Professional Documents
Culture Documents
Relapse
Uploaded by
Emil Eduardo Julio RamosOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Relapse
Uploaded by
Emil Eduardo Julio RamosCopyright:
Available Formats
Originals
J. M. Haro1 A. Ciudad2 J. Alonso3 M. Bousoo4 D. Surez1 D. Novick5 I. Gilaberte2
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
1 2
Fundacin San Juan de Dios. Sant Boi de Llobregat (Barcelona) (Spain) Clinical Research Department of Research and Development Lilly, S. A. Alcobendas (Madrid) (Spain)
Research in Sciencies of Health Unit IMIM Hospital del Mar Barcelona (Spain) 4 Psychiatry Department Universidad de Oviedo Oviedo (Asturias) (Spain)
European Health Outcomes Research Eli Lilly and Company Limited Windlesham Surrey (Reino Unido)
Introduction. Three year data collected in the frame of the SOHO study within Spain were used to evaluate antipsychotic treatment outcomes by analyzing remission and relapse as well as the factors influencing them. Methods. The SOHO was a prospective, long-term, observational study of the outcomes of schizophrenia treatment in ambulatory who initiated therapy or who changed to a new antipsychotic drug performed in 10 European countries, with a focus on olanzapine. This article reports the attainment of international schizophrenia clinical remission and relapse criteria and the associated correlates in these patients. Results and conclusions. A total of 2,020 patients were recruited in Spain. Almost 2/3 (60.1%) of the patients met the criteria for clinical remission. Factors that influence the likelihood of remission were identified, such as gender, baseline clinical and/or functional status, time since treatment initiation, treatment with olanzapine versus oral typical antipsychotics, duration of treatment, gender or the need for concomitant anxiolytics. Relapse occurred in 18.7% of patients. Treatment with quetiapine or the prescription of anticholinergics was associated with a greater risk of relapse. Conclusions. These results highlight some prognostic factors of the course of schizophrenia and underscore the importance of the antipsychotic choice and its maintenance to achieve favorable long-term clinical outcomes in routine practice.
Key words: Schizphrenia. Antipsychotic agents. Outcome assessment. Health care surveys. Prospective studies.
Remisin y recada en el tratamiento ambulatorio de los pacientes con esquizofrenia. Resultados a 3 aos
Introduccin. Los datos del seguimiento de 3 aos realizado para el estudio SOHO en Espaa se han empleado para evaluar los resultados del tratamiento antipsictico en trminos de incidencia y factores asociados a la remisin y la recada. Mtodos. El SOHO es un estudio observacional, prospectivo, longitudinal realizado en 10 pases europeos sobre los resultados del tratamiento de la esquizofrenia en pacientes ambulatorios que inician o modifican su farmacoterapia antipsictica con el objetivo particular de comparar olanzapina con los dems antipsicticos. El presente artculo presenta la incidencia y los factores asociados a la remisin y recada clnicas de la esquizofrenia (definidas segn los criterios internacionales al uso) en la muestra espaola. Resultados. En Espaa se reclutaron 2.020 pacientes. Casi dos tercios (60,1%) cumplieron los criterios de remisin clnica. Se identificaron varios factores relacionados con la probabilidad de remisin, tales como el sexo, el estado clnico y/o funcional basal, el tiempo de evolucin desde el primer tratamiento para esquizofrenia, el tratamiento con olanzapina frente a antipsicticos tpicos orales y la prescripcin concomitante de frmacos ansiolticos. El 18,7 % de los pacientes present alguna recada. El tratamiento con quetiapina y el uso concomitante de anticolinrgicos se asociaron con un mayor riesgo de recada. Conclusiones. Los resultados de este estudio sealan algunos factores asociados a la evaluacin de la esquizofrenia y subrayan la importancia de una correcta eleccin del frmaco antipsictico y su mantenimiento para lograr un resultado clnico favorable a largo plazo en la prctica clnica habitual.
Palabras clave: Esquizofrenia. Antipsicticos. Resultados en salud. Encuestas de salud. Estudios prospectivos.
Actas Esp Psiquiatr 2008;36(4):187-196
Correspondence: Josep Mara Haro Abad Fundacin San Juan de Dios Dr. Antoni Pujadas, 42 08830 Sant Boi de Llobregat (Barcelona) (Spain) E-mail: jmharo@comb.es
Actas Esp Psiquiatr 2008;36(4):187-196
187
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
INTRODUCTION
The efficacy and safety of atypical antipsychotics for the treatment of schizophrenia have been well established thanks to the results of several experimental studies and these have been considered for the up-dating of the international treatment guidelines1-3. However, there is still no final consensus on the role that this group of drugs has for the clinician in the actual clinical practice4. Translating the results of the randomized clinical trials into routine clinical practice is hindered by the inherent limitations of these studies, such as strict selection criteria, small sample sizes or short follow-up periods5. Given the complexity of schizophrenia, the gap between experimental clinical research and routine practice is even wider than in other chronic disorders; but, to date, the efforts made to perform observational studies aiding to close such a gap have been scarce. In general, the naturalistic studies conducted have methodological limitations that affect their external validity, for example, cross-sectional or retrospective designs, reduced sample sizes or lack of appropriate control groups6-11. The improvement of therapeutic (pharmacologic and non-pharmacologic) options has helped to better characterize and control the disease course of schizophrenia. The classical view of a progressive evolution towards a chronic illness with substantial morbidity and persistent deficits in cognition and psychosocial function has given way to the more optimistic notion based on the prolonged symptom stability as an attainable goal12. Furthermore, long-term symptomatic stability is not only a possible outcome but may also be a foundation for functional improvement. In other words, maximum efficacy is achieved with psychosocial therapies and rehabilitation only when there is an adequate control of the symptoms. The aims of this article were to assess in a large sample of outpatients with schizophrenia in Spain who initiated treated with a new antipsychotic: a) the clinical outcomes of antipsychotic treatment in terms of remission and relapse, and b) the factors that influence these outcomes.
whether this substituted another previous one, was added to a previous treatment or if they had not been taking any antipsychotic medication previously were invited to participate. The patients should have been receiving ambulatory treatment or, if hospitalized, should not have been hospitalized for more than 15 days and it only should have been indicated for treatment change. The patients should be at least 18 years of age and not be participating in any clinical trial. As the primary purpose of the study was to compare olanzapine with the other antipsychotics, two patient cohorts of similar size were recruited: a) those who initiated or changed to olanzapine therapy as single drug therapy and b) those who initiated or changed to or added a nonolanzapine antipsychotic therapy. Thus, the olanzapine group was over-sampled to obtain a sample in which approximately 50 % of patients had initiated treatment with this drug. To avoid interference with routine practice, the psychiatrists were instructed to make treatment decisions before and independently from assessing patients for enrolment, the recruitment period was purposely long, and the investigators were not committed to a minimum recruitment. The ethics committees of the regional communities involved approved the protocol beforehand and obtained written informed consent from each participant to gather information before their recruitment. The study protocol did not include any restriction regarding the patients' treatment, neither before nor after their inclusion, this being left up to the discretion of the participating psychiatrists.
