Professional Documents
Culture Documents
DSTC 0309-Dcs & DCR Updated
Uploaded by
Denny TombengOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DSTC 0309-Dcs & DCR Updated
Uploaded by
Denny TombengCopyright:
Available Formats
DAMAGE CONTROL SURGERY
AND
DAMAGE CONTROL RESUSCITATION
UPDATED
Warko Karnadihardja
BANDUNG
03-09
DAMAGE CONTROL
Two types of damage control (since 2004 after
starting Iraqi large scale conflict)
DAMAGE CONTROL SURGERY
Stop bleeding
Stop contamination
Temporary abdominal closure
DAMAGE CONTROL RESUSCITATION
Early management of coagulopathy
And other component of lethal triad
RESPONS TERHADAP RESUSITASI CAIRAN
RAPID RESPONSE
TRANSIENT RESPONSE
NO RESPONSE
WINDOW OF OPPORTUNITY 90 MINUTES
Simulation of heat loss during damage
control
C
o
r
e
T
e
m
p
e
r
a
t
u
r
e
(
C
)
Time (hours)
Operative Profiles
1 hour laparotomy at 21C
90 minutes at 21 C
90 minutes at 24 C
Therapeutic
window
36
32
30
30 60 90
120
0
Traditional approach
individual ligation
DSTC / KT- IKABI
Perihepatic
Packing &
drainage
-damage
control
DSTC / KT- IKABI
Damage
control
packing
DSTC / KT- IKABI
DAMAGE CONTROL
Packing
History
12-06-05 : Kecelakaan lalu lintas, tabrakan
sepeda motor dgn truk, terlempar
Klinis: Mild Head Injury + # maxilla LeFort 1 +
# antebrachii D (closed) + # femur D (closed)
+ abdominal bleeding + shock hemorrhagic
12-06-05: Damage Control Surgery 1
(packing) di RS A ruptur Liver Grade IV
medial dari gallbladder bed
History
Post-op di ICU cepat stabil
15-06-05 : re-laparotomy bleeding
berhenti, angkat packing dipasang 2
buah drain di subhepatic & pelvis
Masalah post-op ke-2 : dari drain keluar
empedu 1500 cc/hari, terutama dari
pelvic, tachycardia, febris, gut failure
Os kemudian pindah ke RS Borromeus
29-06-05 dilakukan CT scan
DAMAGE CONTROL
Penetrating injury: Through-and-through
To avoid an extensive hepatotomy
Utilize an intra hepatic ballon, made from
a Penrose drain
Tamponade within the liver parenchyma
Heroic approach
- High mortality
In non specialized
center
DSTC / KT- IKABI
Sites of OLeary Suture Placement
and Utero-Ovarian Ligament
Ligation
DSTC / KT- IKABI
Transvaginal Pelvic Pressure Pack
DSTC / KT- IKABI
B-LYNCH SUTURE FOR SURGICAL
CONTROL OF UTERINE HEMORRHAGE
B-Lynch, Br J Obstetric gynaecol, 1997; 104: 372-
375
Technique of Extravascular Balloon
Occlusion
of Uncontrolled Bleeding in the Neck
DSTC / KT- IKABI
MULTIPLE BALLOON OCCLUSION
DCS in Complex Vascular and
Bony Injury in the Thigh
DSTC / KT- IKABI
Penetrating Pelvic Injury
DSTC / KT- IKABI
Pulmonary Tractotomy with
Selective Vascular Ligation
DSTC / KT- IKABI
DAMAGE CONTROL SURGERY AND SEQUENCE
OF RELAPAROTOMY & CLOSURE
Jacobs M et.al :ATOM, 2003
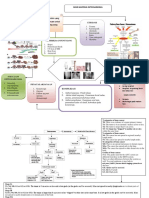
MANAGEMENT TREE FOR BLEEDING INTRAPERITONEAL
INJURIES
Chiara, O, Cimbanasi S and Vesconi S : Critical Bleeding in Blunt Trauma
Patients in 2006 Year Book of Intensive Care and Emergency Medicine,
Springer 2006
NOM: nonoperative management
DCS:damage control surgery
US : Ultrasound
PRBC: Pached red blood cells
Hemodynamically
stable
ATLS protocol
Hemodynamically
unstable
CT scan
Hollow viscus or
Diaphragmatic injuries
US-fast
Contrast extravasation
celitomy
If:
Acidosis
Hypothermia
> 8 PRBC
coagulopathy
D.C.S
Angiography-embolization
N.O.M
Ongoing
bleeding
MANAGEMENT TREE OF COMPLEX INJURIES OF THE
EXTREMITIES
Chiara, O, Cimbanasi S and Vesconi S : Critical Bleeding in Blunt Trauma Patients in 2006 Year Book of Intensive Care and Emergency Medicine,Springer 2006
DCO:
Damage control
orthopedics
Extremity injury
Stop hemorrhage
Check for:
1. Peripheral perfusion
2. Motor/sensory function
3. Bone integrity
4. Soft tissue integrity
Three or more
Components
involved
no yes
Systemic injuries
With higher priority
no yes
Definitive
repair
DCO
successful unsuccessful
Early
amputation
Damage Control Sequence
PART I - OR
control hemorrhage
control contamination
intraabdominal packing
temporary closure
PART III - OR
pack removal
definitive repair
PART II - ICU
core rewarming
correct coagulopathy
maximize hemodynamics
ventilatory support
injury identification
(tertiary survey)
Transfer problems
Transfer problems
DSTC / KT- IKABI
Bogota Bag Abdominal
Closure
using Plastic Bag of Saline Solution
DSTC / KT- IKABI
Warko Karnadihardja, 2000 Bandung
HYPOTHERMIA PREVENTION IN O.R & ICU
Warko Karnadihardja, 2000 Bandung
Intra-Abdominal Hypertension
(IAH)
