Professional Documents
Culture Documents
Community AcquiredPneumoniaDrug
Uploaded by
Katrine Jaya AndrewOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Community AcquiredPneumoniaDrug
Uploaded by
Katrine Jaya AndrewCopyright:
Available Formats
Subscription Information for
Community-Acquired Pneumonia Drug Resistance Patterns Prove Puzzling
Despite resistance in clinical isolates, treatment failures are rare, leading experts to ponder this seeming in vitro-in vivo paradox
David Holzman
ntibiotic resistance skyrocketed during the 1990s. In general, treatment failures and mortality rose in tandem with resistance. But not so in the case of macrolide resistance among isolates of Streptococcus pneumoniae and other bacterial agents that cause community-acquired pneumonia (CAP). This phenomenon can be called the in vitro-in vivo paradox, according to William Bishai of the Johns Hopkins University School of Public Health in Baltimore, Md. By this he means that drug resistance is measured in clinical isolates yet is not accompanied by an epidemic of treatment failures or a rise in mortality among those who are infected. Nonetheless, to some observers, the rising resistance in CAP portends disastrous levels of treatment failures to come if macrolides are not replaced in common clinical practice. The issue, which has taken up many journal pages of late, is critical. For one thing, macrolides are usually the best choice for treating CAP, being effective against the major culprits and the rarer etiologic agents, but sparing just about everything else. The second-choice alternative, the uoroquinolones, are broad-spectrum agents that act less discriminately against bacterial pathogens, potentially generating resistance among many of their scattershot targets. Certainly uoroquinolones are powerful but also resistance to these drugs remains relatively uncommon. Thus, they are highly valued, among other reasons because they sometimes serve as the antibiotics of last resort. Lately resistance to uoroquinolones also is edging up, worrying clinicians. Antibiotics are hard-to-replace resources, not to be squandered.
When do we say we have to switch to the newest agents? wonders infectious disease specialist Victor Yu of the University of Pittsburgh in Pittsburgh, Pa. Dispute over Apparent Rise of Resistance Before the 1990s, clinicians did not typically order susceptibility tests for cases involving pneumococcal pneumonias. That practice changed as antibiotic resistance proliferated. Currently, penicillin resistance in pneumococci is generally 30 50%, but may hover closer to 60% in some medical centers. For Streptococcus pneumoniae during 1999 2000, penicillin resistance averaged close to 35% among 33 centers, up from less than 5% during 1988 89, according to Bishai, who notes that it receded slightly in 20012002. And multidrug resistance now ranges from 24.0 36.6% in Haemophilus inuenzae, and soars to 86.2%96.8% in Moraxella catarrhalis. In the United States, macrolide resistance among pneumococci about doubled, to 20.4% between 1995 and 1999, as did the median minimum inhibitory concentration (MIC) for erythromycin in the less-resistant M phenotype strains, according to T. B. Hyde of the Centers for Disease Control and Prevention in Atlanta, Ga. Resistance is now present in 26% of S. pneumoniae isolates, according to Bishai and his colleague Eric Nuermberger at Johns Hopkins. John R. Lonks of Brown University Medical School directed a large, telltale study of human treatment failure due to macrolide-resistant S. pneumoniae in Providence, R.I. He and his colleagues interpret their ndings to mean that macrolides are failing to treat such infections
David Holzman writes from Lexington, Mass.
