Professional Documents
Culture Documents
Perintal Care of Hiv+ Ve Mother - New
Uploaded by
chandanbarmanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perintal Care of Hiv+ Ve Mother - New
Uploaded by
chandanbarmanCopyright:
Available Formats
DR.
JAVED ALI, MD(O&G) ASSIATANT PROFESSOR GMCH,GUWAHATI
1-2 Per thousand pregnant women in US. Less than 0.5% in most asian countries. In India the rate varies from 0-2.4%. 54 seropositive women detected in department of O&G GMCH. 14 cases underwent caesarian section and 33 cases had vaginal delivery in our department. The rate of transmission from mother to child is in between 15-48%.
Over 5,90,000 children are infected with HIV each year by vertical transmission.(USAID report 1997). Estimated risk of infection to the health care providers after parenteral or mucous membrane exposure is 0.36%.
A. MATERNAL viral load Biological prototype of virus Unprotected sex during pregnancy Smoking & illicit use of drugs in mother Maternal level of CD4 & lymphocyte count. Low maternal vit A level. Presence of RT9/ST9 in mother. Time of rupture of membranes & choriomeningitis Episiotomy & operative vaginal delivery Presence & amount of virus in genital tract.
B.FETAL Fetus can ingest the virus Fetal scalp electrode, scalp blood sampling & umblical blood sampling. Duration of exposure to maternal secretions ( first twin). Via breast milk depending upon the immune response of the fetus, duration of breastfeeding and infectivity of mother.
Does not enhance disease progression. Serious infections do occur if CD4 count is <300 or severe end stage immunodeficiency.
Fertility not impaired in initial stages. Late HIV disease may cause IUGR, preterm delivery, IUD, neonatal death, higher incidence of birth canal sepsis, and opportunistic infections.
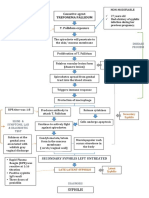
KNOWN HIV+VE CASE Booked/Unbooked DETECTED ONLY IN LABOUR PRESENTING WITH AIDS
THE KEY
1. Optimal care of the pregnancy
- Nutritious diet - Prevent anaemia, hypoprotenemia - Choice of MTP/continuation of pregnancy - Discontinue smoking, illicit drugs - Regular check up - Detect & treat opportunistic infections - Proper intranatal care in hospital
2. Care of the HIV infection
PERVENT VERTICAL TRANSMISSION PREVENT SPREAD OF INFECTION Take universal precaution Proper disposal wastes Disinfection and sterilisation of linens and equipments. THE APPROACHKEEP UTMOST SECRECY BE NON INSISTENT BUT GENTLE.
SHAVING ENEMA CATHETERISATION PV EXAMINATION IV CANULATION INJECTION DRAWING BLOOD OR COLLECTIING URINE SAMPLES
SHOULD WE DO ELECTIVE CESAREAN SECTION? OR
ALLOW VAGINAL DELIVERY?
Each time after examining the patient, wash hand in automatic water tap with soap. Always keep delivery tray ready with linen and cord clamp. Take universal precautions while conducting delivery Never deliver a women without gloved hands(taxi/toilet delivery) Never keep sharp instruments around perineum on delivery table to avoid cut to mother/ baby or to the health worker.
Avoid repeated per vaginal examination to avoid infection Avoid catheterisation unless indicated. Drape perineal area with sterile linen while delivering a woman or suturing episiotomy and perineal tears. A maternal sample for plasma viral load should be taken at the time of delivery. Amniotomy, application of scalp electrodes, scalp blood sampling should better be avoided. Mechanical suctioning( <140mmHg) devices should be used to remove secretions from neonates airway.
Never guide the needle with fingers Non touch technique is the best. Any spillage of blood or fluid over skin area should be washed immediately. Put wash proof band aid over any cut or abrasion before putting on gloves. In case of accidental needle prick or spillage over skin or mucus membrane with breach, take immediate prophylaxis, triple therapy for 4 wks. Cord should be clamped early. Baby should be bathed immediately.
