Professional Documents
Culture Documents
Science of Living Systems: Bio-Thermal-Fluid Sciences: Lecture by Prof. Soumen Das
Uploaded by
himanshu_agraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Science of Living Systems: Bio-Thermal-Fluid Sciences: Lecture by Prof. Soumen Das
Uploaded by
himanshu_agraCopyright:
Available Formats
1
Science of Living Systems:
Bio-Thermal-Fluid Sciences
Lecture by
Prof. Soumen Das
School of Medical Science and Technology
Spring 2012
2
Fluid Shear Stress Schematic Depiction
3
The Flow Physics
Fully developed flow is non-accelerating:
Constant Also C; Constant each term Hence
only Y of function a is RHS as only where x of function a is LHS
: relations two Combining
flow) developed (fully 0 as
Fluid Newtonian Assume
0
0
) (
) (
) ( ) (
= = =
c
c
c
c
=
c
c
=
c
c
=
c
c
+
c
c
= =
=
c
c
+
c
c
=
c
c
+ +
c
c
+
t
t
t
t
t t
y
u
y x
p
v
y
u
y
u
x
v
y x
p
dx dy
y
dx dy dx
x
p
p pdy
4
The Flow Physics
Number Reynolds Re where
Re )
6
(
6
6
)
12
(
2 2
0
: Stress Shear Wall
12
) 6 / (
2
1
0
1
u : velocity Average
Flow Poiseuille ) (
2
1
) (
0
0 0
: conditions boundary with ) ( g Integratin
2
2
2
2
2
avg
2
= =
= =
= = =
=
=
=
=
}
=
=
= =
= =
c
c
c
c
=
c
c
t
t
H u
H H
H u
H
H
u
H
u
H
dx
dp H
y
dy
du
H
u
dx
dp
H
H
dx
dp
H
udy
H
Hy y
dx
dp
y u
H y at u
y at u
y
u
y x
p
avg
avg
w
avg avg
w
avg
5
Major Differences in Transport Phenomena in
Engineering and Physiology
Wide Range of Reynolds Number:
Majority of flow in physiological system is laminar
High and low Reynolds number laminar regime
High Re: Large Arteries and airways in lungs
Low Re: Small capillaries and Interstitial Flow
There are localized bursts of turbulence as well
Artery: Blood vessels that carry blood away from the heart into the tissue.
This blood is normally oxygenated.
Interstitial Flow: Percolating fluid flow through a 3D tissue spaces, around
embedded cells. IF drains out of blood vessels
Local vortices at bifurcation
6
Hierarchy of Blood Vessels
Vein
Venule Capillary Arteriole
THE HEART
Artery
Capillaries permit the diffusion of O
2
and
nutrients from the blood into the tissues
and diffusion of waste products of the
metabolism from the tissues into the blood
7
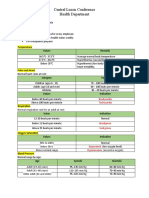
STRUCTURE FUNCTIONS
Arteries
Wall contains smooth muscle fibre that contract and relax
by instructions from nervous system
Transport oxygenated blood away
from the heart; (except pulmonary
artery).
Arterioles
Arterioles are tiny branches of arteries that lead to
capillaries. These are also under the control of the
sympathetic nervous system, and constrict and dilate, to
regulate blood flow.
Transport blood from arteries to
capillaries;
Arterioles are the main regulators
of blood flow and pressure
Capillaries
Tiny blood vessels, 5-20 m diameter. There are networks
of capillaries in most of the organs and tissues of the body.
These capillaries are supplied with blood by arterioles and
drained by venules. Capillary walls are only one cell thick
which permits exchanges of material between the contents
of the capillary and the surrounding tissue.
Supply tissues with components
of, and carried by, the blood, and
also to remove waste from the
surrounding cells as opposed to
simply moving the blood around
the body
Exchange of O
2
, CO
2
, H
2
O, salts,
etc., between blood and
surrounding body tissues.
Venules
Venules are minute vessels. Many venules unite to form a
vein
Drains blood from capillaries into
veins for return to the heart
Veins
Walls of veins consist of 3 layers of tissues that are thinner
and less elastic than the corresponding layers of aerteries.
Veins include valves that aids the return of blood to heart
and avoid reverse flow.
Transport deoxygeneted blood
towards the heart ( except
pulmonary vein)
Structures of Blood Vessels
8
Comparison between Arteries & Veins
Arteries Veins
Transport blood away from the heart
Carry oxygeneted blood
Have relatively narrow lumens
Have relatively more muscle/elastic
tissue
Transport blood under higher pressure
Do not have valves
Transport blood towards the heart
Carry de-oxygeneted blood
Have relatively wide lumens
Have relatively less muscle/elastic
tissue
Transport blood under lower pressure
Have valves throughout the main veins
of the body. These are to prevent
blood flowing in reverse direction
and/or return waste materials to the
tissues
9
Unusual Multiplicity of Tube Branching The branched
networks of tubes from the cardiovascular system and
lungs are extremely intricate and complex.