Study assessments
The data was collected during the routine visits occurring along the patients' treatment. The intention was to obtain data at three and six months after the initiation/change of therapy that motivated the enrolment in the study and then every six months until the completion of the three-year follow-up period. In order not to reduce the impact on the usual practice, a period allowing for a range of one month before and one month after the foreseen dates to gather the information was established. Those patients who did not come to the routine visit within any of these periods were not withdrawn from the study, however, in such case, the corresponding assessment was left blank. Three types of outcomes, clinical severity, quality of life and social functioning, were assessed. For the clinical severity, the Clinical Global Impression-Schizophrenia (CGI-SCH) scale was used. This instrument is an adaptation from the CGI scale to assess overall, positive, negative, depressive and cognitive symptoms at the time of the visit with physician6
METHOD Study design
The SOHO is a prospective, 3 year, observational study of the treatment of schizophrenia in Europe. It pays special attention to the outcomes obtained when the patient is treated with olanzapine. In Spain, 2020 patients were recruited between September 2000 and December 2001 and were followed-up by 86 psychiatrists from different settings (public or private, urban or rural) with a wide geographical distribution. Those patients who initiated treatment with an antipsychotic for the treatment or schizophrenia, regardless of
188
Actas Esp Psiquiatr 2008;36(4):187-196
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
rated scores ranging from 1 (not ill) to 7 (among the most severely ill patients)14. It requires only a few minutes to administer, thus having a minimal impact on the observational nature of the study. The advisory board of the SOHO study agreed on the criteria of definitions of clinical remission and relapse based on these scores prior to knowing study results. In agreement with the Andreasen et al.13 criteria, remission was defined as an overall, positive, negative and cognitive score lower than or equal to 3 in two consecutive visits separated by at least six months in the absence of any inbetween hospitalization. Relapse was defined as the need for hospitalization or increase of at least 2 points in the overall CGI-SCH score that ends in a moderately severe or worse score. Those patients who did not achieve an overall CGI score equal to or lower than 3 throughout the 3 year period were excluded from the analysis of the relapses since patients who did not achieve clinical improvement could not relapse. Given the importance of hospitalizations in cost-effectiveness evaluations, the occurrence of hospitalizations and their associated factors were analyzed separately. Other data were collected on quality of life using the EuroQoL-5 Dimensions (EQ5D), featuring the descriptive part and the visual analogue scale (VAS); social functioning with the social functioning scale, concomitant medications, compliance with treatment, violence/arrest episodes, health resource utilization, social and employment statuses, and appraisal of global activity. The results of these outcomes are outside of the scope of this article.
12-18, 18-24, 24-30 and 30-36 months was analyzed as dependent variables of the model. The medication that the patient was receiving at the first visit of each interval, taking olanzapine as the reference category, was considered to analyze the outcome. The model was also adjusted for baseline differences between the cohorts, taking the baseline status of each patient into account. The following clinical and sociodemographic clinical variables were included in the model as independent variables demographic: gender; clinical; age at first treatment for schizophrenia, time since first treatment, alcohol or substance dependency and/or abuse, suicide attempts, overall positive, negative, depressive and cognitive CGI-SCH, hostility, treatment compliance, body mass index; social functioning: marital status, living independently, having paid employment, being socially active; side effects: extrapyramidal symptoms, amenorrhea; gynecomastia; impotence; galactorrhea, tardive dyskinesia; medication: use of concomitant medication (anticholinergics, antidepressants, anxiolytics, and mood stabilizers), and the visit in question and the medication that the patient was taking at the beginning of each of the periods, defined as the last medication that had been prescribed to the patient. Cox proportional hazards method was used to analyze the risk of relapse. The independent variables used were the antipsychotic (cohort) that the patient was taking in the last visit prior to the relapse, using the olanzapine cohort of reference and those that had been described in the logistic regression model on remission. In addition, an independent Cox hazards risk model was prepared to investigate separately the factors associated to the hospitalization. No a priori calculation was made of the sample sizes used in each one of these analyses because they were done using subgroups of patients from the principal study. Adjustment for multiple comparisons was also not considered.
Statistical analyses
Treatment cohorts were defined based on the antipsychotic treatment initiated in the first visit, considering the following categories: olanzapine, risperidone, quetiapine, clozapine, other atypical antipsychotics, and any oral typical antipsychotic, depot typical antipsychotic, two or more antipsychotics. Incidences of remission and relapse and the factors influencing them were compared among study cohorts by means of multivariate analyses. Backward stepwise selection of variables with significant predictive ability was performed to abridge the models. Furthermore, time to each of these events was analyzed using the Kaplan-Meier method. Time to relapse was imputed by the mid-point between two consecutive visits for those patients who fulfilled the hospitalization criteria. Analysis of the factors associated to achieving clinical remission during the follow-up period was made with a GEE (generalized estimating equation) logistic model. Presence of remission in each one of the intervals ranging from 6-12,
7
RESULTS Sample characteristics
The 2,020 patients included and followed-up in Spain account for 18.4 % of the total sample of the SOHO study (10,972 patients). Of these, 27 were excluded from all analyses either because they could not be ascribed to any treatment cohort or did not meet the selection criteria. Most of the patients were receiving typical antipsychotics prior to enrolment, were male, received treatment in the public healthcare system, lived in an urban setting, and changed their treatment because of lack of efficacy. The olanzapine cohort accounted for 54.8% of the sample (1,092 patients). Among the remaining patients (901 patients), 51.8 % (467 patients; 23.4% of the total sample) started treatment with risperidone and 20.3 % (183 patients; 9.2 % of the total)
189
Actas Esp Psiquiatr 2008;36(4):187-196
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
with quetiapine. A total of 2.4% of the patients (22; 1.1% of the total) initiated polytherapy (two or more antipsychotics), this always being with typical antipsychotics. In table 1 there are more details about the antipsychotic drugs started by the patients at the time of enrolment. Sociodemographic and clinical characteristics were generally homogeneous among study cohorts with the exception of the proportion of patients who initiated treatment for the first time, that were greater in the olanzapine and risperidone cohorts; and the body mass index, that was lower in the olanzapine cohort. A complete description of this sample has been reported in a previous article15.
