to limit accumulation of fluid in the interstitial space
Ayie/Trix/Rheiz/Noemi/Faye*
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Cis 2017 PDFDocument3 pagesCis 2017 PDFTheresa IlanoNo ratings yet
- 392 FullDocument7 pages392 FullMarie Frances Lalican-RingelNo ratings yet
- 12Lec-Dermatologic InfectionsDocument69 pages12Lec-Dermatologic InfectionsCarmela MamintaNo ratings yet
- Preventive Pediatrics 2016Document59 pagesPreventive Pediatrics 2016Marie Frances Lalican-RingelNo ratings yet
- Anatomy Supertable PDFDocument14 pagesAnatomy Supertable PDFAlex Ondevilla100% (1)
- Topnotch Surgery Reviewer PDFDocument81 pagesTopnotch Surgery Reviewer PDFMarie Frances Lalican-Ringel100% (16)
- Heat StrokeDocument6 pagesHeat StrokeMarie Frances Lalican-RingelNo ratings yet
- Synthesis of AcetycholineDocument3 pagesSynthesis of AcetycholineMarie Frances Lalican-RingelNo ratings yet
- Blood TransfusionDocument5 pagesBlood TransfusionCla67% (3)
- Endo AlterationsDocument8 pagesEndo AlterationsMarie Frances Lalican-RingelNo ratings yet
- NCP NeuroDocument2 pagesNCP NeuroMarie Frances Lalican-RingelNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionMarie Frances Lalican-RingelNo ratings yet
- Dr's OrderDocument3 pagesDr's OrderMarie Frances Lalican-RingelNo ratings yet
- Dr's OrderDocument3 pagesDr's OrderMarie Frances Lalican-RingelNo ratings yet
- Osteoporosis CADocument3 pagesOsteoporosis CAMarie Frances Lalican-RingelNo ratings yet
- Dr's OrderDocument3 pagesDr's OrderMarie Frances Lalican-RingelNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionMarie Frances Lalican-RingelNo ratings yet
- Pancreatic Enzymes Do Not Work in An Acidic Environment The Need For An Alkaline Rich FluidDocument17 pagesPancreatic Enzymes Do Not Work in An Acidic Environment The Need For An Alkaline Rich FluidMarie Frances Lalican-RingelNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hypovolemic ShockDocument9 pagesHypovolemic Shockfbathan100% (1)
- Anaphylactic Shock Nursing NotesDocument6 pagesAnaphylactic Shock Nursing Notesjtlammers100% (1)
- Blood Pressure Measurement in Pregnancy: ReviewDocument8 pagesBlood Pressure Measurement in Pregnancy: ReviewNalin AbeysingheNo ratings yet
- 10-2019 - Canine Tactical Combat Casualty Care (CTCCC)Document17 pages10-2019 - Canine Tactical Combat Casualty Care (CTCCC)pibulinNo ratings yet
- Inotropes and VasopressorsDocument63 pagesInotropes and VasopressorsCraig DuHaney50% (2)
- Handbook of Critical Care Drug Therapy PDFDocument382 pagesHandbook of Critical Care Drug Therapy PDFntnquynhproNo ratings yet
- Atwood Management of Acute Coronary Syndrome 2022Document14 pagesAtwood Management of Acute Coronary Syndrome 2022goten ramirezNo ratings yet
- Crush Syndrome: Dario Gonzalez, MD, FACEPDocument8 pagesCrush Syndrome: Dario Gonzalez, MD, FACEPMDC101No ratings yet
- Thesis Dry EyeDocument7 pagesThesis Dry Eyebsfp46eh100% (2)
- Anaesthesia in Emergency Laparotomy: Speaker:P.Shravani Moderator:Dr.K.Vinay Assistant ProfessorDocument52 pagesAnaesthesia in Emergency Laparotomy: Speaker:P.Shravani Moderator:Dr.K.Vinay Assistant ProfessorSanthi Swetha PudhotaNo ratings yet
- General Teaching HospitalDocument40 pagesGeneral Teaching Hospitalmenna zewailNo ratings yet
- Distributive Shock 1Document41 pagesDistributive Shock 1Fuzi HannyNo ratings yet
- Shock - Critical Care Medicine - MSD Manual Professional EditionDocument11 pagesShock - Critical Care Medicine - MSD Manual Professional Editionazaria zhafirahNo ratings yet
- Adult Medical Emergencies HandbookDocument317 pagesAdult Medical Emergencies HandbookRasheid Mekki100% (16)
- Fluid Therapy in DengueDocument54 pagesFluid Therapy in DengueVithiya Chandra SagaranNo ratings yet
- Shock: Deepa Murali Ms IvDocument59 pagesShock: Deepa Murali Ms Ivdee0212No ratings yet
- Ped Med HandbookDocument33 pagesPed Med HandbookDaniela Marie RonquilloNo ratings yet
- Aluminium Phosphide MSDS Issue Oct 2011Document5 pagesAluminium Phosphide MSDS Issue Oct 2011misterpokeNo ratings yet
- SNB Reviewer Updated July 2023Document53 pagesSNB Reviewer Updated July 2023Maria Julryn Jariol PaterezNo ratings yet
- Surgery Quiz Topics 1 5Document48 pagesSurgery Quiz Topics 1 5Hello AngelNo ratings yet
- August 2023 (P2) - 1Document309 pagesAugust 2023 (P2) - 1Sherpao khan100% (1)
- Dr. Jufri Latief (Compartment Syndromes)Document11 pagesDr. Jufri Latief (Compartment Syndromes)shintaNo ratings yet
- Janumet PM eDocument62 pagesJanumet PM eRaffi DerderianNo ratings yet
- 3rd Grading Exam (Grade 9)Document5 pages3rd Grading Exam (Grade 9)marynelb27100% (1)
- Critical Care CasesDocument7 pagesCritical Care CasesJude Micko Bunyi AlipitNo ratings yet
- Jaspreet Singh: Is Certified in Standard First Aid & CPR/AED Level C (Blended) Meets CSA Standard Z1210-17 - IntermediateDocument3 pagesJaspreet Singh: Is Certified in Standard First Aid & CPR/AED Level C (Blended) Meets CSA Standard Z1210-17 - IntermediateJaspreet Singh SalhanNo ratings yet
- 07 Blood Pressure Abnormality 1-8-2021 配布用Document22 pages07 Blood Pressure Abnormality 1-8-2021 配布用Lan NguyenNo ratings yet
- Acute Diarrhea and Shock in The EDDocument5 pagesAcute Diarrhea and Shock in The EDmohamed fahmyNo ratings yet
- Perioperative Nursing CareDocument17 pagesPerioperative Nursing CareMisikir Eyob100% (1)
- Intestinal ObstructionDocument12 pagesIntestinal ObstructionNurul Nurnita100% (1)