Volume 70, Number 12, 2004 / ASM News Y 571
among such patients and should no longer be used routinely. However, Bishai and others disagree with that conclusion, arguing that macrolides are continuing to work clinically and that in vitro test data are providing a misleading picture about the extent of macrolide resistance. Lonks case-control study included 86 patients who had macrolide-resistant pneumococcal bacteremia and were compared to 141 patients who had macrolidesusceptible pneumococcal bacteremia. These cases were culled for analysis from a set of 1,071 cases involving pneumococcal bacteremia patients who had stayed at one of three New England or one Spanish hospital during a period of about 13 years beginning in the late 1980s. Nineteen of the eighty-six case patients with frankly macrolide-resistant or intermediately resistant S. pneumoniae were being treated with a macrolide antibiotic versus none of the 141 control patients (P 0.00000004). This strong correlation leaves little doubt that the treatment failures occurred because patients receiving macrolide therapy were infected with macrolide-resistant S. pneumoniae. Moreover, 63% of the 19 cases of breakthrough bacteremia due to macrolide susceptibility occurred during the most recent three years of the study interval, Lonks further notes. This nding parallels the increasing prevalence of macrolide resistance. . . Lonks and his colleagues conclude that it makes sense to use high-dose, orally administered amoxicillin on outpatients with mild to moderate community-acquired pneumonia, while reserving macrolides for treating patients belonging to selected high-risk populations infected with atypical pathogens. However, where Lonks sees pneumonia treatment failures with macrolides looming on the horizon, Bishai sees continuing efcacy despite rising resistance among clinical isolates. The fact that so few patients with resistant disease were found among so many over so many years . . .is a testament to the effectiveness of macrolides in the management of pneumococcal pneumonia, he notes. Moreover, no deaths occurred among the patients from whom macrolide-resistant isolates were obtained, while among 67 patients with macrolide-resistant bacteria who did not receive a macrolide, the mortality rate was 18%. That is not the end of the story, according to Lonks. The difference in mortality rates was not statistically signicant (P .0605). Furthermore, he notes, the case patients who received
macrolides were younger than those who did not receive macrolides (mean age, 40 versus 55 years). Age, independent of antibiotic treatment received, is a very important predictor of mortality. . . Regarding the small number of cases of treatment failure due to macrolide resistance, the cases described are the tip of an iceberg. However, Yu asserts that in Pittsburgh at least, treatment failures are exceptionally rare. It would take a huge study to nd a lot of treatment failures, according to Keith Klugman of the Rollins School of Public Health at Emory University in Atlanta, Ga. If you look at the population of patients treated with macrolides alone, or at least those that ought to be treated with macrolides alone, bacteremia is very rare probably less than 1%, he says. Then you have to look at the fraction of those in whom a resistant organism might be found. If 10% of the 1% might be resistant, you are now looking for one in 1,000 patients, and then the patient has to have had a repeat blood culture, or a blood culture taken because they are not responding, so this is going to be a very rare event. Why Macrolide Resistance Might Not Prove Clinically Signicant Proponents of continuing to treat pneumococcal pneumonias with macrolides offer other evidence and rationales to support the notion that resistance to these antibiotics has not reached critical levels. One argument invokes a difference in mechanism between resistance that is clinically significant and that which is not. Macrolide resistance typically involves either an efux mechanism that works like a pump to bail the drug from the bacterial cell, involving the M phenotype and the mef gene, or a mechanism that disables the drug, involving the erm gene. Of the two, efux resistance is relatively weak. Most resistance in the United States is of the former variety, while the latter is more common in Europe. Resistance is measured in terms of minimum inhibitory concentration (MIC). Any S. pneumoniae that can survive serum concentrations of more than 0.5 g of macrolide per milliliter is considered to be fully resistant, while those eliminated by less than 0.25 g/ml are considered to be fully susceptible. Those numbers are considered the breakpoints for resistance and susceptibility. According to Gary V. Doern, of the