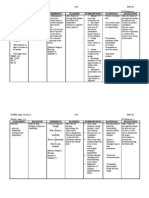
Table 1
Absolute and relative frequencies of the treatments initiated by patients recruited in the SOHO study in Spain
Number of patients (%)
Patients in the olanzapine group Patients in control group Risperidone Quetiapine Any typical depot antipsychotic Any typical oral antipsychotic Clozapine Two or more antipsychotics Any other atypical antipsychotic
1,092 (54.1) 901 (45.9) 467 (51.8) 183 (20.3) 98 (10.9) 94 (10.4) 34 (3.8) 22 (2.5) 3 (0.3)
Analysis of remission
A total of 1,366 patients (68.5% of the total of the evaluable Spanish sample). Those patients in the other atypical antipsychotic cohort, those who did not complete the 3 year follow-up, those who had missed more than one visit or had incomplete data in CGI-SCH evaluations or hospitalization assessments were excluded. In all, 821 (60.1%) patients met the remission criteria. By cohorts (fig. 1), patients treated with olanzapine and clozapine showed the highest remission rates (65.5 % and 60 %, respectively), while the lowest ones were observed in those treated with typical depot or with polytherapy (28 % and 45.5 %, respectively). The proportion of females, of patients in the first treatment for schizophrenia, with stable partner, living independently,
with paid employment, engaged in social activities, or starting treatment with olanzapine, risperidone, clozapine or oral typical antipsychotics were greater among patients who showed remission at some time than those who did not. Furthermore, the duration of the illness was shorter and the scores of the CGI-SCH scales lower in the group of patients that showed remission (table 2 and fig. 1).
100%
80% Proportion of patients
60%
40%
20%
0% 2+ antipsychotics 2+ antipsychotics Oral typing Oral typing Quetiapine Olanzapine Quetiapine Typical depots Typical depots Olanzapine Clozapine Risperidone Risperidone Clozapine
Remission (n = 1,366)
Relapse (n = 1,018)
Figure 1 Distribution of the unadjusted relative frequencies of patients that met criteria of remission and relapse throughout the 3 year follow-up by treatment cohort. The error bars indicate the corresponding 95% confidence intervals.
190 Actas Esp Psiquiatr 2008;36(4):187-196
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
The adjusted analyses (fig. 2) revealed that the likelihood of remission was significantly lower in patients who started treatment with an oral typical antipsychotic drug or with two or more antipsychotics than those who began treatment with olanzapine (respective p-values: 0.0104 and < 0.0001). Similarly, male patients and patients who were prescribed concomitant anxiolytics had less likelihood of remission (p-values: 0.0255 and 0.0060, respectively); while those who had participated in any social activity in the 4 weeks prior to their inclusion, had a paid employment, or who initiated treatment for their schizophrenia for the first time had greater likelihood of achieving remission during the follow-up (p-values: 0.0069, 0.0254 and 0.0069, respectively). Remission was also less likely between months 6 and 12, 12 and 18, or 18 and 24 than between months 30 and 36 (p-values: < 0.0001, < 0.0001 and 0.0030, respectively); as well as and for patients with higher (worse) cog-
nitive, negative or positive CGI-SCH scores or greater BMI at the initial visit (p-values: < 0.0001, < 0.0001, 0.0036 and <0.0001, respectively). The survival distribution functions of the time to remission by cohort (fig. 3 A) shows that it was shorter with olanzapine (solid line, below the remaining lines) than with other antipsychotics, followed by clozapine and oral typical antipsychotics. Patients initially prescribed multiple antipsychotic prescriptions had the longest time to remission.
Analysis of relapse
A total of 1,018 patients were included in this analysis. The patients were excluded from this analysis for the same
Table 2
Sociodemographical and clinical characteristics used in the analyses of remission, relapse and treatment maintenance. The values correspond to the baseline visit relevant to each analysis
Remission (n = 1,366) Yes (n = 821) No (n = 545) Relapse (n = 1,018) Yes (n = 190) No (n = 828)
Sociodemographical characteristics Gender: women (n [%])* Age at initial visit in years [mean (SD)] Body mass index in kg/m2 [mean [SD]) Clinical variables Time from first contact in years [mean (SD)] 9.97 (10.78) Age at first contact in years [mean (SD)] 27.74 (9.87) In the first episode in the initial visit [n (%)]* 91 (11.08) Patients without stable partner [n (%)]* 213 (26.13) Independent patients [n (%)]* 364 (44.50) Paid employment [n (%)]* 178 (21.68) Participation in social activities [n (%)]* 617 (75.52) Extrapyramidal symptoms [n (%)]* 281 (34.39) History of alcohol abuse [n (%)]* 23 (2.80) History of substance abuse [n (%)]* 31 (3.78) Concomitant anticholinergics (n (%)]* Concomitant antidepressants [n (%)]* 111 (13.52) Concomitant mood stabilizers [n (%)]* 44 (5.36) Decrease of libido observed [n (%)]* 319 (42.43) History of suicide attempt [n (%)]* 51 (6.21) Hostile behavior [n (%)]* Global baseline score CGI-SCH [mean (SD)] 4.34 (0.93) Positive symptoms score at baseline CGI-SCH [mean (SD)] 3.90 (1.32) Negative symptoms score at baseline CGI-SCH [mean (SD)] 3.90 (1.13) Depressive symptoms score at baseline CGI-SCH [mean (SD)] Cognitive symptoms score at baseline CGI-SCH [mean (SD)] 3.53 (1.17) EVA-EQ5D baseline score [mean (SD)] 49.33 (18.40) 13.81 (12.33) 26.59 (9.34) 22 (4.04) 103 (19.04) 187 (34.38) 51 (9.36) 330 (60.66) 250 (46.13) 26 (4.77) 18 (3.30) 99 (18.17) 45 (8.26) 237 (51.52) 26 (4.78) 4.81 (0.87) 4.21 (1.22) 4.65 (1.07) 19 (10.00) 2.83 (0.43) 51 (6.18) 2.79 (0.49) 9.03 (10.58) 26.74 (9.59) 16 (8.42) 52 (27.66) 83 (44.15) 45 (23.68) 158 (83.16) 35 (18.42) 6 (3.17) 12 (6.35) 36 (18.95) 10.72 (11.17) 27.74 (9.86) 84 (10.14) 222 (26.94) 367 (44.59) 196 (23.82) 711 (86.39) 116 (14.11) 19 (2.29) 22 (2.66) 74 (8.94) 338 (41.22) 25.83 (4.41) 175 (32.11) 27.39 (5.31) 78 (41.05) 26.61 (4.41) 326 (39.42) 26.83 (4.54)
