Professional Documents
Culture Documents
Anatomy of Urinary Tract Baru
Uploaded by
Adya ArradikhaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anatomy of Urinary Tract Baru
Uploaded by
Adya ArradikhaCopyright:
Available Formats
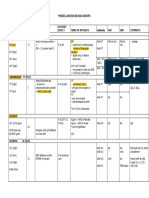
Anatomy of Urinary Tract
Kelompok 6
ANATOMY
THE KIDNEYS
The kidneys serve a number of important functions
required to maintain normal human physiologic
function.
maintaining fluid and electrolyte balance,
maintaining acid-base balance.
produce renincontrolling blood pressure,
produce erythropoietinaffecting red blood cell production.
calcium metabolism, (converting a precursor of vitamin D
1,25-dihydroxyvitamin D)
Grossly, the kidneys are bilaterally paired reddish
brown organs
weighs 150 g each in the male and 135 g in the
female.
10 to 12 cm vertically, 5 to 7 cm transversely, and 3
cm in the anteroposterior dimension
Because of compression by the liver, the right kidney
tends to be somewhat shorter and wider.
Anatomic Relationships
The position of the kidney within the
retroperitoneum varies greatly by side, degree of
inspiration, body position, and presence of anatomic
anomalies
The right kidney sits 1 to 2 cm lower than the left in
most individuals owing to displacement by the liver.
The right kidney 1st lumbar vertebra to the bottom
of the 3rd lumbar vertebra.
The left kidney 12th thoracic vertebra to the 3rd
lumbar vertebra.
Both kidneys have similar muscular surroundings.
Posteriorly, the diaphragm covers the upper third of
each kidney.
Medially the lower two thirds of the kidney lie
against the psoas muscle,
laterally the quadratus lumborum and aponeurosis
of the transversus abdominis.
Structures related to the posterior surface of the kidney
Anteriorly, the right kidney is bordered by a number
of structures.
Cranially, the upper pole lies against the liver
Also at the upper pole, the right adrenal gland is
encountered.
On the medial aspect, the descending duodenum is
intimately related to the medial aspect of the kidney
and hilar structures.
On the anterior aspect of the lower pole lies the
hepatic flexure of the colon.
The left kidney is bordered superiorly by the tail of
the pancreas with the splenic vessels adjacent to the
hilum and upper pole of the left kidney.
Also cranial to the upper pole is the left adrenal
gland and further superolaterally, the spleen.
The splenorenal ligament attaches the left kidney to
the spleen.
Superior to the pancreatic tail, the posterior gastric
wall can overlie the kidney.
Caudally, the kidney is covered by the splenic flexure
of the colon.
Structures related to the anterior surfaces of each kidney
Gerota's Fascia
This fascial layer encompasses the perirenal fat and
kidney and encloses the kidney on three sides:
superiorly, medially, and laterally.
Superiorly and laterally Gerota's fascia is closed, but
medially it extends across the midline to fuse with
the contralateral side.
Inferiorly, Gerota's fascia is not closed and remains
an open potential space.
Serves as an anatomic barrier to the spread of
malignancy as well as a means of containing
perinephric fluid collections.
Renal Vasculature
The renal pediclesingle artery and vein that enter
the kidney via the renal hilum .
branch from the aorta and inferior vena cava (2
nd
lumbar vertebra)
The vein is anterior to the artery.
The renal pelvis and ureter are located further
posterior to these vascular structures
Renal Artery
the right renal artery leaves the aorta and progresses
with a caudal slope under the IVC toward the right
kidney.
The left renal artery courses almost directly laterally
to the left kidney.
Both renal arteries move posteriorly as they enter the
kidney.
Also, both arteries have branches to the respective
adrenal gland, renal pelvis, and ureter
Segmental branches of the right renal artery demonstrated by
renal angiogram
Once in the renal sinus:
the segmental arterieslobar arteriesinterlobar
arteries (in the cortical columns of Bertin) arcuate
arteries (base of pyramids)Interlobular arteries
move radially afferent arteries glomeruli
efferent arteriole vasa recta
Renal Veins
post glomerular capillariesThe interlobular veins
arcuate interlobarlobarsegmental branches
renal vein
The renal vein is located directly anterior to the renal
artery
The right renal vein<The left renal vein
Additionally, the left renal vein receives the left
adrenal vein superiorly, lumbar vein posteriorly, and
left gonadal vein inferiorly.