572 Y ASM News / Volume 70, Number 12, 2004
University of Iowa in Iowa City, 91% of efuxpositive isolates in the United States have erythromycin MICs of 8 g/ml or less. But erm resistance is powerful, with MICs usually exceeding 64 g/ml in serum, and often in the low hundreds. Bishai says that efux resistance is probably not of concern from a clinical standpoint, and he notes that in the Lonks study, only ve case patients had breakthrough bacteremia due to M phenotype strains . . . strong evidence that efux-mediated resistance among pneumococci is not clinically meaningful. Are MICs Relevant? The possibility that in CAP, MICs are being measured in the wrong place further undercuts the meaning of the currently accepted breakpoint values. The relevant concentration may be that at the site of infection, rather than in the serum. There is evidence that in CAP, ordinary doses of macrolides may drive site-of-infection concentrations well beyond ofcial MICs. Biomedical scientists are not certain exactly where the pathogens lodge in CAP, but there is some current thinking that in community-acquired pneumonia, the infection resides in the endothelial lining of the respiratory tract [ELF], the uid that lines the epithelium in the lungs, says Larry Danziger of the University of Illinois, Chicago. If you can get adequate concentration of your drug there, perhaps you can relate that to outcomes. We know the drug concentrates to a great extent in the ELF, as well as in the macrophages. Macrolides can reach a 10-fold-higher concentration in the ELF than in the serum, Danziger adds, citing studies of healthy volunteers conducted by his colleague Keith Rodvold. Although extrapolating from healthy to infected individuals involves some uncertainty, such ndings at least provide a rationale for expecting better outcomes than MICs alone might predict. One would expect patients to have signicantly higher concentrations of the drug in their ELF than healthy volunteers, Rodvold says, because patients usually eliminate drugs more slowly than do healthy individuals, especially drugs that are excreted by the kidneys. Because of ethical constraints, however, conducting experiments to determine levels of antibiotic in ELF among patients with pneumonias
remains an impossible undertaking. Another question involves the relationship between concentration and activity of antibiotics being used clinically, says Rodvold. There is no reason to think that [higher concentration would not improve efcacy in the ELF] but we have no evidence-based medicine to prove that it really does. For example, how might the environment inside the ELF affect the activity of a particular antibiotic being used? Conceivably, tissue-associated proteins might somehow deactivate drug molecules or other factors might concentrate them and make them more effective than expected. Whatever the mechanism, clinical success or failure may turn on differences in drug concentrations at the site of infection, says David Nicolau of Hartford Hospital and the University of Connecticut, Storrs. According to his own studies, clarithromycin concentrates more heavily than azithromycin in the ELF. The general health of patients also inuences their battles with pneumonia. Some individuals have such robust immune systems that they can defeat CAP without help from antibiotics. This general impression is reinforced by animal studies. For example, immunocompetent animals require three- to vefold less in the way of antibiotics than do comparable but immunocompromised animals to survive infections, according to Nicolau, who has conducted such studies. In other words, in vitro studies of pathogens cannot take into account white blood cells, complement, cytokines, all the host factors that are