51.80 (40.00)
4.33 (1.09) 71.26 (14.72)
67.89 (14.46)
*The relative frequencies have been calculated on the total of observations available in each variable, which, in some cases, was less than the total of the group (n)
Actas Esp Psiquiatr 2008;36(4):187-196
191
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
Lower probability of remission 0.55 0.93
Greater probability of remission
A
Two or more antipsychotics versus olanzapine Clozapine versus olanzapine
0.80 Typical depots versus olanzapine 0.64 Typical oral versus olanzapine 0.81 Quetiapine versus olanzapine 0.84 Risperidone versus olanzapine 0.75 Concomitant anxyolitics (yes versus no) 1.37 Social activities versus no activities 1.40 Paid employment versus no 1.72 0.79 0.77 (Higher/worse) cognitive symptoms score. CGI-SCH* 0.74 (Higher/worse) negative symptoms score CGI-SCH* 0.86 (Higher/worse) positive symptoms score CGI-SCH* 0.96 (Higher/worse) global score CGI-SCH* 0.95 (Higher) BMI* 0.99 Time (longest) from the first contact* 0 0.2 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8 2 2.2 2.4 2.6 2.8 First episode versus no first episode Male gender versus female
Odds ratio (remission versus non-remission) Lower probability of relapse 1.42 0.85 Clozapine versus olanzapine 1.09 Typical depot versus olanzapine 1.01 Typical oral versus olanzapine 2.13 Quetiapine versus olanzapine 0.95 2.00 Concomitant anticholinergic (yes versus no) 0.96 1.54 1.30 0.97 Male gender versus female Global score CGI -SCH (mild vs. normal) Global score CGI-SCH (bord. vs. normal) Time (longest) from the first contact* 1.2 1.6 2 2.4 2.8 3.2 3.6 4 4.4 Risperidone versus olanzapine Greater probability of relapse
B
Two or more antipsychotics versus olanzapine
0.4
0.8
Hazard ratio (relapse versus no relapse)
Figure 2 A) Odds ratios and 95% confidence intervals of the independent variables used in the multivariate logistic regression model of the likelihood of showing remission throughout the three-year follow-up period. B) hazard rates and 95% confidence intervals of the variables considered in the Cox proportional hazards model of time to relapse;
192 Actas Esp Psiquiatr 2008;36(4):187-196
10
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
Lower probability of hospitalization 0.91 1.64 1.39 1.87 1.04 2.52 2.20 2.05 1.99 1.25 1.17 1.01 0.98 0.98
Greater probability of hospitalization
C
Clozapine versus olanzapine Typical depot olanzapine Typical oral versus olanzapine Quetiapine versus olanzapine Risperidone versus olanzapine Appearance of galactorrhea versus no Appearance of gynecomastia versus no Concomitant mood stabilizers (yes versus no) Suicide attempts versus no attempts Male gender versus female (Higher/worse) cognitive symptoms score CGI-SCH* (Higher/worse) global score CGI-SCH* (Older) age Time (longest) since first contact*
0.4
0.8
1.2
1.6
2.4
2.8
3.2
3.6
4.4
4.9
5.2
5.6
Hazard ration (hospitalization versus no hospitalization)
Figure 2 C) Hazard ratios and 95% confidence intervals of the variables considered in the Cox proportional hazards model of time to hospitalization. The intervals lying entirely at the right of the dotted line indicate that the likelihood of remission (fig. A), relapse (fig. B) or hospitalization (fig. C) is significantly greater with the first option (exposed cases) than with the second one (unexposed cases) or with the change in the sense indicated in ordinal variables (marked with an asterisk) and vice versa.
reasons as for the analysis of remission, however, those patients who did not have an a score equal to or less than 3 at any time of follow-up were also not included since relapse can only be considered when there a previous favorable clinical state has existed. In all, 190 patients (18.7%) met the criteria for relapse. The sociodemographic and clinical characteristics at baseline (the first visit in which the patients had an overall CGI-SCH score equal or lower than 3) were similar between the groups of patients that relapsed and that did not relapse, with the exception of a greater proportion of substance abusers and concomitant need for anticholinergics among patients who relapsed (table 2). The adjusted analysis revealed that patients who started treatment with quetiapine had a significantly greater risk of relapse (or, in other words, that relapse occurred in a significantly shorter period) than those who started treatment with olanzapine (p-value: 0.0047). Similarly, patients who received concomitant anticholinergics were at significantly greater risk of relapse than those who did not (p-value: 0.0010). A marginally significant association between a longer duration of the illness with a lower risk of relapse was also found (p-value: 0.0470) (fig. 2 B).
11
The longest times to relapse corresponded to patients in the clozapine and risperidone cohorts, followed by patients in the olanzapine cohort (the upper lines in figure 3 B); while the shortest times were found among patients receiving two or more antipsychotics (fig. 3 B). On the other hand, the risk of being hospitalized (fig. 2 C) was greater in patients taking quetiapine than in those on olanzapine. A worse cognitive status at baseline, having a background of suicide attempts, concomitant prescription of mood-stabilizers or the occurrence of gynaecomastia and galactorrhoea were all associated with a greater risk of relapse. Conversely, the risk decreased with age and the duration of the disease; although the respective point estimates of the latter two factors were close to the unity (fig. 2 C).