The right renal vein typically does not receive any
branches.
Renal Lymphatics
On the left, primary lymphatic drainage is into the
left lateral para-aortic lymph nodes including nodes
anterior and posterior to the aorta between the
inferior mesenteric artery and the diaphragm.
On the right, drainage is into the right
interaortalcaval and right paracaval lymph nodes,
including nodes located anterior and posterior to the
vena cava, from the common iliac vessels to the
diaphragm.
Renal Collecting System
Microscopically, the renal collecting system
originates in the renal cortex at the glomerulus as
filtrate enters into Bowman's capsule.
Together the glomerular capillary network and
Bowman's capsule form the renal corpuscle
(malpighian corpuscle).
The glomerular capillary network is covered by
specialized epithelial cells called podocytes that,
along with the capillary epithelium, form a selective
barrier across which the urinary filtrate must pass.
The filtrate is initially collected in Bowman's capsule
and then moves to the proximal convoluted tubule.
The proximal tubule is composed of a thick cuboidal
epithelium covered by dense microvilli.
PCTloop of HenleDCTCTrenal papilla
Renal Papillae, Calyces, and Pelvis
Typically, there are 7 to 9 papillae per kidney
Each of these papillae is cupped by a minor calyx
After cupping an individual papillae, each minor calyx
narrows to an infundibulum.
Infundibuli combine to form two or three major calyceal
branches. These are frequently termed the upper,
middle, and lower pole calyces, and these calyces in turn
combine to form the renal pelvis.
The renal pelvis itself can vary greatly in size, ranging
from a small intrarenal pelvis to a large predominantly
extrarenal pelvis.
Eventually the pelvis narrows to form the ureteropelvic
junction, marking the beginning of the ureter.
Renal Innervation
Sympathetic8
th
thoracic 1
st
lumbar spinal segments
and then travel to the celiac and aorticorenal
gangliapostganglionic fibers travel to the kidney via the
autonomic plexus surrounding the renal artery.
Parasympathetic vagus nerve and travel with the
sympathetic fibers to the autonomic plexus along the
renal artery.
The primary function of the renal autonomic innervation
is vasomotor, with the sympathetics inducing
vasoconstriction and the parasympathetics causing
vasodilation.
THE URETERS
bilateral tubular structures
22 to 30 cm in length
wall composed of multiple layers
transitional epithelium.
lamina propria
smooth muscle (inner longitudinal and an outer circular layer)
adventitia (blood vessels and lymphatics)
Anatomic Relationships
The ureter begins at the ureteropelvic junction,
which lies posterior to the renal artery and vein.
It then progresses inferiorly along the anterior edge
of the psoas muscle.
Anteriorly, the right ureter is related to the
ascending colon, caecum, colonic mesentery, and
appendix.
The left ureter is closely related to the descending
and sigmoid colon and their accompanying
mesenteries.
three distinct narrowings: the ureteropelvic junction,
crossing of the iliac vessels, and the ureterovesical
junction
Ureteral Segmentation and Nomenclature
upper ureter extends from the renal pelvis to the
upper border of the sacrum.
The middle ureter comprises the segment from
the upper to the lower border of the sacrum.
The lower (distal or pelvic) ureter extends from
the lower border of the sacrum to the bladder
Blood Supply and Lymphatic Drainage
upper ureter renal artery, gonadal artery,
abdominal aorta, and common iliac artery.
distal ureter internal iliac artery or its branches,
especially the vesical and uterine arteries, also from
the middle rectal and vaginal arteries.
After reaching the ureter, the arterial vessels course
longitudinally within the periureteral adventitia in
an extensive anastomosing plexus.
The venous and lymphatic drainage of the ureter
parallels the arterial supply
In the pelvisinternal, external, and common iliac nodes
In the abdomen, the left para-aortic lymph nodes are the
primary drainage site for the left ureter whereas the
abdominal portion of the right ureter is drained
primarily to right paracaval and interaortocaval lymph
nodes
The upper ureter and renal pelvis join the renal
lymphatics and is identical to that of the ipsilateral
kidney
Ureteral Innervation
Normal ureteral peristalsis does not require outside
autonomic input but, rather, originates and is
propagated from intrinsic smooth muscle pacemaker
sites located in the minor calyces of the renal collecting
system.