A sustained increase in intra-
abdominal pressure (IAP), can cause
hemodynamic, respiratory, splanchnic
and renal dysfunction
(Midwinter MJ, UK, 2004)
Some authors consider that IAH as first hit
leading to SIRS
Abdominal Compartment Syndrome
(ACS)
Multiple organ dysfunction syndrome (MODS)
attributable to increased intraabdominal
pressures (IAPs), that improves clinically by
decompressive laparotomy
Some authors consider as Second Hit leading to MODS - MOF
Predisposing Factors to Development of
ACS
Extensive abdominal and pelvic injury
Damage control surgery
Abdominal packing : over or under
packing
Continuing bleeding
Extensive contamination of peritoneal cavity
Massive transfusions and crystaloid infusions
Inadequate resuscitation
The presence of triad of death in trauma
patients: hypothermia-coagulopathy-acidosis
Closure the fascia and skin under tension
Measuring Intraabdominal Pressure
(IAP)
Direct Method
Directly placed a catheter into the
peritoneal cavity, attaching to a saline
manometer or pressure transducer
Indirect Method
Measurement of
Bladder pressure most popular
Gastric pressure
IVC pressure
Measurement of urinary bladder
pressure
Steven L.Lee et al, The Journal of Trauma, Injury, Infection and Critical Care,
Vol 52, No.52, June 2002
Diagnosis
Intravesical monitoring
Most closely reflects
direct monitoring1,2
Foley clamped distal to
aspiration port
50 to 100 cc saline
injected into bladder
16-guage needle
connected to pressure
transducer, inserted into
aspiration port
1 Obeid F, Saba A, Fath J, et al. Increases in intraabdominal pressure affect pulmonary compliance. Arch Surg
1995; 130:544-548
2 Iberti TJ, Kelly KM, Gentili DR, Hirsch S, Benjamin E. A simple technique to accurately determine intraabdominal
pressure. Crit Care Med 1987;11401142
Grading System of ACS
Grade Bladder pressure
(mmHg)
I 10 15
II 16 25
III 26 35
IV > 35
Meldrum DR, Moore FA, Moore FE, et al. Am J Surg 174: 667; 1997.
1 mmHg = 1,26 cmH
2
O
Percentage of Patients with Respective Organ
Dysfunction per Grade of Abdominal Compartment
Syndrome
Grade UO < 0.5 PAP > 45 SVR > 1000 DO
2
I < 600
ml/kg/hr
I 0% 0% 0% 0%
II 0% 40% 20% 20%
III 65% 78% 65% 57%
IV 100% 100% 100% 100%
PAP: Peak Airway Pressure (cmH
2
O), DO
2
I: Oxygen Delivery Index (ml O
2
/min/m
2
), SVR:
Systemic Vascular Resistance (dyne/sec/cm
-5
), UO: Urine Output (ml/min)
Meldrum DR, Moore FA, Moore FE, et al. Am J Surg 174: 667; 1997.
THE BROWNER PELVIC STABILIZER IN USED
PREPERITONEAL PELVIC PACKING
PREPERITONEAL PELVIC PACKING
PREPERITONEAL PELVIC PACKING
EXTRAPERITONEAL PELVIC
PACKING
EXTRAPERITONEAL PELVIC
PACKING
Kees-Jan Ponsen et al: J Trauma 2006: 61:662-667
MODIFIED STOPPA APPROACH IN PELVIC
RING AND ACETABULAR FRACTURES
INTERNAL FIXATION FOR RIGHT SACROILIAC
AND SYMPHYSEAL SEPARATIONS
Ahmet Yilmaz Sarlak et al: J Trauma 2006: 61:749-751
FRAKTUR PELVIK DENGAN FIKSASI
EKSTERNA
ALGORITHM FOR MANAGEMENT OF
PELVIC FRACTURE
WTA, J Trauma, 2008, 65 ; 1012-1015
DAMAGE CONTROL RESUSCITATION
Early Coagulopathy Treatment
in Severe Trauma
Lessons learned from the war
IN THE PAST
DIRECT TREATMENT OF COAGULOPATHY HAS
BEEN RELATIVELY NEGLECTED, VIEWED AS
BY PRODUCT OF RESUSCITATION,
HEMODILUTION AND HYPOTHERMIA
TOWARDS NEW PARADIGM
IN TRAUMA CARE
Rapid progress in trauma care occurs when the result
of the research are promptly integrated into clinical
practice such as special lessons learned from modern
large scale conflicts
Large scale conflicts is defined as
Conflicts that occurs after 1990
Involving more than 50.000 US or coalition
combatants
Involving invasion of foreign soil during US military
combat operations
CONVENTIONAL DAMAGE CONTROL
The Basic Thinking
When the lethal triad of hypothermia, acidosis and
coagulopathy are present, death is imminent
Current teaching is to avoid reaching these
conditions by using damage control surgery
focuses on rapid reversal of acidosis and prevention
of hypothermia, and
Surgical techniques focus on controlling
hemorrhage and contamination
DAMAGE CONTROL RESUSCITATION
ADDRESSES
THE ENTIRE LETHAL TRIAD IMMEDIATELY
PRESENTS UPON ADMISSION TO A
COMBAT HOSPITAL
AND SHOULD BE TREATED EARLIER
Hess JR et al : Damage Control Resuscitation: Transfusion, 2006;46; 685-686
Mc Mullin NR et al: Hemostatic Resuscitation in YBICEM, 2006, PP 265-278
TRIAD
OF
DEATH
Moore EE Am J Surg,
1996, 172;405
BETULKAH KOAGULOPATI SUATU
PARADIGMA BARU DALAM TRAUMA ?