DISCUSSION
The SOHO study is a large, three-year long European study on antipsychotic treatment in out-patients. Its observational design makes it possible to analyze the evolution of
193
Actas Esp Psiquiatr 2008;36(4):187-196
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
1 0.9 0.8 0.7
1 0.9 0.8 0.7
Survival distribution function
0.6 0.5 0.4 0.3 0.2 0.1 0 0 6 12 18 24 30 36 Time to remission in months (the circles represent censured data)
Survival distribution function
0.6 0.5 0.4 0.3 0.2 0.1 0 0 6 12 18 24 30 36 Time to relapse in months (the circles represent censured data) Risperidone Quetiapine Typical oral Tpicos depot Clozapine Two or more antipsychotics Olanzapine
Risperidone Quetiapine Typical oral Tpicos depot Clozapine Two or more antipsychotics Olanzapine
Figure 3 A) Survival distribution function of the time to remission by treatment cohort. B) Survival distribution function of time to relapse by treatment cohort. The circles indicate censored data (patients who finished follow-up without remitting [fig. A] or without relapse [fig. b]).
the disorder in the routine clinical practice and its size has helped to used complex statistical techniques to study the evolution predictors. The clinical remission and relapse, analyzed in the present work, is one of the most relevant results for the patient's well-being. The factors associated to a lower likelihood of remission were greater baseline clinical severity, worse social functioning, greater disease evolution time, and the use of a concomitant treatment with anxiolytics, also probably associated a greater clinical severity16. These results reinforce previous studies that indicate the good prognosis associated to good social functioning17 and the tendency of schizophrenia to have lower likelihood of improvement as the disorder evolves18. We have also observed that the likelihood of remission increases with time of treatment after a relapse and that the likelihood of relapse is also maintained even years after the remission. This fact reinforces the notion of the importance of continued treatment to improve the outcomes. The inverse association found between body mass index at baseline and the likelihood of remission may be related to differences in prescription habits, due to the tendency of the participating psychiatrists to prescribe olanzapine in thinner subjects (see complete description of baseline characteristics in the reference15) and the likeli194
hood of remission was greater among patients who initiated treatment with this drug. Consistent with results obtained in both randomized clinical trials19,20 and naturalistic studies21, the clinical evolution, measured as likelihood of remission, has been better in patients who initiated olanzapine in the baseline visit compared to those who used typical antipsychotics. However, other reviews did not find the same results22,23. It is likely that factors such as treatment compliance grade, its maintenance and profile of side effects in addition to the intrinsic antipsychotic efficacy of the drug, influence the long-term clinical efficacy of olanzapine versus typical antipsychotics. These aspects are not generally adequately assessed in the clinical trials. In this sense, the SOHO study shares some of these characteristics with the clinical trial on antipsychotic efficacy of several interventions (Clinical Antipsychotic Trial of Intervention Effectiveness [CATIE]), in which greater improvement and longer time of discontinuation with olanzapine than with other atypical antipsychotics has been demonstrated24. The 18.7 % incidence of relapse found in our analysis is much lower than what had been reported in previous studies25. The finding may be because the appearance of relapses was only evaluated at discrete time points in the control
12
Actas Esp Psiquiatr 2008;36(4):187-196
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
visits made every 6 months, determining the possibility of compliance of relapse criteria between visits only in the cases in which there was a hospitalization. Furthermore, it is likely that the participating psychiatrists, because this was a three-year follow-up study, tended to include patients who complied with the study treatment. Among all the factors considered, only treatment with quetiapine compared to olanzapine and the need for concomitant treatment with anticholinergics showed sufficient predictive capacity to explain future relapses. The concomitant treatment with anticholinergic may be associated to the use of antipsychotics that cause side effects, which in turn are generally associated to worse therapeutic compliance26. It is not surprising that patients with suicide attempts have a greater risk of being hospitalized. Because the risk was also greater in patients requiring concomitant mood stabilizers, affective symptoms appear as an important factor influencing in the need for admissions. The increased risk in patients with a worse cognitive status is also important. Taken together, these data suggest that once we have achieved an effective control of psychotic symptoms with continued effective therapy, the target to reduce in-hospital stay should be the cognitive and affective impairments of these patients. The SOHO study has some general limitations that affect the analysis of remission and relapse. In the first place, the non-randomized allocation has been already mentioned. However, the use of multivariate statistical techniques that take into account the baseline differences among patient who initiate different treatments has been shown as valid to control this bias27. However, there is no assurance that all the factors that may influence the outcome have been considered, as the cohorts may be also imbalanced by other unmeasured parameters. Furthermore, the small number of patients in some subgroups (as is the case of the cohorts of patients with polytherapy or treated with clozapine) may compromise the robustness of estimations made by regression analysis with these treatments. The presence of information biases also cannot be ruled out, as participating psychiatrists were obviously not blinded to the treatment the patients received. Nevertheless, an attempt was made to reduce the influence of this bias in the design stage. This was done by procuring as much flexibility as possible in the patients' treatment and thus avoiding interference with the routine clinical practice. In fact, a specific assessment made on such effects could not demonstrate the existence of observer biases in the SOHO study27. It is also possible that there was a tendency of the participating psychiatrists to keep patients in the study as long as possible by delivering some extra efforts because of economic incentives calculated on the basis of study visits reported. Consequently, the presence of a selection bias cannot be ruled out, as cases having worse prognosis were eliminated from the study in benefit with the less severe patients. In conclusion, the data presented here are relevant because they come from a considerably large sample of almost
13
2000 patients with schizophrenia followed-up for as long as three years within Spain in the frame of an observational prospective clinical study. Patients who require change of antipsychotic treatment for clinical reasons may benefit from substantial improvements in terms of high remission and low relapse rates. Because of the long-term favorable outcomes, olanzapine has been shown to be of great value in routine clinical practice.
ACKNOWLEDGEMENTS
This study has been financed by Eli Lilly and Company Limited, S.A.
REFERENCES 1. Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. American Psychiatric Association. Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 2004;161(2 Suppl.):1-56 2. National Institute for Clinical Excellence (NICE). Technology appraisal. Guidance No. 43. Guidance on the use of newer (atypical) antipsychotic drugs for the treatment of schizophrenia. London: NICE; 2002. Available online at www.nice.org.uk/pdf/ antipsychoticfinalguidance.pdf. Last accessed: 4 May 2006. 3. Treatment of schizophrenia 1999. The expert consensus guideline series J Clin Psychiatry 1999;60(Suppl. 11):3-80. 4. Haro JM, Edgell ET, Jones PB, Alonso J, Gavart S, Gregor KJ, et al., SOHO Study Group. The European Schizophrenia Outpatient Health Outcomes (SOHO) study: rationale, methods and recruitment Acta Psychiatr Scand 2003;107:222-32. 5. Gilbody S, Wahlbeck K, Adams C. Randomized controlled trials in schizophrenia: a critical perspective on the literature. Acta Psychiatr Scand 2002;105:243-51. 6. Kasper S, Rosillon D, Duchesne I; RODOS Investigator Group. Risperidone olanzapine drug outcomes studies in schizophrenia (RODOS): efficacy and tolerability results of an international naturalistic study. Int Clin Psychopharmacol 2001;16:179-87. 7. Ho BC, Miller D, Nopoulos P, Andreasen NC. A comparative effectiveness study of risperidone and olanzapine in the treatment of schizophrenia. J Clin Psychiatry 1999;60:658-63. 8. Dossenbach MR, Kratky P, Schneidman M, Grundy SL, Metcalfe S, Tollefson GD, et al. Evidence for the effectiveness of olanzapine among patients nonresponsive and/or intolerant to risperidone J Clin Psychiatry 2001;62(Suppl. 2):28-34. 9. Coley KC, Carter CS, DaPos SV, Maxwell R, Wilson JW, Branch RA. Effectiveness of antipsychotic therapy in a naturalistic setting: a comparison between risperidone, perphenazine, and haloperidol. J Clin Psychiatry 1999;60:850-6. 10. Bobes J, Gutirrez M, Gibert J, Gonzalez MP, Herraiz ML. Calidad de vida y discapacidad en pacientes esquizofrnicos crnicos en tratamiento con risperidona y previamente tratados con neurolpticos depot. Actas Esp Psiquiatr 1999;27:229-34. 11. Gmez JC, Sacristn JA, Hernndez J, Breier A, Ruiz Carrasco P, Anton Saiz C, et al. The safety of olanzapine compared with