The autonomic nervous system may exert some
modulating effect on this process, but the exact role is
unclear.
Sympathetic input10th thoracic through 2nd lumbar
spinal segments.
Parasympathetic input2nd through 4th sacral spinal
segments.
Pain Perception and Somatic Referral
Paintension (distention) in the renal capsule, renal
collecting system, or ureter.
Direct mucosal irritationalso stimulate
nociceptors.
Visceral-type pain referred to the sympathetic
distribution of the kidney and ureter (eighth thoracic
through second lumbar).
Bladder
When filled, the bladder has a capacity of
approximately 500 mL and assumes an ovoid shape.
The empty bladder is tetrahedral and is described as
having a superior surface with an apex at the
urachus, two inferolateral surfaces, and a
posteroinferior surface or base with the bladder neck
at the lowest point
The superior surfacecovered by peritoneum
Anteriorly, the peritoneum sweeps gently onto the
anterior abdominal wall
Posteriorly, the peritoneum passes to the level of the
seminal vesicles and meets the peritoneum on the
anterior rectum to form the rectovesical space.
Structure
The internal surface of the bladder is lined with
transitional epithelium,
This urothelium is usually six cells thick and rests on
a thin basement membrane.
Deep to this, the lamina propria forms a relatively
thick layer of fibroelastic connective tissue that
allows considerable distention.
This layer is traversed by numerous blood vessels
and contains smooth muscle fibers collected into a
poorly defined muscularis mucosa.
Beneath this layer lies the smooth muscle of the
bladder wall inner longitudinal, middle circular,
and outer longitudinal layers
Near the bladder neck, the detrusor muscle is clearly
separable into the three layers
Trigone
The triangle of smooth urothelium between the two
ureteral orifices and the internal urethral
meatustrigone of the bladder
The edges of this muscular sheet are thickened
between the ureteral orifices (the interureteric crest
or Mercier's bar) and between the ureters and the
internal urethral meatus (Bell's muscle).
Bladder Circulation
The main arteries supplying the bladder are
branches of the internal iliac arteries.
The superior vesical arteries supply anterosuperior
parts of the bladder.
In males, inferior vesical arteries supply the fundus
and neck of the bladder.
In females, the vaginal arteries replace the inferior
vesical arteries and send small branches to
posteroinferior parts of the bladder.
The obturator and inferior gluteal arteries also
supply small branches to the bladder
The veins of the bladder coalesce into the vesicle
plexus and drain into the internal iliac vein.
the lymphatic drainage passes to the external iliac
lymph nodes
Some anterior and lateral drainage may go through
the obturator and internal iliac nodes, whereas
portions of the bladder base and trigone may drain
into the internal and common iliac groups.
Bladder Innervation
The bladder wall is richly supplied with
parasympathetic cholinergic
the male bladder neck receives abundant
sympathetic innervation and expresses -adrenergic
receptors.
The female bladder neck has little adrenergic
innervation.
Prostate
weighs 18 g
3 cm in length, 4 cm in width, and 2 cm in depth;
and is traversed by the prostatic urethra
It is enclosed by a capsule composed of collagen,
elastin, and abundant smooth muscle.
PosteriorDenonvilliers' fascia
On the anterior endopelvic fascia.
Toward the apex, the puboprostatic ligaments extend
anteriorly to fix the prostate to the pubic bone
Structure
70% glandular elements and 30% fibromuscular
stroma.
The stroma is continuous with capsule and is
composed of collagen and abundant smooth muscle.
It encircles and invests the glands of the prostate and
contracts during ejaculation to express prostatic
secretions into the urethra
The urethra runs the length of the prostate and is
usually closest to its anterior surface.
It is lined by transitional epithelium, which may
extend into the prostatic ducts.
Vascular Supply
arises from the inferior vesical artery.
inferior vesical arteries but also the internal
pudendal and middle rectal arteries
2 branch:
Urethral branch
Capsular branch
Nerve Supply
Sympathetic and parasympathetic innervation from
the pelvic plexus travels to the prostate through the
cavernous nerves.