Unusual Wall Properties of Containing Vessels
Networks of vessels containing blood flow and air
flows exhibit complicated dispensability. Walls of
arteries are complicated by viscoelasticity and non-
linear features.
Major Differences
Cardiovascular System: The circulatory system which includes the heart
and the blood vessels and is responsible for the transport of blood,
dissolved oxygen, nutrient, metabolic wastes throughout the body
Viscoelasticity: Property of materials that exhibit both viscous (fluid) and
elastic (solid) characteristics when undergoing deformation
10
Unusual Fluid Properties:
Whole blood contains a suspension of 40-50% by
volume (hematocrit) of deformable bodies (mainly
red blood cells or RBCs) in a transparent plasma.
While the plasma obeys Newtonian behavior, the
whole blood is described by an effective viscosity
which increases substantially with decreasing rate
of strain due to increased formation of RBC
aggregates
Air inhaled into lung is also a suspension of dust
particles which deposit at different levels in the
bronchial tree depending upon particle size
Blood plasma: is the yellow liquid component of blood in
which the blood cells in whole blood are normally
suspended. It makes up about 55% of the total blood
volume.
Bronchial Tree: The branching of the bronchi (airway
passages) of the lung, considered as a structural and
functional unit and designed to spread air over wide
area.
Major Differences
11
Major Differences
Unusual Pulsatility
Pulmonary inspiration and expiration cause regular flow reversal in the
respiratory system
In the circulatory system, however, the arterial blood flow exhibits a
pulsatile characteristics
Attenuation of the pulse waves, due to deformable vessel walls, makes
such pulsatility less important in microcirculation and veins
Related to lungs: Pulmonary Microcirculation
Describes the small vessels in the vasculature which are embedded
within organs and are responsible for the distribution of blood within
tissues; as opposed to larger vessels in the macrocirculation which
transport blood to and from the organs.
12
Unusually Low Conduction of Heat Flux
In human body, maximum temperature is around
37C in the core region while minimum
temperature is around 34C at extremities
The temperature gradient is 0.1C/cm
Thermal conductivity of tissue is quite low ~ 0.06
W/m.K
The conduction heat flux (~ kT) ~ 0.06 W/m
2
is
low to disperse the BMR (Basal Metabolic Rate ~
72 kcal/hour) over our body surface area of 1.8
m
2
(for a normal 70kg adult)
Major Differences
Basal Metabolic Rate
The minimum calorific requirement needed to
sustain life in a resting individual. It is the
amount of energy expended while at rest in a
neutrally temperate environment, in the post-
absorptive state (i.e. the digestive system is
inactive, which requires about twelve hours of
fasting in humans)
13
Unusual Blood Cooling
When blood flows through tissues or organs, it functions not only as a carrier of
nutrients and metabolic waste but also as a coolant to remove the heat produced
by metabolism
Blood gains heat which is transferred by circulation to the skin where it is
dissipated to the environment
For maintaining body core temperature in the normal range, the blood
transfusion cooling is vital, because of the poor conduction flux
Blood cooling rate per unit volume is estimated as
The unusual feature of blood cooling is the variability range of cooling rate with
mass flow mass can be regulated by the vasomotor activity of tissue vessels
For example, vasoconstriction decreases the mass flux while vasodilation
increases it
Metabolism: The chemical processes occurring within a living cell or organism that are
necessary for the maintenance of life.
Vasomotor: Refers to actions upon a blood vessel which alter its diameter.
Vasoconstriction/Dilation: is the narrowing of the blood vessels resulting from
contraction of the muscular wall of the vessels, particularly the large arteries, small
arterioles and veins. Vasodilation refers to the widening of blood vessels resulting
from relaxation of smooth muscle cells within the vessel walls.
Major Differences
) ( ~
T T C m
q
Tissue blood arterial p b
vol
14
Unusual Thermoregulatory Mechanisms
Skin Temperature (T
s
) is one of the most important factors in the regulation
of body temperature and it varies with a change in the environmental
conditions.
For a resting person in thermally steady state, metabolic heat generation
balances the heat loss by convection and radiation
However for sudden change in ambient temperature (T
amb
), T
s
and T
core
change, activating peripheral and central thermoreceptors respectively.
Signals from thermoreceptors are integrated by the thermorgulator centers
(mainly located in Hypothalamus), which trigger the necessary regulatory
mechanisms.
The control mechanisms include
Vasomotor Systems (induce either vasodilation or vasoconstriction)
Active regulation: sweating for T
amb
>T
s
and cold induced metabolic
heat generation (including shivering and non-shivering) for T
amb
<T
s
Major Differences
A thermoreceptor is a sensory receptor, or more accurately the receptive
portion of a sensory neuron, that codes absolute and relative changes in
temperature.
Hypothalamus is an area of the brain that produces hormones which control
body temperature, hunger, moods etc.