195
Actas Esp Psiquiatr 2008;36(4):187-196
J. M. Haro, et al.
Remission and relapse in the ambulatory treatment of patients with schizophrenia. Outcomes at 3 years
12.
13.
14.
15.
16.
17.
18. 19.
other antipsychotic drugs: results of an observational prospective study in patients with schizophrenia (EFESO Study). Pharmacoepidemiologic Study of Olanzapine in Schizophrenia. J Clin Psychiatry 2000;61:335-43. Lieberman JA, Perkins D, Belger A, Chakos M, Jarskog F, Boteva K, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches Biol Psychiatry 2001;50:884-97. Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 2005;162:441-9. Haro JM, Kamath SA, Ochoa S, Novick D, Rele K, Fargas A, et al, on behalf of the SOHO Study Group. The Clinical Global ImpressionSchizophrenia scale: a simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatr Scand 2003;107(Suppl. 416):16-23. Ciudad A, Prieto L, Olivares JM, Montejo AL, Ros S, Novick D, and the Spanish SOHO Study Group. Estudio observacional paneuropeo de la efectividad de la olanzapina frente a otros antipsicticos (SOHO): resultados basales de la muestra espaola. Actas Esp Psiquiatr 2004;32:227-35. Brunette MF, Noordsy DL, Xie H. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv 2003;54:1395-401. Robinson DG, Woerner MG, McMeniman M. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry 2004;161:473-9. Huber G. The heterogeneous course of schizophrenia. Schizophr Res 1997;28:17785. Tollefson GD, Beasley CM Jr, Tran PV, Street JS, Krueger JA, Tamura RN, et al. Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform dis-
20.
21.
22.
23.
24.
25.
26.
27.
orders: results of an international collaborative trial. Am J Psychiatry 1997;154:457-65. Beasley CM Jr, Tollefson G, Tran P, Satterlee W, Sanger T, Hamilton S. Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial. Neuropsychopharmacology 1996;14:111-23. Rabinowitz J, Lichtenberg P, Kaplan Z, Mark M, Nahon D, Davidson M. Rehospitalization rates of chronically ill schizophrenic patients discharged on a regimen of risperidone, olanzapine, or conventional antipsychotics. Am J Psychiatry 2001;158:266-9. Geddes J, Freemantle N, Harrison P, Bebbington P. Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis BMJ 2000;321:1371-6. Leucht S, Wahlbeck K, Hamann J, Kissling W. New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003;361:1581-9. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al., Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23. Csernansky JG, Schuchart EK. Relapse and rehospitalisation rates in patients with schizophrenia: effects of second generation antipsychotics. CNS Drugs 2002;16:473-84. Karow A, Czekalla J, Dittmann RW, Schacht A, Wagner T, Lambert M, et al. Association of subjective well-being, symptoms, and side effects with compliance after 12 months of treatment in schizophrenia. J Clin Psychiatry 2007;68:75-80. Haro JM, Kontodimas S, Negrin MA, Ratcliffe M, Surez D, Windmeijer F. Methodological aspects in the assessment of treatment effects in observational health outcomes studies. Appl Health Econ Health Policy 2006;5:11-25.
196
Actas Esp Psiquiatr 2008;36(4):187-196
14
You might also like
- The Massachusetts General Hospital Guide to Depression: New Treatment Insights and OptionsFrom EverandThe Massachusetts General Hospital Guide to Depression: New Treatment Insights and OptionsBenjamin G. ShaperoNo ratings yet
- DemenciaDocument8 pagesDemenciajuby30No ratings yet
- Clinical StudyDocument5 pagesClinical StudyBruno Pedraz PetrozziNo ratings yet
- Rubio Valera2013Document10 pagesRubio Valera2013Marcus Fábio leite AndradeNo ratings yet
- Remission in Schizophrenia: One-Year Italian Prospective Study of Risperidone Long-Acting Injectable (RLAI) in Patients With Schizophrenia or Schizoaffective DisorderDocument11 pagesRemission in Schizophrenia: One-Year Italian Prospective Study of Risperidone Long-Acting Injectable (RLAI) in Patients With Schizophrenia or Schizoaffective Disorderdr.cintaNo ratings yet
- BMC Psychiatry: Non-Adherence To Antipsychotic Medication, Relapse and Rehospitalisation in Recent-Onset SchizophreniaDocument7 pagesBMC Psychiatry: Non-Adherence To Antipsychotic Medication, Relapse and Rehospitalisation in Recent-Onset SchizophreniaKamaruzzamanNo ratings yet
- Jurnal JiwaDocument6 pagesJurnal JiwaoldDEUSNo ratings yet
- Compliance With Aftercare Treatment Including Disulfiram and Effect On Outcome in Alcohol Dependent PaDocument7 pagesCompliance With Aftercare Treatment Including Disulfiram and Effect On Outcome in Alcohol Dependent PajpfundsNo ratings yet
- J Eurpsy 2007 03 002Document11 pagesJ Eurpsy 2007 03 002xhdrv7nvdrNo ratings yet
- The Effect of Motivational Interviewing On Medication Adherence and Hospitalization Rates in Nonadherent Patients With Multi-Episode SchizophreniaDocument10 pagesThe Effect of Motivational Interviewing On Medication Adherence and Hospitalization Rates in Nonadherent Patients With Multi-Episode SchizophreniaCarmen IoanaNo ratings yet
- The Treatment of SchizophreniaDocument9 pagesThe Treatment of Schizophreniaapi-542787928No ratings yet
- BarbuiDocument8 pagesBarbuirinaldiapt08No ratings yet
- Effects of Risperidone and Olanzapine Dose Reduction On Cognitive Function in Stable Patients With SchizophreniaDocument6 pagesEffects of Risperidone and Olanzapine Dose Reduction On Cognitive Function in Stable Patients With Schizophreniawen zhangNo ratings yet