Parasympathetic nerves end at the acini and promote
secretion;
sympathetic fibers cause contraction of the smooth
muscle of the capsule and stroma.
Male Urethra
Merupakan saluran fibromusculer untuk jalan urine dari
Vesica Urinaria, dan pada pria juga merupakan jalan
sekret dari Vesicula Seminalis, Prostat, dan Glandula
Bulbourethralis.
Panjangnya 20 cm. Dimulai dari Collum Vesicae,
menembus kelenjar Prostat, Diafragma
Urogenitalis, kemudian melalui Corpus
Spongiosum Penis, yang berakhir di Glans Penis.
Urethra dibagi menjadi 3 bagian yaitu Pars Prostatica,
Pars Membranacea, dan Pars Cavernosa / Pars
Spongiosa.
Sedangkan bagian Urethra yang lumennya
melebar adalah Pars Prostatica, Fossa
Intrabulbaris ( pada Bulbus Urethrae ), dan Pada
Fossa Navicularis.
Female Urethra
Panjangnya 4 cm, berjalan ke ventrocaudal, mulai dari
Orificium Urethrae Internum ( pada Collum Vesicae )
sampai pada Orificium Urethrae Externum pada
Vestibulum Vaginae ( antara Introitus Vaginae dan
Clitoris ).
Urethrae melekat pada dinding ventral Vagina dan
difiksasi pada Os Pubis oleh beberapa serabut dari
Ligamentum Pubovesicalis dan oleh penebalan dari
Fascia Diafragma Urogenitalis Superior.
Female Urethra : Structure
Bagian dalam adalah mucosa dimana terdapat lubang
lubang Glandula Urethralis ( Lacunae Urethralis ), yang
dibagian caudalnya terdapat Ductus Glandula
Paraurethralis Scene ( Homolog dengan Prostat ), yang
bermuara pada sisi kanan dan kiri Orificium Urethrae
Externum.
Bagian tengah terdiri dari jaringan otot polos dan
bergaris yang berasal dari Musculus Pubovaginalis.
Bagian distalnya tidak ada jaringan ototnya.
Female Urethra
Vascularisasinya oleh :
Bagian cranial dari Arteri Vesicalis Inferior
Bagian media dari Arteri Vesicalis Inferior dan Arteri
Uterina
Bagian caudal dari Arteri Pudendalis Interna
Venanya dialirkan menuju Plexus Venosus Vesicalis
dan Vena Pudendalis Interna.
Aliran limfenya mengikuti Arteri Pudendalis
Interna, menuju ke Lnn. Iliaca Interna dan Lnn.
Iliaca Externa.
THANK YOU
You might also like
- Urinary System (Week 16)Document42 pagesUrinary System (Week 16)Krisha Mabel TabijeNo ratings yet
- Functional Anatomy of Renal System: by DR Amber IlyasDocument51 pagesFunctional Anatomy of Renal System: by DR Amber IlyasAlexah BanuagNo ratings yet
- Surgical Anatomy of Retroperitoneum, Kidneys and UretersDocument46 pagesSurgical Anatomy of Retroperitoneum, Kidneys and UretersDiana MarcusNo ratings yet
- Yusi - Anatomy of The Urinary Tract 2009 12-7Document129 pagesYusi - Anatomy of The Urinary Tract 2009 12-7abstabsNo ratings yet
- Seminar Cs 15 NovDocument24 pagesSeminar Cs 15 Novzeenatn1995No ratings yet
- Chapter 4 The Urinary SystemDocument43 pagesChapter 4 The Urinary Systemsomebody_maNo ratings yet
- DR Laxman Khanal Bpkihs 07-06-2013Document86 pagesDR Laxman Khanal Bpkihs 07-06-2013Bilal YimamNo ratings yet
- Kidney and UreterDocument9 pagesKidney and UreterDianne EstradaNo ratings yet
- Ureter AnatomyDocument8 pagesUreter AnatomyGhaly AmirNo ratings yet
- The Kidneys (Nephros) : FunctionsDocument6 pagesThe Kidneys (Nephros) : FunctionsOjambo FlaviaNo ratings yet
- The Anatomy of the Urinary SystemDocument44 pagesThe Anatomy of the Urinary SystemRahmawati HamudiNo ratings yet
