Professional Documents
Culture Documents
Journal
Uploaded by
Riin IrasustaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal
Uploaded by
Riin IrasustaCopyright:
Available Formats
Izalyn N.
Irasusta
II-BSN
Ipsilateral ectopic pregnancy occurring in the stump of a previous ectopic site: a case report Bode-Law Faleyimu, Gabriel O Igberase and Mojeed O Momoh Cases Journal 2008 http://www.casesjournal.com/content/1/1/343 Abstract Background Ectopic pregnancy continues to be a significant cause of maternal morbidity, mortality and reproductive failure in Nigeria. Ipsilateral ectopic pregnancy occurs rarely and may be difficult to diagnose in low resource settings where there are no diagnostic tools. Few cases have been reported in the literature but none in our region. Case presentation We present an unusual case of a 22 year old female undergraduate, from the Urhobo tribe in the Niger Delta region of Nigeria who had a recurrent left ectopic pregnancy at the stump of a previous cornual resection done five years earlier. She had a left salpingo-oophorectomy done and did well postoperatively. Conclusion Ectopic pregnancy could pose a diagnostic dilemma where diagnostic facilities are not available. Every woman with a previous ectopic pregnancy would be at high risk for recurrence and that would be the condition to be ruled out if a pregnant woman presented at early gestation with abdominal pain. Background Ectopic pregnancy continues to be an important contributor to maternal mortality, morbidity and early fetal wastages in the first trimester of pregnancy [1]. The incidence of recurrent ectopic pregnancy is approximately 15% and this rises to 30% following two ectopic pregnancies [2]. A previous study on ectopic pregnancy done in the same region revealed an incidence of 3.5% of total hospital births [1]. Management of ectopic pregnancy has been improved upon by the use of ultrasound, laparoscopy and monitoring of beta subunit of human chorionic gonadtrophin[3]. In developed nations, treatment options have shifted from laparotomy to conservative surgical and non surgical techniques. Ectopic pregnancy could pose a diagnostic dilemma in centres where diagnostic facilities are lacking. We present an unusual case of left ipsilateral ectopic pregnancy occurring in the stump of a previous ectopic site following cornual resection. Case presentation We present the case of a 22 year old Para 0+2 female undergraduate from the Urhobo tribe in the Niger Delta region of Nigeria who was seen at the gynecological clinic with a two week history of colicky lower abdominal pain which became generalized a day prior to presentation. There was no history of dizziness or fainting spells. There were no gastrointestinal symptoms. She bled per vaginam two weeks prior to presentation for four days which she claimed to be her menses. There was no history of chronic cough or weight loss. She did not have any purulent vaginal discharge prior to bleeding per vagina. She had a previous left cornual resection for a ruptured ectopic pregnancy five years ago in this hospital. There was also a history of having been managed for sepsis following the termination of an eight week pregnancy four months prior to presentation.
Examination revealed that she was in painful distress and had mild pallor. Chest was clinically clear. Her pulse rate was 100 beats per minute while the blood pressure was 120/70 mmHg. Abdomen examination revealed a full, soft abdomen with tenderness in the suprapubic region, right and left iliac fossae, left renal angle and periumbilical area. Vaginal examination showed a normal lower genital tract, uterus was normal sized, anteverted, no pelvic masses were felt, pouch of Douglas was empty and there was marked cervical excitation tenderness. Differential diagnoses were those of left pyelonephritis, pelvic inflammatory disease and slow leaking ectopic pregnancy. Complete blood count and urinalysis was normal. Hemoglobin was 10.6 gm/dl. Serum beta human chorionic gonadotrophin was 3,500 mIU/mL. Screening for chlamydia and gonorrhoea were negative. Pelvic ultrasound scan revealed the presence of a left adnexal complex mass with associated free pelvic fluid and increased blood flow activity. The uterus shows a normal outline with slightly thickened endometrial plate and no intrauterine cyesis. Conclusion was left ectopic pregnancy. She was placed on a nil per os regimen and intravenous fluid was commenced. Two units of whole blood were grouped and cross-matched. A left salpingo-oophorectomy with pelvic adhesiolysis was done. Repeat Pfannenstiel incision through previous scar was made to enter the abdominal cavity. Findings at surgery were hemoperitoneum of 600 mls, left