- Example 2Document5 pagesExample 2Сергей СтанишевNo ratings yet
- Prevention of Recurrent Depression With Cognitive Behavioral TherapyDocument13 pagesPrevention of Recurrent Depression With Cognitive Behavioral TherapyImuzz Al GhassanNo ratings yet
- The Long-Term Effects of Antipsychotic Medication on 精神病病程Document9 pagesThe Long-Term Effects of Antipsychotic Medication on 精神病病程wen zhangNo ratings yet
- Comparison of Topiramate and Naltroxene For Treatment of Alcohol DependenceDocument8 pagesComparison of Topiramate and Naltroxene For Treatment of Alcohol Dependencejgwatson1979No ratings yet
- Evaluation of A Pharmaceutical Care Program For Hypertensive Patients in Rural PortugalDocument7 pagesEvaluation of A Pharmaceutical Care Program For Hypertensive Patients in Rural PortugalNOorulain HyderNo ratings yet
- Schizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapyDocument13 pagesSchizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapydilaNo ratings yet
- 9130Document13 pages9130BimaNo ratings yet
- Usr 6403928586398Document3 pagesUsr 6403928586398Rodrigo SosaNo ratings yet
- Hambleton Et Al Blue Print Study HandoutDocument3 pagesHambleton Et Al Blue Print Study Handoutlmnf717086No ratings yet
- Clozapine in Treatment of Schizophrenia: V. Burtea P. Ifteni A Teodorescu L. RogozeaDocument6 pagesClozapine in Treatment of Schizophrenia: V. Burtea P. Ifteni A Teodorescu L. RogozeaReza Badruun Syahrul HakimNo ratings yet
- Multiple Versus Single Antipsychotic Agents For Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus BenefitsDocument7 pagesMultiple Versus Single Antipsychotic Agents For Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus BenefitsPutri KeyshaNo ratings yet
- Alzrt 210Document15 pagesAlzrt 210avestusNo ratings yet
- Efficacy and Safety of Paliperidone Palmitate Eca ADocument14 pagesEfficacy and Safety of Paliperidone Palmitate Eca AMaria Fernanda AbrahamNo ratings yet
- The Role of CBT in Relapse Prevention of SchizophreniaDocument2 pagesThe Role of CBT in Relapse Prevention of SchizophreniaKorn IbraNo ratings yet
- Managing Antidepressant Discontinuation A Systematic ReviewDocument9 pagesManaging Antidepressant Discontinuation A Systematic ReviewAlejandro Arquillos ÁlvarezNo ratings yet
- Antipsychotic PolypharmacyDocument10 pagesAntipsychotic PolypharmacymarcoNo ratings yet
- Herrmann WM, Stephan K. Int Psychogeriatr. 1992 4 (1) :25-44.Document20 pagesHerrmann WM, Stephan K. Int Psychogeriatr. 1992 4 (1) :25-44.Ангелина СкоморохинаNo ratings yet
- Clinical Antipsychotic Trials of Intervention Effectiveness: (Catie)Document2 pagesClinical Antipsychotic Trials of Intervention Effectiveness: (Catie)vinodksahuNo ratings yet
- Alzheimer PicoDocument6 pagesAlzheimer PicoRaja Friska YulandaNo ratings yet
- Long-Term Follow-Up Ofthe Tips Early Detection in Psychosisstudy:Effectson 10-YearoutcomeDocument7 pagesLong-Term Follow-Up Ofthe Tips Early Detection in Psychosisstudy:Effectson 10-YearoutcomeELvine GunawanNo ratings yet
- Defining Treatment Response, Remission, Relapse, and RecoveryDocument21 pagesDefining Treatment Response, Remission, Relapse, and Recovery주병욱No ratings yet
- Good For QualitativeDocument9 pagesGood For QualitativeWassie TsehayNo ratings yet
- The TEPHRA Trial Is The First Study With The Primary Aim of Determining The Effects of Structured Aerobic Exercise and Physical Activity SelfDocument9 pagesThe TEPHRA Trial Is The First Study With The Primary Aim of Determining The Effects of Structured Aerobic Exercise and Physical Activity Selfach maskurNo ratings yet
- The Effects of Recreation Therapy On The Habit of Smoking and Positive-Negative Symptoms Among Patients With Chronic SchizophreniaDocument5 pagesThe Effects of Recreation Therapy On The Habit of Smoking and Positive-Negative Symptoms Among Patients With Chronic SchizophreniaTeodorNo ratings yet
- Resmume Jurnal JiwaDocument3 pagesResmume Jurnal Jiwaanj arNo ratings yet
- SchizoDocument4 pagesSchizoArlene Bonife MontallanaNo ratings yet
- Evaluation and Management of Treatment-Resistant Schizophrenia - UpToDateDocument16 pagesEvaluation and Management of Treatment-Resistant Schizophrenia - UpToDateJessica ChavesNo ratings yet
- Inggris IntervensionDocument8 pagesInggris IntervensionNasrudin JamilNo ratings yet
- Antipsychotic Augmentation vs. Monotherapy in Schizophrenia: Systematic Review, Meta-Analysis and Meta-Regression AnalysisDocument13 pagesAntipsychotic Augmentation vs. Monotherapy in Schizophrenia: Systematic Review, Meta-Analysis and Meta-Regression AnalysisvanfafiafiaNo ratings yet
- Antipsychotic Augmentation vs. Monotherapy in Schizophrenia: Systematic Review, Meta-Analysis and Meta-Regression AnalysisDocument13 pagesAntipsychotic Augmentation vs. Monotherapy in Schizophrenia: Systematic Review, Meta-Analysis and Meta-Regression AnalysisvanfafiafiaNo ratings yet
- Guía de Dosis de AntipsicóticosDocument8 pagesGuía de Dosis de AntipsicóticoskarlunchoNo ratings yet
- Behavioural Intervention For Dysphagia in Acute Stroke A Randomised Controlled Trial PDFDocument7 pagesBehavioural Intervention For Dysphagia in Acute Stroke A Randomised Controlled Trial PDFmichelle montesNo ratings yet
- Estudio CattieDocument18 pagesEstudio CattieMaría Alesia FernándezNo ratings yet