Double gloves Special puncture resistant glove if available. Using eye glasses, shield, special gowns and boots. Spinal anaethesia preferable Liberal incision There should not be active bleeding from incision wound while extracting the baby. Disinfection of anesthesia equipments. Other precautions already mentioned in precautions in vaginal delivery. Universal precautions by anaethetist and paediatrician.
UNIVERSAL PRECAUTIONS
nn
NEONATOLOGIST
(WITH UNIVERSAL PRECAUTIONS)
MEMBERS OF THE OPERATING TEAM
ISSUES- Gestational age - Severity ( viral load/ CD4 count) - Tolerance of regimen during pregnancy - Potential adverse effects
ACTG O76 TRIALZidovudin-100mg 5times a day from 14wks until labour. During labour2mg/kg over 1st 2hrs maintainence dose of 1mg/kg/hr until delivery zidovudin syrup- 2mg/kg 4times a day for the 6 weeks to the neonate
SHORT COURSE ZDV300mg zidovudin twice daily from 36wks until onset of labour then every 3hrs till delivery neonate is given 2mg/kg ZDV syrup QID for 1 week
HIV NET 02Nevirapin 200mg 2 tabs to mother at the time of delivery neonate- Nevirapin syrup 2mg/kg in single dose within 72 hrs In case of LSCS- Nevirapin is given 4 hrs before procedure
IF ON ART OPTIONS ARE Suspend therapy temporarily during 1st trimester. Continue the same therapy Change to a different regimen If not on ART- prophylaxis (PPTCT)
ART may be delayed if in the 1st trimester Weigh the severity of the disease and the potential benefits/risks of delaying ART until after 1st trimester. For the women who are severely ill, the benefit of early initiation of ART may outweigh the risk to fetus.
Postpartum care
Actual HIV status of the baby can only be ascertained by PCR and P24 Antigen. After 15 months of breastfeeding HIV-1 transmissions to the infant is around 32% The mother should be counseled regarding the risks and benefits. She should be helped to make an informed choice. In India because of the potential risks of diarrhoea and other diseases involved in alternative feeding, breastfeeding has not been routinely disregarded. If breast feeding is chosen as an option, encourage exclusive breastfefeeding and advise early cessation.
Awareness about infectionBurning micturation Fever Foul smelling lochia Cough sputum,shortness of breath Redness,pain,pus,discharge from incision/episiotomy Lower abdominal pain She should be told about disposal of sanitary pads etc. and care of perineum and breast.
COTRACEPTIVE ADVICE- condoms - sterilization
Regular gynecological care including pap smears. Regular HIV/AIDS care- medical follow up/ visit to ART centre. Nutrition and dietary care Family planning services.
1.RED CONTAINER/BAGSsyringes, canula , catheter, needles , blood bag, drip set , gloves& any infectious item. 2. YELLOW CONTAINER/ BAGSBlood soaked articles like cotton bandages, dressings, plasters, pathological and anatomical wastes and other laboratory wastes. 3. BLUE CONTAINER/ BAGSBroken glass , blades, scalpels. 4. BLACK CONTAINER/BAGSOffice wastes, kitchen& canteen wastes. other non infectious wastes
Put soiled linen, gloves and instruments in 10% hypochloride solution/ bleach solution for 10 minutes before washing. A toothbrush may be used for cleaning the instruments. Pour bleach solution on labour table for half an hour. It can also be disinfected using 10% lysol or 2% gluteraldehyde. Put the placenta in a bag with bleaching powdereither incinerate or burry with bleaching powder all around. Floor soiled with blood or amniotic fluid should be cleaned with antiseptic/ bleach solution immediately.
Disposable syringes and needles should be disinfected using bleach solution/ gluteraldehyde/mutilation/ shredding. Universal precautions should also be adopted by workers in the labour room. Heavy duty gloves or utility gloves best be used.
Every obstetrician or maternity service provider has already delivered or will deliver HIV+VE mother knowingly or unknowingly. We must keep abreast with the recent developments in HIV/AIDS. Need not be panicked. Keep secrecy, be non insistent, but gentle this will help her not to disappear. Proper care can help prevent vertical transmission and as well as prevent spread of the disease. There is a little risk to service provider if universal precaution is adopted.