tubo-ovarian mass adherent to the pelvic floor (left chronic ectopic involving the tubal stump and the ovary with vesico-utero-ovarian adhesions), omento-uterine adhesions, cornual adhesions and stump, slightly bulky uterus, normal looking right ovary and a beaded right fallopian tube. The haemoperitoneum was sucked and adhesiolysis performed to free the omentum from behind the uterus. The left tubo-ovarian mass was lifted out and bluntly freed from the pelvic floor to define a near anatomy. A left salpingooophorectomy was performed and haemostasis was secured. Abdominal wall was closed with subcuticular dexon to skin. She was discharged on the fourth postoperative day. She was counseled on the use of contraception and the combined oral contraceptive was offered her. The possibility of repeat ectopic pregnancy was explained and she was counseled on safe sex. She was seen again two weeks later and was found to be stable. Histology report revealed a left tubal ectopic pregnancy and a left ovarian corpus luteum cyst. There was no evidence of genital tuberculosis. Discussion She had a previous cornual resection done and she still had a repeat episode on the stump of the same fallopian tube. There was no history of this patient being on any contraceptive method. There was also a positive history of septic abortion which is a risk factor for ectopic pregnancy. This, in combination with a history of previous ectopic, which is the most significant risk factor, favoured the setting for a repeat ectopic pregnancy [1,4]. The literature is replete with a lot of theories on the mechanism of recurrent ipsilateral ectopic pregnancy [5,6]. One theory explains that spermatozoa pass through the patent tube into the pouch of Douglas, then travel to fertilize the ovum on the side of the diseased tube. The fertilized ovum then implants on the stump of previous ectopic site. Another, is the theory of transperitoneal migration which says the fertilized ovum on the side of the normal tube migrates and gets implanted on the tubal stump. A third theory says despite ligation, lumina remain intact in the interstitial portion and distal remnant of the fallopian tube. This allows communication between the endometrial and peritoneal cavities and thus migration of the fertilized ovum or spermatozoa from the endometrial cavity to the distal remnant of fallopian tube. Ectopic pregnancy has been described as the great masquerader. Figure 1 shows left tubal ectopic gestation. What looked like her last menstrual period lasted for four days. This would have confused the picture more. However, she had abdominal pain which is the commonest presenting symptom. Can we say this girl was lucky? In a way, yes. She had the ectopic pregnancy on the same fallopian tube previously affected. She still has more than 80% chance of intrauterine conception if the contralateral tube is healthy. Unfortunately it appeared beaded macroscopically. However if the only viable tube is affected, she will be left only with the choice of assisted conception. The patient was
screened for Chlamydia, Gonorrhoea and genital tuberculosis. This rules out a pelvic inflammatory disease because of the possibility of recurrence and further complications. Tuberculosis is common in developing countries and with the presence of pelvic adhesions in this patient, is a good differential diagnosis. There was no history of chronic cough or weight loss. Genital tuberculosis was ruled out by histology. Figure 1. Showing the uterus (UT) and left tubal ectopic gestational sac (EGS). Salpingo-oophoorectomy was done in this case as the fallopian tubes and ovaries were bound in adhesions. Modern management involves the use of laparoscopy to perform salpingectomy and the conservative surgeries of salpingostomy and salpingotomy. Conclusion Ectopic pregnancy could pose a diagnostic dilemma where diagnostic facilities are not available. Every woman with a previous ectopic pregnancy would be at high risk for recurrence and that would be the condition to be ruled out if a pregnant woman presented at early gestation with abdominal pain. Reaction: Ectopic pregnancy is considered as a high risk factor in pregnancy. It is one of causes of bleeding in the first trimester. This is dangerous for the mother and there rare chance for the embryo turns into a live baby. Many complications can happen in this pregnancy, worse is that in can lead to death. A recurrent ectopic pregnancy is surely more dangerous. An early detection and management is a must for the safety of the mother and the embryo. One thing about this case was that the embryo implanted on the same site of previous pregnancy and she still have a chance to have intrauterine conception.