- Sap 28 195Document9 pagesSap 28 195IntanAgustiFernandesNo ratings yet
- Facilitated Pa-Depression-2Document13 pagesFacilitated Pa-Depression-2api-332791374No ratings yet
- Jurnal SkizoafektifDocument7 pagesJurnal SkizoafektifkhairinanurulNo ratings yet
- Quality of Life Is Predictive of Relapse in Schizophrenia: Researcharticle Open AccessDocument8 pagesQuality of Life Is Predictive of Relapse in Schizophrenia: Researcharticle Open AccessUMINAHNo ratings yet
- Journal of Schizophrenia ResearchDocument8 pagesJournal of Schizophrenia ResearchAustin Publishing GroupNo ratings yet
- Counselling Problem Drinkers in Medical Wards: Study: A ControlledDocument3 pagesCounselling Problem Drinkers in Medical Wards: Study: A ControlledIlyichia HuttonNo ratings yet
- Association Between Medication Adherence and Duration of Outpatient Treatment in Patients With SchizophreniaDocument7 pagesAssociation Between Medication Adherence and Duration of Outpatient Treatment in Patients With SchizophreniaazedaaNo ratings yet
- Research in Supportive Psychotherapy 1994Document9 pagesResearch in Supportive Psychotherapy 1994Elizabeth Paola CabreraNo ratings yet
- Paliperidona Revision 18 PagsDocument19 pagesPaliperidona Revision 18 PagsRodrigo SosaNo ratings yet
- BMC Psychiatry: Effectiveness of Second Generation Antipsychotics: A Systematic Review of Randomized TrialsDocument14 pagesBMC Psychiatry: Effectiveness of Second Generation Antipsychotics: A Systematic Review of Randomized Trialsyeontan onNo ratings yet
- Validation of The Short Form of The Hypertension Quality of Life Questionnaire (MINICHAL)Document35 pagesValidation of The Short Form of The Hypertension Quality of Life Questionnaire (MINICHAL)Adi SaputraNo ratings yet
- TreatmentResistantSchizophreniaReview CITROME Neuropsych2011Document23 pagesTreatmentResistantSchizophreniaReview CITROME Neuropsych2011Leslie CitromeNo ratings yet
- Farma - ArtDocument13 pagesFarma - ArtMaria Victoria Madariaga RevueltaNo ratings yet
- Starting An Intravenous Infusion Iv Insertion ChecklistDocument3 pagesStarting An Intravenous Infusion Iv Insertion ChecklistWeljoy LabbaoNo ratings yet
- Risk-Prone Health BehaviorDocument2 pagesRisk-Prone Health Behaviordragon3466100% (1)
- CHP Manual EN-webfinal PDFDocument29 pagesCHP Manual EN-webfinal PDFmajaklipaNo ratings yet
- NCP (Icu)Document2 pagesNCP (Icu)jessie_nuñez_263% (8)
- Brochure ECAICC 2024Document2 pagesBrochure ECAICC 2024أسعد حسنانNo ratings yet
- The Hiding Place, by John Burley - ExtractDocument13 pagesThe Hiding Place, by John Burley - ExtractAnonymous ikUR753am100% (1)
- Preserving The Ancestral Knowledge of Traditional Indigenous MidwivesDocument4 pagesPreserving The Ancestral Knowledge of Traditional Indigenous MidwivesCentro de Culturas Indígenas del PerúNo ratings yet
- Book Review: Available Online atDocument3 pagesBook Review: Available Online atFransiska DewiNo ratings yet
- International Journal of Surgery Open: Amir Forouzanfar, Jonathan Smith, Keith S. ChappleDocument3 pagesInternational Journal of Surgery Open: Amir Forouzanfar, Jonathan Smith, Keith S. ChappleSiti Fildzah NadhilahNo ratings yet
- BlindnessDocument26 pagesBlindnessdrmeenaxiNo ratings yet
- Tqip Poster 2016Document2 pagesTqip Poster 2016api-351340246No ratings yet
- Professional Development PlanDocument2 pagesProfessional Development Planapi-245887979100% (1)
- Patient Safety Is Our Top PriorityDocument14 pagesPatient Safety Is Our Top PriorityAlexandre SouzaNo ratings yet
- A Cup Otomo LogyDocument4 pagesA Cup Otomo LogyTumee DashNo ratings yet
- Nitin Thapar DataDocument4 pagesNitin Thapar DataRajat GuptaNo ratings yet
- Sudharani ResumeDocument3 pagesSudharani ResumeKranthi KumarNo ratings yet
- Health Project Management Final Indian Institute of Public Health DelhiDocument40 pagesHealth Project Management Final Indian Institute of Public Health DelhiKartavya Tiwari100% (2)
- Crisis Prevention Intervention Plan TrainingDocument8 pagesCrisis Prevention Intervention Plan TrainingSheila OdorNo ratings yet
- Asthma IhpDocument2 pagesAsthma Ihpapi-454842648No ratings yet
- Reading Sub-Test - Question Paper: Part A Text A Economy Class Syndrome Text C SymptomsDocument10 pagesReading Sub-Test - Question Paper: Part A Text A Economy Class Syndrome Text C SymptomsNaveen Abraham100% (1)
- Final Haldon Unit BrochureDocument16 pagesFinal Haldon Unit BrochureMarcin KlodaNo ratings yet
- Self Assesment Alat KesehetanDocument20 pagesSelf Assesment Alat KesehetanHariyadiAlldhiAchildNo ratings yet
- By: Jonalyn C. GalvezDocument60 pagesBy: Jonalyn C. GalvezvernaNo ratings yet
- Let's Talk About New Jobs : AnswersDocument3 pagesLet's Talk About New Jobs : AnswersosmarNo ratings yet
- Patient Safety and Clinical RiskDocument5 pagesPatient Safety and Clinical Riskshylajathomas33No ratings yet
- New Patient Registration Form TemplateDocument8 pagesNew Patient Registration Form TemplateHasfi YakobNo ratings yet
- Operating Room Surgical ProceduresDocument197 pagesOperating Room Surgical ProceduresChin Chan100% (6)
- Micro Labs Limited Planning For The FutureDocument11 pagesMicro Labs Limited Planning For The FutureHari ChandanaNo ratings yet
- Jurnal Dehydration of NewbornDocument7 pagesJurnal Dehydration of NewbornRSU Aisyiyah PadangNo ratings yet
- Doctor X.ep01.480p.x264 (D Addicts)Document54 pagesDoctor X.ep01.480p.x264 (D Addicts)an006No ratings yet