- UT AnatomyDocument35 pagesUT AnatomyAngel SaraNo ratings yet
- Anatomy of Liver and Pancreas by Kazim AliDocument32 pagesAnatomy of Liver and Pancreas by Kazim AliAhmad KhanNo ratings yet
- Introduction to the Renal System and Kidney Anatomy (39Document10 pagesIntroduction to the Renal System and Kidney Anatomy (39Jeeson MichaelNo ratings yet
- Human Anatomy,: Renal /urinary SystemDocument62 pagesHuman Anatomy,: Renal /urinary Systemsapana shresthaNo ratings yet
- L31 - Renal SystemDocument30 pagesL31 - Renal SystemsairahhannahNo ratings yet
- Anatomy of The Kidney and UreterDocument6 pagesAnatomy of The Kidney and UreterMario Ivan De la Cruz LaraNo ratings yet
- Kidney, Suprarenal Gland, Ureter and Bladder AnatomyDocument46 pagesKidney, Suprarenal Gland, Ureter and Bladder AnatomyzahrazhfNo ratings yet
- Renal Anatomy and PhysiologyDocument15 pagesRenal Anatomy and PhysiologySapna JainNo ratings yet
- The Urinary System: Muh - Iqbal Basri Anatomy Department Hasanuddin UniversityDocument41 pagesThe Urinary System: Muh - Iqbal Basri Anatomy Department Hasanuddin Universityraynhard b. fandresNo ratings yet
- Anatomy, Abdomen and Pelvis, Kidneys: Statpearls (Internet) - Treasure Island (FL) : Statpearls Publishing 2022 JanDocument6 pagesAnatomy, Abdomen and Pelvis, Kidneys: Statpearls (Internet) - Treasure Island (FL) : Statpearls Publishing 2022 Janvenus ohNo ratings yet
- LiverDocument3 pagesLiverMamunNo ratings yet
- Abdominal Visceral OrgansDocument5 pagesAbdominal Visceral OrgansYudi Kelsi KaharapNo ratings yet
- grp52 UTI DseDocument9 pagesgrp52 UTI DsekcdgrvnNo ratings yet
- Urinary System: Nurmila Sari Anatomi FKIK UIN Syarif Hidayatullah JakartaDocument44 pagesUrinary System: Nurmila Sari Anatomi FKIK UIN Syarif Hidayatullah JakartaSeptiara IqraNo ratings yet
- Marking Scheme For Ant 414 (Functional Anatomy of Abdomen, Pelvis and Perineum) For 2017/2018 SessionDocument5 pagesMarking Scheme For Ant 414 (Functional Anatomy of Abdomen, Pelvis and Perineum) For 2017/2018 SessionmomoduNo ratings yet
- UNIT 10 (Urinary System)Document6 pagesUNIT 10 (Urinary System)Workinesh Kaynabo KambaloNo ratings yet
- SGD 10Document38 pagesSGD 10Mohd Johari Mohd ShafuwanNo ratings yet
- Anatomy of UreterDocument19 pagesAnatomy of Ureterfabunmiopeyemiv23No ratings yet
- Kidneys and Urinary Systems ExplainedDocument40 pagesKidneys and Urinary Systems ExplainedOlaifa victorNo ratings yet
- Kidney AnatomyDocument55 pagesKidney AnatomyMohammad zreadNo ratings yet
- Liver:: Anatomy The Abdomen Liver and Gall BladderDocument5 pagesLiver:: Anatomy The Abdomen Liver and Gall BladderWaeel AbdullatifNo ratings yet
- The AortaDocument52 pagesThe Aortaviorel79No ratings yet
- Rectumanalcanal 221008135814 55d691e6Document42 pagesRectumanalcanal 221008135814 55d691e6Emmanuel AdemoNo ratings yet
- Problem 2.03Document12 pagesProblem 2.03DeirdreNo ratings yet
- KidneysDocument6 pagesKidneysAmbg GhalyNo ratings yet
- Anatomy of Esophagus and StomachDocument65 pagesAnatomy of Esophagus and Stomachmackiecc100% (2)
- RectumDocument43 pagesRectummidhunramesh007100% (4)