15
Unusual Thermal Properties
Tissue thermal properties are
inhomogeneous, anisotropic
and age dependent
Unusual Range of System Size
for Heat Transfer
Ranges from microheat
transfer in cellular scale to macro
heat transfer on system scales
Major Differences
Cellular Scale: Typical length scale of an animal cell is 5-10 m. Mass Transport
processes at this scale is dominated by diffusion while heat transfer is dictated
by the enhanced surface area to volume ratio which scales as the inverse of the
characteristic length scale
Tissue Organized
Cluster of Cells
Hierarchical
Organization of Life
Inner Architecture of a
Typical Animal Cell
16
Human Plasma is transparent, slightly yellowish
with = 1.035 g/ml
It contains a solution of plasma proteins is an
aqueous medium
Proteins contain about 7% of total plasma volume
and can be classified into three major groups
Albumin, Globulin and Fibrinogen
Plasma also contains emulsified fats (or lipids),
cholesterol, free fatty acids, hormones (adrenalin),
dissolved O
2
, dissolved CO
2
Blood Rheology Blood Properties
Whole blood consists of a suspension of RBCs
(erythrocytes), WBCs (White Blood Cells or
Leukocytes) and Platlets in an aqueous solution
RBC count is approximately 5 million/mm
3
40-
45% by volume of whole blood Hematocrit
Typical dimensions of RBC 7.8 m in diameter
(Biconcave Disc), 2 m thick and 88 m
3
in volume
Function Transport of oxygen
Less number of RBC Anaemia
17
Blood Properties
RBC
WBC
Platelets
Size of WBC varies from 16 - 22 m for
monocytes to 6 - 12 m for lymphocytes
and granulocytes
WBC protects body from disease
Normal WBC:RBC concentration = 1:1000
Abnormal rise in WBC number ~
Leukemia
Platelets are smaller than RBC and WBC:
Diameter ~ 2-3 m
Platelet:RBC = 1 : 10 (number concentration)
In general platelets and WBCs are actively
not enough to influence the flow
characteristics
However, platelets play important role in
forming blood clots that may severely
interfere with flow
18
A Newtonian fluid is a fluid whose stress vs strain rate curve is linear and
passes through the origin. The constant of proportionality is known as the
viscosity (). A simple equation to describe Newtonian fluid behaviour is
shear of direction lar to perpendicu gradient velocity
fluid, by exerted stress sheer where
=
= =
dy
du
dy
du
t t
) (
0
t t
B
+ =
t =
1 , < =
n
n
t
1 , > =
n
n
t
19
Blood Properties Unusual Hydrodynamics
Fahraeus Lindquist Effect: Tendency of blood cells to move
away from the wall
At wall, they leave a layer of low viscosity
The effect is more pronounced for reduced capillary diameter (d)
Hence, apparent viscosity decreases with the reduction in
capillary diameter
Apparent viscosity increases with increasing volume
percentage of RBC (Hematorcrit)
20
Unusual Hydrodynamics - Disease
Shape of RBC changes with
flow rate
At abnormally high flow rate
and in constricted region of
circulatory system, RBCs may
deform and burst
Change in effective/apparent
viscosity with volume percentage of
RBC (also Packed Cell Volume or PCV)
is manifested in several diseases like
Anaemia or Polycythaemia
Anaemia: A decrease in normal
number of red blood cells (RBCs) or
less than the normal quantity of
hemoglobin in the blood.
Polycythaemia: A disease state in
which the proportion of blood volume
that is occupied by red blood cells
i.e. hematocrit increases
21
Blood Properties Unusual Rheology
Often represented by a Pseudoplastic behavior (apparent
viscosity decreases with increasing shear rate)
Blood is also sometimes modeled as a Bingham plastic fluid
with
0
~ 0.1 dyn/cm
2
However, the deviation from this model may be significant,
typically at low shear rates
Casson model is an empirically modified Bingham plastic model
to give a better fit to measured
app
data for lower shear rates.