Kalau terjadi koagulopati, apakah itu
Terjadi secara primer ?
atau
Akibat kejadian sekunder ?
THEORY OF TRAUMATIC COAGULOPATHY
As primary event modified by promoters
Mc Leod, JBA, Arch Surg 143, Aug.2008
THEORY OF TRAUMATIC COAGULOPATHY
As secondary event
Mc Leod, JBA, Arch Surg 143, Aug.2008
Class IV Hemorrhage
Confused, lethargic
Hypotension
Heart rate > 140 / min
Decreased pulse pressure
Respirations >35 / min
Urinary output negligible
>2000 mL BVL (>40%)
Definitive control,
blood components
ATLS 2008
Hypothermia
Early coagulopathy
Pitfalls
Pitfalls
Complications of Shock and Shock Management
ATLS 2008
THE FACTS
In the severely injured the
coagulopathy of trauma is present at
admission
Recent studies have brought back to
light the importance of treating this
disorder at an earlier stage
Brohi K et al.J.Trauma 2003, 54 Hirshberg A et al, J Trauma 2003,
54 Mc Leod JB et al: J Trauma 2003, 54, Faringer PD et al.J.Trauma,
1993,34
THE FACTS
Reports of RL and NaCl 0.9% solutions
increasing reperfusion injury and leucocyte
adhesion lead one to conclude that the
standards crystalloid-based resuscitation
guidelines in PHTLS and ATLS may worsen
the presenting acidosis and coagulopathy
in severely injured trauma pts
Possibly increase ARDS, SIRS and MOF
Combra R et al.J. Trauma 1997,42, Cotton BA et al Shock,
2006,26,Rhee P et al: Crit Care Med 2000,28, Ayuste E L et al J
Trauma 2006,60 Rhee P et al: J. Trauma 2003.54 (Suppl)
The safety of with holding PRBC in hemodynamically
stable pts has been demonstrated
Herbert PC et al N Eng J Med 1999,340
The risks associated with blood transfusion are well
described
Sheppard FR et al J Trauma, 2004.53 Malone et al: J
Trauma, 2003, 54
Massive transfusion in military and civilian casualties
has been associated with an increase of death
Como JJ et al : Transfusion 2004,44
Eastridge BJ et al : J Trauma, 2006.61
Hoyt DB : Semin Hematal, 2004,41 ( Suppl)
THE FACTS
MASSIVE TRANSFUSION
> 10 units RBCs in the first 24 hours, are
uncommon and constitute only 1% to 2 %
the patient population in the largest civilian
academic trauma centers
But 7% to 10% of combat casualties require
massive transfusion
An opportunity to observe the effects of
new resuscitation strategies in the combat
hospitals of Iraq and Afghanistan
DIFFERENT AVAILABILITY TO BLOOD PRODUCTS
BETWEEN CIVILIAN AND COMBAT SYSTEMS
In civilian systems, treatment of
coagulopathy is often limited by standard
blood bank logistics
In combat hospital in Iraq frequently have
immediate access to PRBCs and thawed AB
or A plasma
Rapid access to apheresis platelets,
prepooled cryoprecipitate, fresh whole
blood and rF VIIa
PROTOCOL FOR THE USE OF rFVIIa IN
CRITICAL HEMORRHAGE IN THE BLUNT TRAUMA PATIENT
Chiara, O, Cimbanasi S and Vesconi S : Critical Bleeding in Blunt Trauma Patients in 2006 Year
Book of Intensive Care and Emergency Medicine, Springer 2006
INR: International Normalized Ratio
FFP: Fresh Frozen Plasme
PLT: Platelets
CPR: Cardio pulmonary resuscitation
Non-mechanical bleeding in:
- Pelvic ring disruption
- Intraperitoneal injury
- Injury of extremities and
- Multiple transfusions (>
8 PRBC within 4 h)
- Coagulopathy (INR>1.5)
1. Infuse FFP 10 ml/kg
2. Give PLT (> 50.000)
3. Correct fibrinogen
(>50 mg/dl)
4. Correct pH (>7.2)
5. Check again for surgical
bleeding
Still
bleeding
Still
bleeding
Traumatic bleeding in patient on
pre-injury anticoagulant therapy
Still bleeding after 120 min
rFVIIa 90 g/kg
rFVIIa 90 g/kg
Exclude (futile administration) If:
pH < 7.1
Lactate > 13 mmol/l
Previous or impending CPR