important in determining whether people get better or dont get better, Doern says. Immunomodulatory and Other Effects of Macrolides and Macrolide Resistance Another factor that complicates and undermines the predictive value of MICs is the growing evidence that macrolides are more than mere antibiotics. Thus, in addition to having direct antibacterial activity and perhaps also blocking biolm formation, they also act on the host in several wayssuppressing inammation and thinning mucus secretions. Further, clinicians at cystic brosis (CF) centers prescribe them routinely to inhibit inammation responses among CF patients, Bishai says. Thus, although macrolides are not effective against Pseudomonas aeruginosa, a gram-negative species that chron-
Volume 70, Number 12, 2004 / ASM News Y 573
ically infects the lungs of many CF patients, these drugs are effective in relieving symptoms associated with such infections. All this translates into measurable improvement for CF patients, says Bishai. In one uncontrolled study, seven patients who were treated with 500 mg of clarithromycin for six weeks showed a 14% increase in forced expiratory volume, and a 6% increase in forced vital capacity, as well as an increased number of sputum neutrophils. Other studies suggest that clarithromycin has similar activity in bacterial sinusitis, he adds. Such ndings support the notion that macrolides are helping CAP patients not only by knocking out the bacterial pathogen but also by mitigating other symptoms associated with those infections. Moreover, resistance itself might sap energy from these pathogens, thereby reducing virulence, Nicolau says. A Moving Target All this points to an unsettling thought. Legitimate in vitro experiments that measure MICs may only approximate and perhaps even misrepresent key features of in vivo infections. The predictive value of antibiotic testing in the lab [is poor], says Doern. More importantly, resistance is a moving target, and there are institutional obstacles to keeping up with it. Since 1965, the National Committee for Clinical Laboratory Standards (NCCLS), a globally recognized organization, has issued values for MICs, including estimates for acceptable antibiotic resistance levels. This process involves not only science but also art and sometimes politics as well, says Doern, who served with NCCLS for nearly a decade. The committee typically includes 12 members and additional advisors when it meets. But virtually anyone may attend its open meetings. Everyone has a voice if they want to be heard, he says. All they have to do is raise their hand. There is often a tug of war between committee members and laboratory professionals, according to Doern. For example, the setting of breakpoint values, which are numbers used to describe the boundaries between resistance and susceptibility for a particular pathogen, are mostly not disease specic. The laboratorians are reluctant to embrace disease-specic break-
points... because of the reporting confusion they would create in laboratories given the current fairly rudimentary laboratory information systems in use, he says. Committee members also often try to walk a tightrope when setting such values. If resistances are dened too conservatively, they are useless, but too-liberal breakpoints might lead to treatment failures as clinicians prescribe antibiotics that the pathogens resist. The overarching principal is, when in doubt, dene conservatively, Doern says. You would rather err by calling something falsely resistant, encouraging the use of some other antibiotic. IDSA Guidelines Still Favor Macrolides NCCLS breakpoint values for macrolides notwithstanding, the Infectious Diseases Society of America (IDSA) still considers macrolides to be safe for use in North American patients with CPA, according to IDSA chairman Lionel A. Mandell. They are actually prescribed for a large percentage of outpatients, and are an option for some inpatients as well, he says. They are rst-line treatment for outpatients who are otherwise well and have no complicating factors. Macrolides have been used since about 1951. If you add up all the case reports, there are maybe 50-60-70 failures, versus I dont know how many millions and millions of cures. One alternative for use in