As per the model
0
t t + + =
k
C
t
22
Lump Parameter Modeling of Compartmental
System with Flow Regulation
e i e i CV
QC QC V C
dt
d
m m
dt
dm
= = ) (
0 C(0) condition initial with )) ( (
) (
= = t C C Q
dt
t dC
V
i
ompartment t of the c ons V/Q Time c
e C t C solution
t
i
tan where
) 1 ( ) ( :
=
=
t
t
Note:
i. V = Constant volume of organ
ii.C
e
= C(t)
QC
e
=QC(t)
Compartment: An organ or tissue
Q: Volumetric flow rate; C: Concentration
V: Volume; m: mass = CxV
Control mass (CV)
Q
C
e
(t)
Q
C
i
(t)
23
Compartmental Systems in Parallel and Series
)) ( ) ( (
) (
)) ( (
) (
2 1 2
2
2
1 1
1
1
t C t C Q
dt
t dC
V
t C C Q
dt
t dC
V
i
=
=
) ( ) (
)) ( (
) (
)) ( (
) (
2 2 1 1
2 2 1 1
2 2 1 1 2 1
2
2
2
2
2
1
1
1
1
1
t C Q t C Q QC
C Q C Q QC
C Q C Q QC Q Q Q
t C C Q
dt
t dC
V
t C C Q
dt
t dC
V
e
e e e
i i i
i
i
+ =
+ =
+ = + =
=
=
V
1
C
1
(t)
V
2
C
2
(t)
Q
2,
C
i2
(t)
Q
1,
C
i1
(t)
Q
2,
C
e2
(t)
Q
1,
C
e1
(t)
Q,
C
i
(t) Q,
C
e
(t)
V
1
C
1
(t)
V
2
C
2
(t)
Q
C
i
(t)
Q
C
2
(t)
Q
C
1
(t)
24
Cardiac Cycle
SYSTOLIC: Heart
contracts, blood
pressure raises, and
blood moves out
along the vessels
DIASTOLIC: Heart
relaxes, blood
pressure falls, and
blood fills the heart
During systolic phase of a heartbeat cycle, blood is pumped from the heart to
one end of the aorta and walls of the aorta stretch to accommodate the
blood. During the diastolic phase, there is no blood flow into the aorta. The
walls of the aorta contract, squeezing blood out of the aorta around the
circulatory network of the body
25
Human heart is a pulsatile pump that is characterized by alternating periods of
contraction and relaxation. During the contraction phase (systole), blood is ejected from
both the ventricles and pumped into the systemic circulation and pulmonary circulation,
respectively. During the relaxation phase of the heart (diastole), the ventricles are filled
with blood in preparation for the next contraction phase. Contraction of the left ventricle
leads to the opening of aortic semilunar valve in order to eject blood into the aorta and,
hence, the systemic circulation. Contraction of the right ventricle leads to the opening of
pulmonary semilunar valve in order to eject blood into the pulmonary trunk (which
branches out into the right pulmonary artery and left pulmonary artery) and, hence, the
pulmonary circulation. To prevent back flow of blood into the ventricles, the semilunar
valves close during ventricular diastole. The cycles of ventricular contraction and
relaxation lead to maximum (systolic) and minimum (diastolic) levels of blood pressure
in the major arteries.
Arterial Blood Pressure
While systolic and diastolic pressure values are important measurements and have
tremendous diagnostic value, it is the mean arterial pressure (MAP) that drives blood
through the vasculature from the arteries to arterioles, capillaries, venules, veins, and
back to the heart. The mean arterial pressure is a time-weighted average of pressure
values in large systemic arteries during the cardiac cycle and is a function of (1) rate at
which the heart pumps blood into the large arteries, (2) the rate of blood flow out of the
large arteries to enter smaller arteries and arterioles, and (3) arterial wall compliance. If
the ventricles spent an equal length of time in systole and diastole, the mean arterial
pressure could simply be estimated as the mathematical average of systolic and
diastolic pressure values. In reality, however, the ventricles spend approximately one-
third (1/3) of their time in systole, and two-thirds (2/3) in diastole.
26
Normal blood pressure fluctuations in the aorta and other arteries.
Contraction and relaxation of the ventricles in the heart lead to maximum (systolic)
and minimum (diastolic) blood pressure values in the aorta and other arteries.
Typical systolic and diastolic pressure variation is shown. Mean arterial pressure is
shown to be approximately 93 mm Hg. Following ventricular systole, pressure in the
left ventricle rapidly drops to below that in the aorta, thus, causing the aortic
semilunar value to close and thus causes the appearance of the dicrotic notch.
Mean Arterial Pressure (MAP) is an approximation for the time-weighted average of
blood pressure values in large system arteries during the cardiac cycle.
Diastolic Pressure (DP) is the minimum blood pressure measured in large systemic
arteries. The lowest value occurs just before the start of every ventricular systole.
Pulse Pressure (PP) is the difference between systolic blood pressure and diastolic
blood pressure. Therefore, Pulse Pressure = Systolic Pressure - Diastolic Pressure.
PP)
3
1
( DP P + =
Arterial Blood Pressure
27
Compartmental Systems in Body
Heart
Q
i
Aorta
V,p
Circulatory Network
Q
e
28
Compartmental Systems in Body
]
) (
exp[
cos sin ) exp(
) exp(
: Solution
phase systolic of end and beginning at the pressure aortic are and
( and ) 0 ( : Assume
phase systolic during , sin
phase diastolic during 0,
: Assume
) ( ) (
: Aorta of on conservati Mass
blood of pressure the is and
aorta of volume the is ) ( V where
Q and ) ( : Assume
1
1
2 2
0
1 0
1 1 0
e 0
} {
a
t t b
p p
a b
t a t b
a
bt
a
A
a
bt
p p
p p
p t t p p t p
t A
Q
bp Q
dt
dp
a bp Q
dt
dV
Q Q
dt
dV
p
p
bp ap V p V
systolic
systolic
i
i i e i
=
+
+
=
= = = = =
=
= = =
= + =
e e e
e
t
e
Heart
Q
i
Aorta
V,p
Circulatory Network
Q
e
29
Some Diseases with Fluid Mechanics Relevance
Air Embolism: Cavitation of Bubbles
creates destructive action to the blood
components (RBCs typically). This can
trigger coagulation mechanisms that
produce blood clots
Thrombus is stationary clot while
Embolus is moving clot
Hemolysis: Refers to loss (damage) of
RBCs and is a measure of cell trauma.