DENVER GROUPS POLICY IN THE
RESUSCITATION FOR BLEEDING PELVIC TRAUMA
Resuscitate with 2 L crystalloid-place CVP line-Measure-Base Deficit-
R/O Thoracic Source (Portable Chest X-Ray)
If beginning to transfuse PRBCs, start thinking about pelvic packing
Transfuse PRBC and FFP 1:1 ;1 apheresis unit PLT for each 5 U PRBC
Immediate Notification: Attending Trauma Surgeon, Attending
Orthopaedic Surgeon, Blood Bank Resident, IR Fellow
Cothren EC et al, Denver Group. USA, J.Trauma 2007, vol 62 N 4: 834-842
LOS ANGELES COUNTRY MEDICAL CENTER
Rapid Uncontrolled
Hemorrhagic Shock
HEMORRHAGE CONTROL
(surgical/endovascular)
Send type and crossmatch,
aPTT, INR and platelet count
Autotransfusion of shed
pleural blood
Hypotermia control
(Warm fluids & vent gases,
remove wet clothing, dry
patient, Bair Hugger, etc)
1. Start with 0 negative PRBC
Opening ER or OR fridge containing 8 units
of O negative blood automatically phones
blood bank to notify them of units taken
2. Switch to type specific or crossmatched blood as
soon as it is available
LAC-USC Trauma transfusion protocol. aPTT, activated partial thromboplastin time, FFP, fresh frozen plasma, INR, International
normalized ratio. PRBC, packed red blood cells
COMPONENT THERAPY TRIGGERS
EMPIRIC
1. >6 units of PRBC
2. History of coumadin
TARGETED
ABNORMAL:
aPTT/INR
Platelet < 50x10
3
Fibrinogen < 100
Request trauma cooler
6 units type specific FFP
(pre-thawed)
1 unit ABO/Rh matched
apheresis platelets
Request trauma cooler
6 units type specific FFP
(pre-thawed)
1 unit ABO/Rh matched
apheresis platelets
cryoprecitate
Recombinant factor VIIa
100 mcg/kg
Additional doses as required
(best if pH > 7.1 and T > 35
0C)
LOS ANGELES COUNTRY MEDICAL CENTER
DIFFUSE
NONSURGICAL
BLEEDING
Alam H.B, P Rhee, Surg. Clin N Am, 2007
FLOW DIAGRAM OF MASSIVE TRANSFUSION/FRESH WHOLE BLOOD
TRANSFUSION PROTOCOL EMPLOYED
Repine TB, Perkins J, Kauvar D, Blackborne L, J Trauma, 2006
Emergency
Release pRBCs
Initial labs
Type & cross
4 Prbc
4 FFP
4 pRBC
4 FFP
16pk platelets
(when available)
4 pRBC
4 FFP
Protocol terminated when no longer needed
60 min
4 fresh whole
blood
4 fresh whole
blood
Surgeon
Blood bank
Time=0
Suspend
routne duties
Get help
Massive
Transfusion pack
4 pRBC
4 FFP
10 cryoppt
30 min
90 min
120 min
Whole
blood drive
Nursing supervisor
Notify
command
Walking Blood Bank
Additional donors called
from phone list ~8 at a
Time Any gaps in donors
filled with additional
donors
BY THE 31
st
COMBAT SUPPORT HOSPITAL IN BAGHDAD, IRAQ
Writtened report on wound dressing
MAJ Alec C Beekley, MD, Surg Clin N Am 86 ,2006, 689-709
MASSIVE BLEEDING
BLOOD COMPONENT TRANSFUSION
BLOOD COMPONENT TRANSFUSION
DCR + DC + RECONSTRUCTION +
AMPUTATION
COMBAT CASUALTY CARE ISSUES &
SOLUTIONS LESSONS LEARNED FROM IRAQI
WAR
By August 2005, > 275.000 combat application
torniquets (CAT-1) had been seen to Iraq
Small portable fluid warmers are being approved
for use on helicopters
Critically ill patients are placed in vinyl body bags
to conserve heat
CAVR ( Continuous Arterio Venous Rewarning)
decreases rewarning times and blood product
requirements at CSH
CSH : Combat Service Hospital
THE FUTURE DIRECTIONS
Perceptive observation
Thoughtful discussion
Insightful analysis concerning medical
care during war, will generate
recommendations for new and
improved medical practice
DSTC / KT- IKABI
CONTOH
KASUS
CONTOH KASUS DSTC 11-05
1. Nn. LH
19 TAHUN di Bandung
Tgl 3/8/05 jam 16.05 KLL motor menabrak
mobil, perut kena stang.
15 menit kemudian ke UGD RSB, c.m
hipotensi, resusitasi, rapid response.
M.I.S.T ?