You might also like
- Preceptor GuidelinesUERM-RLE 2Document6 pagesPreceptor GuidelinesUERM-RLE 2Ron OpulenciaNo ratings yet
- Unedited Patho Hip FractureDocument1 pageUnedited Patho Hip FractureRiin IrasustaNo ratings yet
- Pterygium PresentationDocument16 pagesPterygium PresentationRiin IrasustaNo ratings yet
- AACN Synergy ModelDocument59 pagesAACN Synergy ModelRiin Irasusta100% (2)
- Machine Language: Advantage Machine LanguageDocument2 pagesMachine Language: Advantage Machine LanguageRiin IrasustaNo ratings yet
- A Case of Diabetic RetinopathyDocument29 pagesA Case of Diabetic RetinopathyRiin IrasustaNo ratings yet
- A Taxonomy For Disease Management: AHA Scientific StatementDocument15 pagesA Taxonomy For Disease Management: AHA Scientific StatementRiin IrasustaNo ratings yet
- Draft StressDocument6 pagesDraft StressRiin IrasustaNo ratings yet
- Chronic Disease ManagementDocument15 pagesChronic Disease ManagementRiin IrasustaNo ratings yet
- Description: Tags: CompneedsassessmentDocument27 pagesDescription: Tags: Compneedsassessmentanon-134896No ratings yet
- Employee Motivation & Performance ManagementDocument10 pagesEmployee Motivation & Performance ManagementRiin IrasustaNo ratings yet
- Jennifer AssignmetnDocument5 pagesJennifer AssignmetnRiin IrasustaNo ratings yet
- Bio Stat ChartDocument10 pagesBio Stat ChartRiin IrasustaNo ratings yet
- 1 Review of Anatomy and Physiology of Endocrine SystemDocument48 pages1 Review of Anatomy and Physiology of Endocrine SystemRiin Irasusta100% (1)
- Kanjibookjlptn5 PDFDocument111 pagesKanjibookjlptn5 PDFIleana ContrerasNo ratings yet
- Cannabis may be a risk factor for stroke in younger patientsDocument1 pageCannabis may be a risk factor for stroke in younger patientsRiin IrasustaNo ratings yet
- This Is!!!! KwinDocument65 pagesThis Is!!!! KwinRiin IrasustaNo ratings yet
- Working Through Moral Anguish BeneficienceDocument2 pagesWorking Through Moral Anguish BeneficienceRiin IrasustaNo ratings yet
- Drugpolar PDFDocument1 pageDrugpolar PDFRiin IrasustaNo ratings yet
- Most Shy Children Do Not Suffer From Social PhobiaDocument2 pagesMost Shy Children Do Not Suffer From Social PhobiaRiin IrasustaNo ratings yet
- Practice Test 1Document10 pagesPractice Test 1Riin IrasustaNo ratings yet
- Groupcase PresentationDocument18 pagesGroupcase PresentationRiin IrasustaNo ratings yet
- CannabisDocument2 pagesCannabisRiin IrasustaNo ratings yet
- Amphetamine AbuseDocument2 pagesAmphetamine AbuseRiin IrasustaNo ratings yet
- Benevolence InjusticeDocument5 pagesBenevolence InjusticeRiin IrasustaNo ratings yet
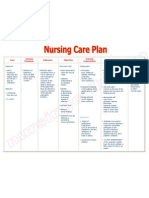
- Assessment Diagnosis Planning Intervention Rationale Evaluation IndependentDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation IndependentRiin IrasustaNo ratings yet
- BorderlineDocument3 pagesBorderlineRiin IrasustaNo ratings yet
- El PresidenteDocument2 pagesEl PresidenteRiin Irasusta0% (1)
- The Nurses Who Gossip About Patients On Facebook and How They Are Spying On Their Loved OnesDocument2 pagesThe Nurses Who Gossip About Patients On Facebook and How They Are Spying On Their Loved OnesRiin IrasustaNo ratings yet
- RRL Summary 1Document2 pagesRRL Summary 1Riin IrasustaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Critical Thinking Exercise NCM 106Document5 pagesCritical Thinking Exercise NCM 106Julienne Sanchez-SalazarNo ratings yet