This may be due to the diseased
condition or in presence of prosthetic
devices such as valves.
Hemolysis is triggered by
Wall-RBC interaction
Prolonged Exposure to intermediate shear
stress (1000-2000 dynes/cm
2
)
Short exposure to high shear stress (> 40,000
dynes/cm
2
)
30
Disease: Thrombosis
Thrombosis: Formation of a clot or thrombus
(an abnormal clot) in ant part of the vascular
or lymphatic system. The thrombus bump or
clot is a coagulation of blood elements or a
growth of cells formed in the heart, blood
vessel or lymphatic system.
Once a clot has developed, the continued flow
of blood past the clot may break it away from
its attachment. Such freely flowing clots are
called Emboli (Embolus in singular). These
may continue flowing until coming to a
narrow point in the circulatory system
Formation of thrombus or embolus is favored
by
Any roughened endothelial surface of a vascular
or lymphatic vessel which may be caused by
Atherosclerosis, Infection or Trauma
Very slow rate of Blood Flow
31
Diseases: Atherosclerosis
Atherosclerosis: Disease of large arteries in which lipid deposits called
Atheromatous plaques appear in the subintimal layer of the arteries. These
plaques are rich in cholesterol.
Calcium often precipitates with lipids to form calcified plaques.
In later stage, progressive sclerosis of the arteries occurs due to infiltration of
fibroblasts in the degenerative area. When both reactions take place, arteries
become extremely hard Arteriosclerosis (Hardening of Arteries).
These plaques often protrude into the flowing blood and their surface roughness
may cause clots to develop. When a small clot has developed, platelets become
entrapped and cause more clots to develop (thrombus) or the clot breaks away
(Embolus) and plugs a smaller vessel further downstream.
This is the mechanism for most coronary occlusions.
Interestingly, the presence of flow separation at branching points and bifurcation
is considered to be one form of hydrodynamic disturbance that contributes to
Atherogenesis at these sides.
Subintimal layer situated beneath the intima i.e. the innermost layer of an artery or vein.
Plaque is a deposit of fat and other substances that accumulate in the lining of the
artery wall.
Sclerosis or sclerotization is a hardening of tissue and other anatomical features.
Fibroblast is a type of cell that synthesizes and maintains the structural framework for
connective tissues such as skin, tendons, ligaments etc.
32
Illustration of Atherosclerosis
33
34
Diseases Stenosis from Atherosclerosis
Abnormal narrowing of lumen is called
as Stenosis
There are three primary methods of
treating Atherosclerosis
Balloon Angioplasty
Stenting
Arterial Bypass
Arterial Bypass: This is created to
restore flow to distal tissue by
bypassing the obstraction. The graft
may be synthetic (made from polymer
materials such as Dacron) or natural
(uses arteries or veins from other
vascular parts of the patient)
Balloon Angioplasty: Dilatation of a
balloon-tipped catheter within the
stenosis to expand the lumen
Stenting: To hold open the diseased
region by using a metallic stent
35
Endothelial Cells (ECs) that line the inner
(Luminal) surface of the vasculature are
sensitive to flow induced shear stress
Large arteries appear to vasoconstrict or
vasodilate via smooth muscle contraction and
relaxation so as to maintain wall shear stress (
w
) of 1.5 Pa under all conditions
The vasomotion is controlled partly by
endothelial productions of vasoactive molecules
such as
Vasodilators: Nitric Oxide (NO), Prostacyclin
(PGI
2
)
Vasoconstrictors: Endothelin-1 (ET-1) and
Thromboxene (TXA
2
)
Important research goal is to correlate endothelial
production of these molecules with stress
In general as shear stress is increased (e.g.