Tanda-tanda peritonitis, konsul bedah
indikasi laparotomi
Hb 8 g%, hematokrit 24%, leukosit 17.800,
thrombosit 150.000
Hematuri makroskopis
Amilase darah 1.200 U/liter
PEMERIKSAAN TAMBAHAN
3/8/05
FAST
Foto Thoraks AP, BNO datar, BNO
tegak
MD-CT abdomen tgl 3/8/05
Ibu orang sakit menolak operasi, selain itu
o.s tidak boleh ditransfusi darah/produk
darah karena penganut Jehovah
APA TINDAKAN SELANJUTNYA ?
TINDAKAN LANJUT
4/8/05
Abdomen makin distensi, tekanan intra
abdominal 20 cm H2O = tekanan buli buli.
Tahikardi 110/menit
Subfebris 37,8
o
C
Tekanan darah 110/90, infus R/L 4 liter/24
jam maintenance
Bersedia dioperasi , syarat tanpa transfusi
Operasi laparotomi 4/8/05
Pra bedah Hb 7,5 g% hematokrit 21%
Transfusi Pasien Trauma
Trauma, Edisi VI (Felociano DV, Mattox KL, Moore, EE., tahun 2008)
Hb 7-15
Jika volume darah
normal
dan jantung sehat
|
Hb 7 -15 gm/dl
membawa O2
ke jaringan
sama banyak
Sunder-Plasman (1968)
Despite their belief regarding transfusion,
Jehovahs witnesses do not have higher
mortality rate after traumatic injury or
surgery if compared with other religious
groups
Transfusion requirements are often
overestimated increased morbidity and
mortality is rarely observed in pts with a Hb >
7 g/dL
The acute hemoglobin threshold for
cardiovascular collapse may be as low as
3g/dL to 5g/dL
INTRODUCTION
Varela et al in 2003 (J.Trauma 2003, 54: 967-
972)
Retrospective Cohort study of 550 pts,
concluded
That no increased risk of death after major
trauma compared with other religious
groups
Kitchens in 2003 (Am J med, 1993. 98: 1223-
1225)
A review of 16 reported series of Jehovah
s witness pts undergoing 1.404 surgical
procedures that normally require blood
transfusion
Conclusion : such refusal is not as
perilous as anticipated
CLINICAL CONSEQUENCE OF
TRANSFUSION REFUSAL
Recent data suggest that Jehovahs
witnesses may actually benefit with regard
to improved clinical outcomes
Vincent et al of 3.534 critically ill non-
Jehovahs witness pts admitted to 146
Western Europa ICUs during 2 week
periods in 1999
ICU length of stay, organ dysfunction, and
overall mortality were significantly higher
in critically ill pts who underwent
transfusion compared with similar non
transfused pts
29% vs 14.9% `
CLINICAL CONSEQUENCE OF
TRANSFUSION REFUSAL
Despite their belief regarding transfusion, Jehovahs
witnesses do not have higher mortality rate after
traumatic injury or surgery if compared with other
religious groups
Transfusion requirements are often overestimated
increased morbidity and mortality is rarely observed
in pts with a Hb > 7 g/dL
The acute hemoglobin threshold for cardiovascular
collapse may be as low as 3g/dL to 5g/dL
PROHIBITION OF BLOOD TRANSFUSION
AMONG JEHOVAHS WITNESSES
Pra bedah 4/8/05
Pasca bedah 11/8/05
Pulang 12/8/05
KASUS 2
Tn.DS
16 TAHUN
History
12-06-05 : Kecelakaan lalu lintas, tabrakan
sepeda motor dgn truk, terlempar
Klinis: Mild Head Injury + # maxilla LeFort 1 +
# antebrachii D (closed) + # femur D (closed)
+ abdominal bleeding + shock hemorrhagic
12-06-05: Damage Control Surgery 1
(packing) di RS A ruptur Liver Grade IV
medial dari gallbladder bed
Trauma Multiple
kecelakaan lalu
lintas,hemorrhagic
shock, perdarahan
intraabdominal
History
Post-op di ICU cepat stabil
15-06-05 : re-laparotomy bleeding
berhenti, angkat packing dipasang 2
buah drain di subhepatic & pelvis
Masalah post-op ke-2 : dari drain keluar
empedu 1500 cc/hari, terutama dari
pelvic, tachycardia, febris, gut failure
Os kemudian pindah ke RS Borromeus
29-06-05 dilakukan CT scan
Os. tetap sepsis, gut failure TPN
02/07/05
SIRS/sepsis segera dapat diatasi setelah CT guided
drainage
Operasi bertahap untuk koreksi
fraktur maxilla mulai dapat
dilakukan
Mengapa ?
1,5 bulan ini membaik, SIRS & Sepsis hilang,
# maxilla diperbaiki, # femur & antebrachii
direpair, bisa makan suplemen enteral
tetapi dari drain masih keluar empedu 1500
cc / hari
Sudah latihan mobilisasi
19/07/05
19/07/05
Diputuskan melakukan laparotomy elektif
untuk mengatasi kebocoran empedu
Operasi apa yang akan dilakukan ?