treating patients with CAP is telithromycin, a member of the new class of antibiotics, the ketolides, that was made available in the United States last April. Meanwhile, however, resistance troubles appear to be brewing for uoroquinolones, which are a widely used class of antibiotics, including to treat patients with CAP. The hottest topic in infectious diseases now is that we have quinolone resistance, says Pittsburghs Yu. In S. pneumoniae it rose from 0.9% in 1988 89 to 3.4% in 20012002 in the United States. And relatively high resistance to the uoroquinolone, ciprooxacin, is showing up in Spain. That suggests to us that the CDCs recommendations of reserving uoroquinolones for difcult cases is warranted, Bishai says. With antibiotics, you use it and you lose it, Yu says, adding: We dont have to lose [quinolones] right now.
574 Y ASM News / Volume 70, Number 12, 2004
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Write 55g As A Percentage of 2.2kgDocument8 pagesWrite 55g As A Percentage of 2.2kgKatrine Jaya AndrewNo ratings yet
- A Train Leaves Zurich at 2240 and Arrives in Vienna at 0732 The Next Day. Work Out The Time TakenDocument11 pagesA Train Leaves Zurich at 2240 and Arrives in Vienna at 0732 The Next Day. Work Out The Time TakenKatrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.5 Forces (Part 2) - Worksheet - Paper 2Document7 pages1 General Physics - 1.5 Forces (Part 2) - Worksheet - Paper 2Katrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.2 MotionDocument5 pages1 General Physics - 1.2 MotionKatrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.1 Length and TimeDocument11 pages1 General Physics - 1.1 Length and TimeKatrine Jaya AndrewNo ratings yet
- A Train Leaves Zurich at 2240 and Arrives in Vienna at 0732 The Next Day. Work Out The Time TakenDocument11 pagesA Train Leaves Zurich at 2240 and Arrives in Vienna at 0732 The Next Day. Work Out The Time TakenKatrine Jaya AndrewNo ratings yet
- RatioDocument13 pagesRatioKatrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.5 Forces (Part 1)Document16 pages1 General Physics - 1.5 Forces (Part 1)Katrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.2 MotionDocument5 pages1 General Physics - 1.2 MotionKatrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.1 Length and TimeDocument11 pages1 General Physics - 1.1 Length and TimeKatrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.3 Mass and Weight - Paper 4Document10 pages1 General Physics - 1.3 Mass and Weight - Paper 4Katrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.2 Motion - Worksheet - Paper 4Document12 pages1 General Physics - 1.2 Motion - Worksheet - Paper 4Katrine Jaya AndrewNo ratings yet
- 1 General Physics - 1.3 Mass and WeightDocument10 pages1 General Physics - 1.3 Mass and WeightKatrine Jaya AndrewNo ratings yet
- 1 General Physics - Topic Assessment 1Document6 pages1 General Physics - Topic Assessment 1Katrine Jaya AndrewNo ratings yet
- Density (Multiple Choice) QPDocument15 pagesDensity (Multiple Choice) QPChong Xue Er100% (1)
- 1 General Physics - Topic Assessment 1Document6 pages1 General Physics - Topic Assessment 1Katrine Jaya AndrewNo ratings yet
- 1 General PhysicsDocument37 pages1 General PhysicsKatrine Jaya Andrew100% (1)
- TIPSDocument12 pagesTIPSKatrine Jaya AndrewNo ratings yet
- Plants and KS3 Science: Planting Ideas and Helping Them GrowDocument8 pagesPlants and KS3 Science: Planting Ideas and Helping Them GrowKatrine Jaya AndrewNo ratings yet
- 0580 s19 Ms 42 PDFDocument9 pages0580 s19 Ms 42 PDFKatrine Jaya AndrewNo ratings yet
- TIPSDocument12 pagesTIPSKatrine Jaya AndrewNo ratings yet
- Number IGCSE MathsDocument28 pagesNumber IGCSE MathsKatrine Jaya AndrewNo ratings yet
- Student Seminar Booklet Paper 6Document45 pagesStudent Seminar Booklet Paper 6Katrine Jaya AndrewNo ratings yet
- 07 Human Transport Biology Notes IGCSE 2014 PDFDocument27 pages07 Human Transport Biology Notes IGCSE 2014 PDFJohn DeHans100% (2)
- May-June 2016 Paper 6Document12 pagesMay-June 2016 Paper 6EmanNo ratings yet
- Tips For Chemistry Paper 2Document5 pagesTips For Chemistry Paper 2Katrine Jaya AndrewNo ratings yet
- Electricity & Magnetism Paper 6Document6 pagesElectricity & Magnetism Paper 6Katrine Jaya AndrewNo ratings yet