during exercise), the endothelium produces
more vasodilators to increase the lumen area
and thereby restores shear stress to its normal
value. The converse occurs when shear stress
is decreased by a decreased flow
Blood Flow and Cell Adaptation
36
Fluid Shear Stress Schematic Depiction
You might also like
- Functional organization of the cardiovascular systemDocument19 pagesFunctional organization of the cardiovascular systemIbtesam Mohammed100% (2)
- Pocket Medicine 5th Edition - The Massachuset PDFDocument661 pagesPocket Medicine 5th Edition - The Massachuset PDFSubha Saeed Khan86% (7)
- College of Mathematics and Natural Sciences: CirculationDocument7 pagesCollege of Mathematics and Natural Sciences: CirculationNelzen GarayNo ratings yet
- The Essential Guide To The New FRCR Part 2A and Radiology BoardsDocument208 pagesThe Essential Guide To The New FRCR Part 2A and Radiology Boardsbana galaxyNo ratings yet
- Circulatory SystemDocument21 pagesCirculatory SystemYusuf AzeezNo ratings yet
- Cardiac ArrhythmiasDocument11 pagesCardiac ArrhythmiasChino Paolo SamsonNo ratings yet
- Cardiovascular System AnatomyDocument16 pagesCardiovascular System AnatomyJona Addatu0% (1)
- Visceral Vascular Manipulation, 2011Document270 pagesVisceral Vascular Manipulation, 2011kkalu_just_funky91% (11)
- Noise PolutionDocument48 pagesNoise Polutionhimanshu_agraNo ratings yet
- Biology - Circulatory System Notes 1Document13 pagesBiology - Circulatory System Notes 1archit.kulkarni7756No ratings yet
- Ineffective Cerebral Tissue PerfusionDocument3 pagesIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- Chapter 8: The Mammalian Transport System: SummaryDocument4 pagesChapter 8: The Mammalian Transport System: SummaryMerimaNo ratings yet
- MF-local Circulation 2016Document61 pagesMF-local Circulation 2016OnSolomonNo ratings yet
- Waste Minimization and Cleaner ProductionDocument75 pagesWaste Minimization and Cleaner Productionhimanshu_agra100% (2)
- Note On Pressure Flow and ResistanceDocument43 pagesNote On Pressure Flow and ResistanceSilver FestusNo ratings yet
- How Blood Flows Through the HeartDocument5 pagesHow Blood Flows Through the HeartAkshay BahetyNo ratings yet
- Circulatory System and Gas Exchange Powerpoint CUMMULATIVEDocument55 pagesCirculatory System and Gas Exchange Powerpoint CUMMULATIVEAjay N. SharmaNo ratings yet
- Chapter 21 - Blood VesselsDocument6 pagesChapter 21 - Blood Vesselstomorrow.today.yesterday .yesterdayNo ratings yet
- Understanding HemodynamicsDocument41 pagesUnderstanding HemodynamicsBerihunNo ratings yet
- English PDFDocument46 pagesEnglish PDFGayatri BeheraNo ratings yet
- Types of Circulatory SystemsDocument8 pagesTypes of Circulatory SystemsJanis Micaela EsmasNo ratings yet
- Blood Circulatory SystemDocument8 pagesBlood Circulatory SystemstephanietoppoNo ratings yet
- For Quiz AnaphyDocument26 pagesFor Quiz AnaphyRuel AlejandroNo ratings yet
- Cardiovascular System: Blood Vessels and HemodynamicsDocument12 pagesCardiovascular System: Blood Vessels and HemodynamicsVon Valentine MhuteNo ratings yet
- Dr. Dini's guide to the cardiovascular systemDocument52 pagesDr. Dini's guide to the cardiovascular systemReni TeeWeeNo ratings yet
- Transport in HumansDocument29 pagesTransport in HumansMadison SmithNo ratings yet
- The Cardiovascular System: Blood Vessels: I. Overview of Blood Vessel Structure and FunctionDocument7 pagesThe Cardiovascular System: Blood Vessels: I. Overview of Blood Vessel Structure and FunctionAdam ButterworthNo ratings yet
- Biology Unit 1Document11 pagesBiology Unit 1Islam ElsayedNo ratings yet
- Mader Inquiry into Life Chapter 12 Cardiovascular System OutlineDocument3 pagesMader Inquiry into Life Chapter 12 Cardiovascular System Outline117320No ratings yet
- Circulatory System2Document9 pagesCirculatory System2Wajeeha AsifNo ratings yet
- CirculationDocument11 pagesCirculationRishikaphriya RauichandranNo ratings yet
- The Structure and Function of The Cardiovascular SystemDocument28 pagesThe Structure and Function of The Cardiovascular SystemShamaeNogaNo ratings yet
- IntroductionDocument2 pagesIntroductionEMAXE GAMINGNo ratings yet
- Chapter 42 Reading GuideDocument5 pagesChapter 42 Reading GuideCaleb SchantzNo ratings yet
- 23circulation Part 1Document13 pages23circulation Part 1Jaydave PatelNo ratings yet
- Pathophysiology of Cardiovascular System Arterial Hypertension Heart ArrhythmiasDocument38 pagesPathophysiology of Cardiovascular System Arterial Hypertension Heart ArrhythmiasLunguVictoriaNo ratings yet