Penemuan intra-operatif ruptur lebar meliputi segmen 5-6 liver,
agaknya ada transeksi total portahepatis, CBD dan kandung
empedu utuh tetapi tidak berisi empedu
Sewaktu induksi narkose untuk laparotomy ke-3
Pasca Bedah
FOLLOW UP
2 minggu setelah
pulang
DCR In Practice, Vascular 08
Warko Karnadihardja
THE GOAL
The primary aim of this study
was to assess the ability to
use aggressive DCR to
enhance limb salvage
THE PROTOCOL OF DCR
INITIAL ASSESSMENT AND MANAGEMENT
OF COMBAT WOUNDED
First evaluated in a treatment resuscitation area
DCR was initiated in ED based on initial lab studies
and presentions vital signs and continued intra
operatively
Blood products were transfused within minutes of
arrival with an emerging release of 4 u PRBC, 2u
thawed AB plasma
A massive transfusion protocol consisting
standardized release and transfusion of PRBCs or
fresh WB, thawed AB plasma, cryoprecipitate and
platelets for pts in-extremis
Aggressive DCR maneuvers for successful
limb salvage in combat casualties with
vascular trauma
DCS & DCR
DCS: Is based on avoiding the lethal triad of
hypothermia, coagulopathy and progressive
acidosis in severely injured pts
(Stone, Strom and Feliciano the pioneer)
(Referensi) Cosgrift N, Moore EE, Sa uaia A et al. J. Trauma, 1997,
42: 857-861
DCR: Treats immediately the coagulopathy &
lethal triad of death as the patient was first
admitted
The essense of damage control is to achieve an
conclude an operative procedure before the
physiologic point of no return is reached
DCR + DC + RECONSTRUCTION +
AMPUTATION
CONCLUSION
The presenting in severe trauma
physiologic condition that has
classically led us to perform DCS may
no longer be a contraindication to
complex and prolonged extremity
vascular reconstruction when DCR
principles are employed
You might also like
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument51 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticedrhendyjuniorNo ratings yet
- Presentation 1Document25 pagesPresentation 1Nihar ShahNo ratings yet
- Goldenhar PDFDocument4 pagesGoldenhar PDFDaniel FernandezNo ratings yet
- ATLS Chapter Spine and Spinal Cord InjuryDocument29 pagesATLS Chapter Spine and Spinal Cord InjuryFahmi AnshoriNo ratings yet
- Anterior AbdominalDocument9 pagesAnterior AbdominalTAMBAKI EDMONDNo ratings yet
- Fasciotomy of Compartment SyndromeDocument19 pagesFasciotomy of Compartment Syndromeansuh22No ratings yet
- Chronic Limb Threatening IschemiaDocument35 pagesChronic Limb Threatening Ischemiasifatullah khanNo ratings yet
- Catatan DSTC CourseDocument3 pagesCatatan DSTC CourseHanny FadhilaNo ratings yet
- 2013 ASA Guidelines Difficult AirwayDocument20 pages2013 ASA Guidelines Difficult AirwayStacey WoodsNo ratings yet
- Algoritma Dan Prosedur Blunt Abdominal TraumaDocument1 pageAlgoritma Dan Prosedur Blunt Abdominal Traumareeves_coolNo ratings yet
- Acute Limb IschaemiaDocument32 pagesAcute Limb IschaemiaAnonymous 9wHscM100% (1)
- ATLS CirculationDocument19 pagesATLS Circulationfebriani pangaribuanNo ratings yet
- Orthopedic EmergenciesDocument63 pagesOrthopedic EmergenciesNasser AlQadhibNo ratings yet
- Chapter 5 ATLSDocument27 pagesChapter 5 ATLSUlfaa MutiaaNo ratings yet
- Kompartemen SindromDocument9 pagesKompartemen SindromPutri PratiwiNo ratings yet
- Perioperative Management 1203114432600412 4Document53 pagesPerioperative Management 1203114432600412 4polushkyNo ratings yet
- ATLS 8th EditionDocument50 pagesATLS 8th EditionPaolo VegaNo ratings yet
- 3.trauma Vaskular Richard SDocument79 pages3.trauma Vaskular Richard SAdang SunandarNo ratings yet
- Chronic Limb IschemiaDocument29 pagesChronic Limb IschemiaSadia NaveedNo ratings yet
- The Surgical Anatomy of The Nerve Laryngeal RecurrensDocument2 pagesThe Surgical Anatomy of The Nerve Laryngeal RecurrensvaNo ratings yet
- Staged Abdominal Re-Operation For Abdominal TraumaDocument7 pagesStaged Abdominal Re-Operation For Abdominal TraumaNovrianda Eka PutraNo ratings yet
- C. Anterior Cord SyndromeDocument1 pageC. Anterior Cord SyndromelubisinggidNo ratings yet
- Transhiatal EsophagectomyDocument12 pagesTranshiatal EsophagectomyprofarmahNo ratings yet
- Acute Osteomyelitis: Presented by Group - GDocument20 pagesAcute Osteomyelitis: Presented by Group - GSujan ThapaNo ratings yet