- Nursing Care Plan Infection Bartholins Duct CystDocument1 pageNursing Care Plan Infection Bartholins Duct Cystderic100% (5)
- Urology Instrumentation A Comprehensive GiudeDocument185 pagesUrology Instrumentation A Comprehensive GiudeJade Kenneth Gonzales Lomansoc93% (15)
- Julia Rolla Nursing ResumeDocument2 pagesJulia Rolla Nursing Resumeapi-340271685No ratings yet
- 3rd Newsletter FinalDocument14 pages3rd Newsletter FinalBhavish RamroopNo ratings yet
- LEPROSYDocument55 pagesLEPROSYGeraldine Marie SalvoNo ratings yet
- CNPASDocument3 pagesCNPASaneeshNo ratings yet
- Learning Related Vision ProblemsDocument38 pagesLearning Related Vision Problemseva.benson100% (1)
- Chapter 12Document15 pagesChapter 12kk5522No ratings yet
- Initial Evaluation General InformationDocument7 pagesInitial Evaluation General InformationJoanna EdenNo ratings yet
- Jeevan Suraksha Hospital 1-2Document41 pagesJeevan Suraksha Hospital 1-2Prashansa AgrawalNo ratings yet
- Albumin: Pathophysiologic Basis of Its Role in The Treatment of Cirrhosis and Its ComplicationsDocument26 pagesAlbumin: Pathophysiologic Basis of Its Role in The Treatment of Cirrhosis and Its Complicationsravi rajNo ratings yet
- Morales-Roman ResumeDocument2 pagesMorales-Roman Resumeapi-301624882No ratings yet
- Malunion Delayed Union and Nonunion FracturesDocument31 pagesMalunion Delayed Union and Nonunion FracturesKalayo100% (1)
- Session 8 Rle - OdquierDocument18 pagesSession 8 Rle - OdquierAndrea Mae OdquierNo ratings yet
- Hyper Parathyroid IsmDocument7 pagesHyper Parathyroid IsmEllene Mae Dejapa VillasisNo ratings yet
- Nursing Assignments GuideDocument54 pagesNursing Assignments GuideEya CamillerNo ratings yet
- 1001 Arab Inventions WorksheetDocument4 pages1001 Arab Inventions WorksheetVictorNo ratings yet
- Clínica Oftalmológica Del Caribe (COFCA) ColombiaDocument11 pagesClínica Oftalmológica Del Caribe (COFCA) ColombiaJulio Martinez-ClarkNo ratings yet
- HeartBeat Magazine1 Oktober 2017 PDFDocument32 pagesHeartBeat Magazine1 Oktober 2017 PDFMr. KINGNo ratings yet
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-317390500No ratings yet
- HEAL 2013 RecommendationsDocument39 pagesHEAL 2013 RecommendationsDhawan SandeepNo ratings yet
- Nursing Care Plan Impaired AdjustmentDocument1 pageNursing Care Plan Impaired Adjustmentderic100% (2)
- Guiding Pharmacist Patient Interview ModelDocument25 pagesGuiding Pharmacist Patient Interview ModelHumera Sarwar100% (1)
- Angina: Angina:chest Pain Caused by Reduced Blood Flow To The Heart MuscleDocument11 pagesAngina: Angina:chest Pain Caused by Reduced Blood Flow To The Heart MuscleMohammed Falih HassanNo ratings yet
- Commercial Index - SV - CarlislecDocument308 pagesCommercial Index - SV - CarlislecRobert RangstanNo ratings yet
- Nursing Care Plan - SLHDocument4 pagesNursing Care Plan - SLHheartyprincess54No ratings yet
- Project of Shree Shivanand Mission Trust Hospital RajkotDocument22 pagesProject of Shree Shivanand Mission Trust Hospital RajkotDevvrat SukhwalNo ratings yet
- Debre Brehan University - Nursing Program Module.Document82 pagesDebre Brehan University - Nursing Program Module.Minlik-alew Dejenie100% (3)
- Diabetes PharmacologyDocument14 pagesDiabetes PharmacologyRich JeongNo ratings yet