- The Circulation of BloodDocument3 pagesThe Circulation of BloodTykmeto UrHartNo ratings yet
- Pathophysiology of microcirculation layers and controlDocument37 pagesPathophysiology of microcirculation layers and controlMarina ModringaNo ratings yet
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDocument61 pagesLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuNo ratings yet
- Life Process Transportaion & Excretion Batch 2023-24Document40 pagesLife Process Transportaion & Excretion Batch 2023-24Rajkumar RawatNo ratings yet
- Cardiovascular SystemDocument5 pagesCardiovascular SystemCraig100% (1)
- Circulatory System TerminologiesDocument4 pagesCirculatory System TerminologiesavduqueNo ratings yet
- 24circulation Part 2Document11 pages24circulation Part 2Jaydave PatelNo ratings yet
- Haematology. BaharDocument14 pagesHaematology. BaharJustin OmwengaNo ratings yet
- Life Process Part 2 2Document32 pagesLife Process Part 2 2Anin BertNo ratings yet
- CirculationDocument3 pagesCirculationAIKA BAYANo ratings yet
- Evolution and Functions of the Cardiovascular SystemDocument78 pagesEvolution and Functions of the Cardiovascular SystemNilay PatelNo ratings yet
- The Circulatory System: How Diffusion Led to Bulk TransportDocument10 pagesThe Circulatory System: How Diffusion Led to Bulk Transportben-jNo ratings yet
- The Circulatory SystemDocument10 pagesThe Circulatory SystemRezki RasyakNo ratings yet
- Cardiovascular System Lecture 1 2020 2021Document5 pagesCardiovascular System Lecture 1 2020 2021olawandeilo123No ratings yet
- Module 3 The Circulatory SystemDocument11 pagesModule 3 The Circulatory SystemAndriya JoshyNo ratings yet
- The MicrocirculationDocument12 pagesThe MicrocirculationRahaf Majadly100% (1)
- AcknowledgementDocument9 pagesAcknowledgementJovin AshickNo ratings yet
- Anatomy and Physiology Cardiovascular System The HeartDocument6 pagesAnatomy and Physiology Cardiovascular System The Heartmark OrpillaNo ratings yet
- The Circulatory System ExplainedDocument51 pagesThe Circulatory System ExplainedMohammed ahmedNo ratings yet
- Human Circulatory SystemDocument8 pagesHuman Circulatory SystemChelsea EdwardsNo ratings yet
- Circulatory SystemDocument44 pagesCirculatory SystemAdonai Jireh Dionne BaliteNo ratings yet
- 07 Human Transport Biology Notes IGCSE 2014 PDFDocument27 pages07 Human Transport Biology Notes IGCSE 2014 PDFJohn DeHans100% (2)
- KS3 Science Year 9 The Circulatory System-2Document15 pagesKS3 Science Year 9 The Circulatory System-2f72ktyd78nNo ratings yet
- Circulation Physiology: Dr. Dara Rosmailina Reviews Key ConceptsDocument48 pagesCirculation Physiology: Dr. Dara Rosmailina Reviews Key ConceptsYudi1223No ratings yet
- Test 3 Review Part 1Document6 pagesTest 3 Review Part 1Manduh NozzilNo ratings yet
- Circulatory SystemDocument21 pagesCirculatory SystemSaadNo ratings yet
- Chp 05 (Blood and Circulation) DrRiyadAhmed PC 3Document69 pagesChp 05 (Blood and Circulation) DrRiyadAhmed PC 3Kamrun NaherNo ratings yet
- Presidium Indirapuram Students Handout-3 Grade X (Biology) Chapter: Life Processes Topic: TransportationDocument8 pagesPresidium Indirapuram Students Handout-3 Grade X (Biology) Chapter: Life Processes Topic: TransportationSaniya nebNo ratings yet
- Micro ControllersDocument25 pagesMicro Controllershimanshu_agraNo ratings yet
- BS 3Document60 pagesBS 3himanshu_agraNo ratings yet
- RF Module Quick Mannua v3Document3 pagesRF Module Quick Mannua v3himanshu_agraNo ratings yet
- Novice's Guide To AVR DevelopmentDocument5 pagesNovice's Guide To AVR Developmentdeivs001100% (1)
- Motifs of Protein StructureDocument41 pagesMotifs of Protein Structurehimanshu_agraNo ratings yet
- Science of LIVING SYSTEM AB (Part of Unit 2)Document46 pagesScience of LIVING SYSTEM AB (Part of Unit 2)himanshu_agraNo ratings yet
- Installing USBTINY Programmer in WindowsDocument3 pagesInstalling USBTINY Programmer in Windowshimanshu_agraNo ratings yet
- Max 232Document17 pagesMax 232Rohan KelkarNo ratings yet
- L293DDocument7 pagesL293Dapi-370080950% (2)
- BS 4Document95 pagesBS 4himanshu_agraNo ratings yet
- Avr Aswarm v1.2 SchematicDocument1 pageAvr Aswarm v1.2 Schematichimanshu_agraNo ratings yet
- Bs18-1SC Kundu - Cell Division, Cell Cycle & Apoptosis (Two Lectures For Sci of Liv Sys-Autumn 2011)Document35 pagesBs18-1SC Kundu - Cell Division, Cell Cycle & Apoptosis (Two Lectures For Sci of Liv Sys-Autumn 2011)Akshat Kumar AgarwalNo ratings yet