- Critical Limb IschemiaDocument29 pagesCritical Limb IschemiadockunNo ratings yet
- Surviving Sepsis Campaign 2016 Guidelines PresentationDocument30 pagesSurviving Sepsis Campaign 2016 Guidelines PresentationwisnusigitpratamaNo ratings yet
- ATLS in WomanDocument37 pagesATLS in WomanLukKaew Dhatchai CharoensilawathNo ratings yet
- Tracheostomy: Indications and ProcedureDocument10 pagesTracheostomy: Indications and ProcedureAinur AbdrakhmanovaNo ratings yet
- Dr. Kiki - Pengantar Trauma UpdateDocument20 pagesDr. Kiki - Pengantar Trauma UpdateRsud Malinau Ppk Blud100% (1)
- FOM STUDY GUIDE 3rd Block 1Document3 pagesFOM STUDY GUIDE 3rd Block 1Bernadine Cruz Par100% (1)
- U04 Fxs of Humeral ShaftDocument88 pagesU04 Fxs of Humeral Shaftadrian_mogosNo ratings yet
- Lefort 1 OsteotomyDocument36 pagesLefort 1 OsteotomyNidhi Jayan100% (2)
- Sialadenitis: K.Abhinaya. Bds 3 YearDocument14 pagesSialadenitis: K.Abhinaya. Bds 3 YearAsline JesicaNo ratings yet
- Minimal Invasive Surgery, Robotic, Natural Orifice Transluminal EndoscopicDocument59 pagesMinimal Invasive Surgery, Robotic, Natural Orifice Transluminal EndoscopicKahfi Rakhmadian KiraNo ratings yet
- OsteosarkomaDocument2 pagesOsteosarkomaLinawati DLNo ratings yet
- Multiple Endocrine Neoplasm Short Note by S.Wichien (SNG KKU)Document1 pageMultiple Endocrine Neoplasm Short Note by S.Wichien (SNG KKU)URo KkuNo ratings yet
- Patellar FracturesDocument26 pagesPatellar FracturesDavid VillanuevaNo ratings yet
- Mandible FX Slides 040526Document62 pagesMandible FX Slides 040526azharNo ratings yet
- Urogenital TumorDocument71 pagesUrogenital TumorJanet UngNo ratings yet
- Discuss Thoracic IncisionsDocument47 pagesDiscuss Thoracic IncisionsSucipto HartonoNo ratings yet
- Sejarah Dan Perkembangan Ilmu Bedah September 2017Document18 pagesSejarah Dan Perkembangan Ilmu Bedah September 2017Arief Fakhrizal100% (1)
- Parasitic Infections in SurgeryDocument24 pagesParasitic Infections in SurgerykhadzxNo ratings yet
- Procedural Skills (Awasir)Document34 pagesProcedural Skills (Awasir)Yousef TaqatqehNo ratings yet
- Iatrogenic Biliary InjuriesDocument15 pagesIatrogenic Biliary InjuriessolysanNo ratings yet
- Preventable Death: Dco: DR Thit Lwin School of Medicine UMSDocument56 pagesPreventable Death: Dco: DR Thit Lwin School of Medicine UMSStar CruiseNo ratings yet
- CA MammaeDocument30 pagesCA MammaeAlfiany SahrNo ratings yet
- Nervus Laryngeus RecurrensDocument5 pagesNervus Laryngeus RecurrensAri Julian SaputraNo ratings yet
- Jurnal Tyroid PDFDocument3 pagesJurnal Tyroid PDFVinnaNo ratings yet
- DR - Abeidi's Review FinalDocument157 pagesDR - Abeidi's Review FinalSandra AbboudNo ratings yet
- RIZ - Enterocutaneous FistulaDocument35 pagesRIZ - Enterocutaneous FistulaAdiwirya AristiaraNo ratings yet
- Orbitotomi MedscapeDocument9 pagesOrbitotomi MedscapeBonita AsyigahNo ratings yet
- 2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesDocument11 pages2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesOlteanu IonutNo ratings yet
- Indikasi ReplantasiDocument6 pagesIndikasi ReplantasiAngga Restu Pray YouGoNo ratings yet
- Thyroid Cancer Diagnosis and ManagementDocument45 pagesThyroid Cancer Diagnosis and Managementapi-3704562100% (1)
- Internal Medicine: Dr. Nindyasari Diajeng Larasati Tim UKMPPD FKU MalahayatiDocument209 pagesInternal Medicine: Dr. Nindyasari Diajeng Larasati Tim UKMPPD FKU MalahayatiSilvi Qiro'atul AiniNo ratings yet
- Volkmann's Ischemic ContractureDocument41 pagesVolkmann's Ischemic ContractureAayush AryalNo ratings yet
- Jurnal CA TyroidDocument4 pagesJurnal CA TyroidErvina ZelfiNo ratings yet
- Dermatoscopy and Skin Cancer, updated edition: A handbook for hunters of skin cancer and melanomaFrom EverandDermatoscopy and Skin Cancer, updated edition: A handbook for hunters of skin cancer and melanomaNo ratings yet
- Cotton and Williams' Practical Gastrointestinal Endoscopy: The FundamentalsFrom EverandCotton and Williams' Practical Gastrointestinal Endoscopy: The FundamentalsNo ratings yet
- FY 2010 INDR Indorama Synthetics TBKDocument57 pagesFY 2010 INDR Indorama Synthetics TBKDenny TombengNo ratings yet