- Electricity & Magnetism Paper 6Document12 pagesElectricity & Magnetism Paper 6Katrine Jaya AndrewNo ratings yet
- Cambridge International Examinations Cambridge International General Certificate of Secondary EducationDocument6 pagesCambridge International Examinations Cambridge International General Certificate of Secondary EducationImmy MaysmeekaNo ratings yet
- Physics Checkpoint QuestionsDocument5 pagesPhysics Checkpoint QuestionsKatrine Jaya AndrewNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Universal Health Coverage Ambition Faces A Critical Test.Document2 pagesThe Universal Health Coverage Ambition Faces A Critical Test.Brianna Vivian Rojas TimanaNo ratings yet
- Control of Microorganisms - Sterilization and Disinfection.Document27 pagesControl of Microorganisms - Sterilization and Disinfection.manojbanNo ratings yet
- Iec DengueDocument3 pagesIec DengueKeith Wesley YbutNo ratings yet
- Manual MassageadorDocument5 pagesManual Massageadorjuliocarlossch100% (1)
- Manual of Travel Medicine & Health, 2nd Ed, 2003Document641 pagesManual of Travel Medicine & Health, 2nd Ed, 2003Alfan Bayu Firmansyah100% (2)
- Training For Hygiene Promotors and HP Coordinators. Part 1 of 3. Essential To KnowDocument176 pagesTraining For Hygiene Promotors and HP Coordinators. Part 1 of 3. Essential To KnowOswar Mungkasa100% (1)
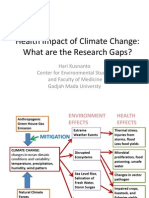
- 2 - Prof Hari Kusnanto - Climate Change and Impacts On Health in IndonesiaDocument12 pages2 - Prof Hari Kusnanto - Climate Change and Impacts On Health in IndonesiaMohammad Rahman HakimNo ratings yet
- Orthopaedic Surgery MCQsDocument23 pagesOrthopaedic Surgery MCQsWinifred Chen70% (10)
- Mal de Ojo (English)Document2 pagesMal de Ojo (English)Tim OrtizNo ratings yet
- Abdomen XrayDocument82 pagesAbdomen Xraypriyasureddi8004100% (2)
- Handbook of Disease Burdens and Quality of Life Measures - V. Preedy, R. Watson (Springer, 2010) WWDocument4,278 pagesHandbook of Disease Burdens and Quality of Life Measures - V. Preedy, R. Watson (Springer, 2010) WWRiska Indriani100% (1)
- CHN ExamDocument21 pagesCHN ExamExemplar ReviewNo ratings yet
- Breast Self-Examination: Knowledge and Practice Among Nurses in United Arab EmiratesDocument4 pagesBreast Self-Examination: Knowledge and Practice Among Nurses in United Arab EmiratesMuhammad AlfianNo ratings yet
- NanoviridaeDocument16 pagesNanoviridaeDeepak Singh SangwanNo ratings yet
- DCR 's-4 AprilDocument33 pagesDCR 's-4 AprilVidya BudihalNo ratings yet
- 4 Microorganisms QueDocument6 pages4 Microorganisms Querashmi_harryNo ratings yet
- Community Health Nursing Notes - Epidemiology, Health Policy, DisasterDocument16 pagesCommunity Health Nursing Notes - Epidemiology, Health Policy, DisasterKristen Ruehman100% (1)
- Diphtheria in NepalDocument30 pagesDiphtheria in NepalBinaya100% (1)
- Dyspepsia (Gastritis) Case StudiesDocument9 pagesDyspepsia (Gastritis) Case StudiesJessica Nurin Graman100% (1)
- 6bi04 Exam Paper SampleDocument20 pages6bi04 Exam Paper SampleAli AkramNo ratings yet
- Diare: Arlinda Silva Prameswari 201810401011044Document28 pagesDiare: Arlinda Silva Prameswari 201810401011044Lilian Rahma AnandaNo ratings yet
- Jurnal Case Report - Hemangioma KavernosaDocument12 pagesJurnal Case Report - Hemangioma KavernosaMaulida Ayu NorizaNo ratings yet
- National Nipah Virus Guideline BangladeshDocument77 pagesNational Nipah Virus Guideline BangladeshFaisol KabirNo ratings yet
- Introduction To Non Communicable DiseasesDocument35 pagesIntroduction To Non Communicable DiseasesNayyar Raza Kazmi100% (1)
- Guidelines For Use of The ILO Inernational Classification Od Radio Graphs of PneumoconiosesDocument57 pagesGuidelines For Use of The ILO Inernational Classification Od Radio Graphs of PneumoconiosesbumdinNo ratings yet
- Ectropion vs. EntropionDocument1 pageEctropion vs. EntropionAhmed ShafikNo ratings yet
- Prevention and Control of Soil-Transmitted Helminthiasis With Focus On DewormingDocument51 pagesPrevention and Control of Soil-Transmitted Helminthiasis With Focus On DewormingDaxw JlmiNo ratings yet
- Phobia ListDocument14 pagesPhobia Listkyle.smile2011No ratings yet
- Contact DermatitisDocument70 pagesContact DermatitisThariq Mubaraq DrcNo ratings yet
- Sentimental Medicine PDFDocument8 pagesSentimental Medicine PDF杨飞燕No ratings yet