- Kidney Anatomy and DevelopmentDocument12 pagesKidney Anatomy and DevelopmentErum IsmailNo ratings yet
- Urinary Organs - MahasiswaDocument43 pagesUrinary Organs - MahasiswaJendral Andi Wijaya KusumaNo ratings yet
- 1 - Anatomy of KidneysDocument22 pages1 - Anatomy of KidneysAHMAD YUNUSA GARBANo ratings yet
- Anatomy of The Kidney and Ureter: Basic ScienceDocument6 pagesAnatomy of The Kidney and Ureter: Basic ScienceAsfahani LatiefahNo ratings yet
- Anatomy of GALL BLADDER PANCREAS 2016Document32 pagesAnatomy of GALL BLADDER PANCREAS 2016Omar Ali AyoubkhanNo ratings yet
- Abiola Seminar in SpleenDocument23 pagesAbiola Seminar in SpleenBamgbose OpeyemiNo ratings yet
- Urinary System.Document33 pagesUrinary System.TakshikaNo ratings yet
- The Anatomy, Histology and Development of The Kidney PDFDocument14 pagesThe Anatomy, Histology and Development of The Kidney PDFredderdatNo ratings yet
- Radi 583 Paper Final Draft - HicksDocument26 pagesRadi 583 Paper Final Draft - Hicksapi-356393960No ratings yet
- Kidneys and Suprarenal Glands - DR Nto, Nto JDocument34 pagesKidneys and Suprarenal Glands - DR Nto, Nto JMary-precious EgboNo ratings yet
- Structures of The ForegutDocument13 pagesStructures of The ForegutJatan KothariNo ratings yet
- Visceras of AbdomenDocument91 pagesVisceras of AbdomenMusfera ImranNo ratings yet
- Clinical Anatomy of The Esophagus and StomachDocument82 pagesClinical Anatomy of The Esophagus and StomachmackieccNo ratings yet
- Pregnancy nutrition and bowel changesDocument25 pagesPregnancy nutrition and bowel changesMed LawNo ratings yet
- Large IntestineDocument29 pagesLarge IntestineHamza SultanNo ratings yet
- Colon Benign Conditions - Surgery NotesDocument85 pagesColon Benign Conditions - Surgery NotesNagulan ChanemougameNo ratings yet
- Abdomen (Repaired)Document174 pagesAbdomen (Repaired)Merellyn Hurtado PachecoNo ratings yet
- Grainger - Angiographic & Interventional AnatomyDocument5 pagesGrainger - Angiographic & Interventional AnatomympNo ratings yet
- SpleenDocument20 pagesSpleenjjjayakrishnan70No ratings yet
- Anatomy Notes: ProstateDocument4 pagesAnatomy Notes: ProstatekhawlabyNo ratings yet
- Anatomy SpleenDocument32 pagesAnatomy SpleenBijo K BennyNo ratings yet
- Diversity of MICROBIAL WORLDDocument47 pagesDiversity of MICROBIAL WORLDAdya ArradikhaNo ratings yet
- Surgical and Nosomial Infection: The SummaryDocument11 pagesSurgical and Nosomial Infection: The SummaryAdya ArradikhaNo ratings yet
- Patophysiology and Diagnosis of EDH & Basic PrinciplesDocument21 pagesPatophysiology and Diagnosis of EDH & Basic PrinciplesAdya ArradikhaNo ratings yet
- Shock, Body Responses To Hypovolemia Kel 6Document28 pagesShock, Body Responses To Hypovolemia Kel 6Adya ArradikhaNo ratings yet
- CM 07007312Document9 pagesCM 07007312Adya ArradikhaNo ratings yet
- Summary SamuelsDocument4 pagesSummary SamuelsAdya ArradikhaNo ratings yet
- Early Enteral NutritionDocument55 pagesEarly Enteral NutritionAdya ArradikhaNo ratings yet
- High Risk Neonatal Nursing CareDocument40 pagesHigh Risk Neonatal Nursing CareJaya PrabhaNo ratings yet
- How To Warm Up: Stage 1: Mobility ExercisesDocument7 pagesHow To Warm Up: Stage 1: Mobility Exercisesriz2010No ratings yet