- Surgical Wound Dehiscence Operative Wound DehiscenceDocument3 pagesSurgical Wound Dehiscence Operative Wound DehiscenceHendri GintingNo ratings yet
- Wound HealingDocument7 pagesWound HealingMarnia SulfianaNo ratings yet
- A Simplified Appendicitis ScoreDocument6 pagesA Simplified Appendicitis ScoreDenny TombengNo ratings yet
- Time - Special Edition - The Future of Medicine, 2023Document100 pagesTime - Special Edition - The Future of Medicine, 2023carlos samboniNo ratings yet
- Letters Combined (11 Referral, 2 Discharge, 1 Transfer)Document49 pagesLetters Combined (11 Referral, 2 Discharge, 1 Transfer)Faisal ImtiazNo ratings yet
- Case Saraf Bepri 5Document14 pagesCase Saraf Bepri 5Wen wenNo ratings yet
- The Active Pharmaceutical Ingredients (API) MarketDocument5 pagesThe Active Pharmaceutical Ingredients (API) Marketlek01No ratings yet
- National Leprosy Eradication Program (Nlep: Dr. Kanupriya ChaturvediDocument24 pagesNational Leprosy Eradication Program (Nlep: Dr. Kanupriya ChaturvediLavendra KunwarNo ratings yet
- Perforative PeritonitisDocument58 pagesPerforative PeritonitisSangeeta BSR82% (17)
- DyslpDocument141 pagesDyslpOmar AyashNo ratings yet
- Segundo - Medical Words - Compound NounsDocument0 pagesSegundo - Medical Words - Compound NounsCarlos Billot AyalaNo ratings yet
- Bupropion Hydrochloride (Drug Study)Document3 pagesBupropion Hydrochloride (Drug Study)Franz.thenurse6888100% (1)
- Definitions in Forensics and RadiologyDocument16 pagesDefinitions in Forensics and Radiologyabdul qadirNo ratings yet
- Guidance Document - Nutritional Care & Support For TB Patients in India PDFDocument107 pagesGuidance Document - Nutritional Care & Support For TB Patients in India PDFekalubisNo ratings yet
- Sadie Carpenter-Final DraftDocument5 pagesSadie Carpenter-Final Draftapi-609523204No ratings yet
- Exam Semi23423123132Document2 pagesExam Semi23423123132gwapoNo ratings yet
- SIGN 131 - Management of Schizophrenia: A National Clinical Guideline March 2013Document71 pagesSIGN 131 - Management of Schizophrenia: A National Clinical Guideline March 2013Septia Widya PratamaNo ratings yet
- Careers in Biomedical ScienceDocument24 pagesCareers in Biomedical ScienceEncik LaLaNo ratings yet
- 282173Document75 pages282173Shirley MoNo ratings yet
- Diagnosis and Treatment of Medial Epicondylitis of The ElbowDocument13 pagesDiagnosis and Treatment of Medial Epicondylitis of The ElbowSAKAI69No ratings yet
- Kaur, Diabetic Autonomic Neuropathy Pathogenesis and Treatment, 2014Document8 pagesKaur, Diabetic Autonomic Neuropathy Pathogenesis and Treatment, 2014elbueno21No ratings yet
- Retro VirDocument3 pagesRetro VirJericho MangalinNo ratings yet
- Nursing Diagnosis # 1 Acute Pain Related To Abdominal Incision.Document10 pagesNursing Diagnosis # 1 Acute Pain Related To Abdominal Incision.jhunanax100% (3)
- NCP RHDDocument4 pagesNCP RHDlouie john abilaNo ratings yet
- Pharmaceutical Reimbursement Access Manager in Austin TX Resume Brian BucklesDocument2 pagesPharmaceutical Reimbursement Access Manager in Austin TX Resume Brian BucklesBrian Buckles100% (1)
- Music I. Read The Following Questions Carefully and Write The Letter of The Correct Answer On Your Answer SheetDocument4 pagesMusic I. Read The Following Questions Carefully and Write The Letter of The Correct Answer On Your Answer SheetJohn Christopher Ping-ay Par IINo ratings yet
- Roleplay Discharge PlanningDocument3 pagesRoleplay Discharge PlanningAnonymous KQKONmD9H100% (1)
- Practice Questions - EDNDocument6 pagesPractice Questions - EDNKaren BlancoNo ratings yet
- Determination of Risk Factors For Drug - Related Problems - A Multidisciplinary Triangulation ProcessDocument7 pagesDetermination of Risk Factors For Drug - Related Problems - A Multidisciplinary Triangulation Processzenita reizaNo ratings yet
- Biology Project Class 12Document16 pagesBiology Project Class 12Anshika Singh100% (1)
- Garuda 762976Document5 pagesGaruda 762976bimaNo ratings yet
- Explanation 2020 1Document315 pagesExplanation 2020 1Reshma Shaji PnsNo ratings yet
- Therapeutic Management of Acute Respiratory Infections in AIEPIDocument12 pagesTherapeutic Management of Acute Respiratory Infections in AIEPIAndres RamirezNo ratings yet