THANK YOU!
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nursing Care PlanDocument10 pagesNursing Care PlanSittie Rohaina SabanNo ratings yet
- The Client With Urinary Tract InfectionDocument4 pagesThe Client With Urinary Tract InfectionMarisol Jane JomayaNo ratings yet
- CALAS - Module4 All Chapters FINAL2018Document349 pagesCALAS - Module4 All Chapters FINAL2018Muneeb ArshadNo ratings yet
- Experimental Research Chapter 1-3Document16 pagesExperimental Research Chapter 1-3kristleNo ratings yet
- Stool AnalysisDocument11 pagesStool AnalysisMohsen Haleem100% (1)
- Viral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDocument14 pagesViral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDARLENE CLAIRE ANDEZANo ratings yet
- Daftar PustakaDocument2 pagesDaftar Pustakacute_chooeyNo ratings yet
- BacillusDocument18 pagesBacillusdrparachuruNo ratings yet
- Filariasis: Signs and SymptomsDocument30 pagesFilariasis: Signs and SymptomsAnonymous VJjzqbAlNo ratings yet
- Digestive SystemDocument42 pagesDigestive Systemapi-87967494100% (1)
- Kode Diagnosa P-Care - SimpusDocument2 pagesKode Diagnosa P-Care - SimpusiqbalNo ratings yet
- Presepsin Reference Poster 2012Document1 pagePresepsin Reference Poster 2012donkeyendutNo ratings yet
- Path o Physiology of SyphilisDocument1 pagePath o Physiology of Syphilis3S - JOCSON, DENESE NICOLE LEE M.No ratings yet
- Idr 177247 Healthcare Associated Infections An Overview 111418Document13 pagesIdr 177247 Healthcare Associated Infections An Overview 111418ednihs100% (1)
- Systemic Diseases and The EyeDocument17 pagesSystemic Diseases and The Eyeapi-337689057No ratings yet
- Fish Disease BookDocument112 pagesFish Disease BookMemo KenaweeNo ratings yet
- Pathology of The Nervous SystemDocument163 pagesPathology of The Nervous SystemEmmanuel De Leon100% (1)
- Medlifeline Drug of Choice 1st EditionDocument39 pagesMedlifeline Drug of Choice 1st EditionAswin Krishna83% (6)
- DrugsDocument98 pagesDrugsReo PratapNo ratings yet
- Reporting Draft For PPT InputsDocument2 pagesReporting Draft For PPT InputsPhaestus ReverseNo ratings yet
- A& P II Assignment 2Document5 pagesA& P II Assignment 2hepnandeNo ratings yet
- PCV 13Document2 pagesPCV 13api-237098034No ratings yet
- 2015 HBV EQA Result FormDocument3 pages2015 HBV EQA Result FormTiny Coffee HouseNo ratings yet
- Covid 19 RRLDocument2 pagesCovid 19 RRLPurple Ivy GuarraNo ratings yet
- Diaper Rash: What Is Diaper Rash? What Can I Do If My Baby Gets Diaper Rash?Document2 pagesDiaper Rash: What Is Diaper Rash? What Can I Do If My Baby Gets Diaper Rash?gkNo ratings yet
- IBRDocument2 pagesIBRAde HermawanNo ratings yet
- Pest Management Program For Grape Series Downy Mildew of GrapeDocument4 pagesPest Management Program For Grape Series Downy Mildew of Grapeagrosergio2010920No ratings yet
- Self-Assessment Colour Review of Small Animal Soft Tissue SurgeryDocument194 pagesSelf-Assessment Colour Review of Small Animal Soft Tissue Surgerymiliindianu100% (3)
- Nursing Leadership and ManagementDocument7 pagesNursing Leadership and ManagementRamon Carlo AlmiranezNo ratings yet
- Acute Vs Chronic Disease: Comparison ChartDocument3 pagesAcute Vs Chronic Disease: Comparison ChartMoise FloriNo ratings yet