- How To Start With AVR Series Micro ControllersDocument9 pagesHow To Start With AVR Series Micro ControllersAditya KamathNo ratings yet
- Atmega 16Document357 pagesAtmega 16Edy 'nye' IrawanNo ratings yet
- R-Sen Lecture 01bDocument57 pagesR-Sen Lecture 01bhimanshu_agraNo ratings yet
- R-Sen Lecture 01aDocument28 pagesR-Sen Lecture 01ahimanshu_agraNo ratings yet
- Bioscience: Protein Structure Function BS20001 Section 2Document27 pagesBioscience: Protein Structure Function BS20001 Section 2himanshu_agraNo ratings yet
- Science of Living SystemsDocument52 pagesScience of Living Systemshimanshu_agraNo ratings yet
- Soild Waste AmangementDocument75 pagesSoild Waste Amangementhimanshu_agraNo ratings yet
- Photosynthesis: Prof. S. Dutta GuptaDocument41 pagesPhotosynthesis: Prof. S. Dutta Guptahimanshu_agraNo ratings yet
- New 2012 04 Rabibrata Bio TransportDocument66 pagesNew 2012 04 Rabibrata Bio Transporthimanshu_agraNo ratings yet
- Eukariotic Cell StructureDocument26 pagesEukariotic Cell Structurehimanshu_agra100% (1)
- Water Treatment 25-01-2012Document57 pagesWater Treatment 25-01-2012himanshu_agra100% (1)
- Evs - Soil PollutionDocument47 pagesEvs - Soil Pollutionhimanshu_agraNo ratings yet
- Cell StructureDocument17 pagesCell StructureSoumyadeep MajumdarNo ratings yet
- Wastewater Treatment: Department of Civil Engineering Indian Institute of Technology KharagpurDocument26 pagesWastewater Treatment: Department of Civil Engineering Indian Institute of Technology Kharagpurhimanshu_agraNo ratings yet
- Water Pollution18!01!2012Document41 pagesWater Pollution18!01!2012himanshu_agraNo ratings yet
- CPR Saves Lives in Cardiac ArrestDocument17 pagesCPR Saves Lives in Cardiac ArrestAntonioSánchezRodríguezNo ratings yet
- F3 Workbook p45-47Document3 pagesF3 Workbook p45-47jnieeeNo ratings yet
- 2541 FullDocument100 pages2541 FullIrina Luciana DumitriuNo ratings yet
- First Aid Management of Haemorrhage: Veterinary Nursing JournalDocument3 pagesFirst Aid Management of Haemorrhage: Veterinary Nursing JournalRizqiNo ratings yet
- ASA Classifications 4-09Document2 pagesASA Classifications 4-09FaridahMaksumNo ratings yet
- Aortoiliac Occlusive DiseaseDocument37 pagesAortoiliac Occlusive Diseasewolff_512No ratings yet
- Arteriovenous FistulaDocument11 pagesArteriovenous FistulaAbby GuiritanNo ratings yet
- Normal Values ChartDocument1 pageNormal Values ChartHiesel Madera VaronaNo ratings yet
- SP 2.3c - Dissection of A Mammalian HeartDocument4 pagesSP 2.3c - Dissection of A Mammalian HeartPinu CattoNo ratings yet
- Wednesday 6 May 2020: Human BiologyDocument24 pagesWednesday 6 May 2020: Human BiologySimam RistaNo ratings yet
- Laporan KematianDocument1 pageLaporan KematianIntan Robi'ahNo ratings yet
- Anatomy Review Blood Vessel PDFDocument6 pagesAnatomy Review Blood Vessel PDFAngeliki HoNo ratings yet
- Heart FailureDocument8 pagesHeart FailureApple Mae AlmoniaNo ratings yet
- D3 Nursing Study Program on AMI Patient CareDocument8 pagesD3 Nursing Study Program on AMI Patient CareNurul HendrianiNo ratings yet
- Viskin Et Al 2021 Polymorphic Ventricular Tachycardia Terminology Mechanism Diagnosis and Emergency TherapyDocument17 pagesViskin Et Al 2021 Polymorphic Ventricular Tachycardia Terminology Mechanism Diagnosis and Emergency TherapyMey TalabessyNo ratings yet
- Reflective Writing 4Document2 pagesReflective Writing 4Luiza NiyazmetovaNo ratings yet
- SolutionDocument6 pagesSolutionAmanda IrvingNo ratings yet
- Cardiac Enzymes Practical Handout For 2nd Year MBBSDocument7 pagesCardiac Enzymes Practical Handout For 2nd Year MBBSIMDCBiochemNo ratings yet
- Ecg PDFDocument2 pagesEcg PDFNaveen SharmaNo ratings yet
- Jurnal PPT Sindrom BrugadaDocument64 pagesJurnal PPT Sindrom Brugadasoraya olyfiaNo ratings yet
- Cardiovascular Histology Layers and StructuresDocument4 pagesCardiovascular Histology Layers and StructuresJason Anthony SupenaNo ratings yet
- CABGDocument16 pagesCABGhama cr7No ratings yet
- 2015 ESC Guidelines For The ManagementDocument59 pages2015 ESC Guidelines For The ManagementSri WahyuniNo ratings yet
- The Influence of Anesthesia On Cardiac RepolarizationDocument13 pagesThe Influence of Anesthesia On Cardiac Repolarizationzuraini_mdnoorNo ratings yet
- Cardiovascular System Physiology LectureDocument28 pagesCardiovascular System Physiology LecturevincenzoNo ratings yet
- DigoxinDocument2 pagesDigoxinMohamed M. AbdElhalimNo ratings yet