- Journal Data Filtered By: Selected JCR Year: 2014 Selected Editions: SCIE, SSCIDocument247 pagesJournal Data Filtered By: Selected JCR Year: 2014 Selected Editions: SCIE, SSCImarceloicimoto2495No ratings yet
- Summary of CPR Steps 2016Document1 pageSummary of CPR Steps 2016Katerina TsNo ratings yet
- PENCERNAAN, ABSORPSI DAN METABOLISME KARBOHIDRATDocument29 pagesPENCERNAAN, ABSORPSI DAN METABOLISME KARBOHIDRATsenoNo ratings yet
- Grade: 8 Time: 60 Minutes Teacher: Ali Dokmak Subject: Biology Summer Reassessment Choose The Correct AnswerDocument5 pagesGrade: 8 Time: 60 Minutes Teacher: Ali Dokmak Subject: Biology Summer Reassessment Choose The Correct AnswerAli DokmakNo ratings yet
- Cardiac, Diabetic and General Range Drug ListDocument6 pagesCardiac, Diabetic and General Range Drug ListLisa PutriNo ratings yet
- Beginner PilatesDocument10 pagesBeginner PilatesVen Viv Gumpic100% (1)
- ATLSDocument6 pagesATLSYoga Wicaksana0% (1)
- Roth 10e Nclex Chapter 08Document3 pagesRoth 10e Nclex Chapter 08jennaaahhh100% (1)
- Plant and Animal Development: Lesson 2Document10 pagesPlant and Animal Development: Lesson 2hellohelloworldNo ratings yet
- Muscle Structure and FunctionsDocument59 pagesMuscle Structure and FunctionsThopu Umamaheswari100% (1)
- Synthesis of Adrenaline: Prepared by Sandesh Nair Roll No 204Document20 pagesSynthesis of Adrenaline: Prepared by Sandesh Nair Roll No 204Sreejith Menon0% (1)
- A To Z Orthodontics Vol 5 Soft Tissue Morphology1Document23 pagesA To Z Orthodontics Vol 5 Soft Tissue Morphology1Ishtiaq HasanNo ratings yet
- SummativeDocument2 pagesSummativeVan TotNo ratings yet
- Heredity AND Variation: Cell DivisionDocument21 pagesHeredity AND Variation: Cell Divisionshahadah_rahimNo ratings yet
- Brain and Behavior 4e PrefaceDocument26 pagesBrain and Behavior 4e Prefaceboka987No ratings yet
- Chapter 19Document34 pagesChapter 19Sahithya MNo ratings yet
- Acute Poisoning and Its AntidoteDocument10 pagesAcute Poisoning and Its AntidoteRachman UsmanNo ratings yet
- 2nd Anatomy QuizDocument2 pages2nd Anatomy QuizbevorsiNo ratings yet
- Cellular and Molecular Immunology - A PresentationDocument36 pagesCellular and Molecular Immunology - A PresentationShubham GuptaNo ratings yet
- Guidelines Angina FTDocument63 pagesGuidelines Angina FTMikhwanul JumarNo ratings yet
- The Teenage Brain Understanding TeenDocument5 pagesThe Teenage Brain Understanding TeenLuisLopez0% (1)
- Mangiferin From Mangifera Indica Fruits Reduces Post-Prandial GlucoseDocument6 pagesMangiferin From Mangifera Indica Fruits Reduces Post-Prandial GlucosePaulina Valderrama ArayaNo ratings yet
- Effects of Ethanol, Nicotine and Caffeine on Daphnia Heart RatesDocument6 pagesEffects of Ethanol, Nicotine and Caffeine on Daphnia Heart Ratesittoiram setagNo ratings yet
- Listening Is Twice As Hard As TalkingDocument9 pagesListening Is Twice As Hard As TalkingBridget Nothabo NdlovuNo ratings yet
- History and Drug StudyDocument4 pagesHistory and Drug StudyBel CortezNo ratings yet
- MISCELLANEOUS BLOOD GROUP ANTIGENSDocument4 pagesMISCELLANEOUS BLOOD GROUP ANTIGENSIan Leo SantosNo ratings yet
- Case Study (Placenta Previa)Document5 pagesCase Study (Placenta Previa)Jai - HoNo ratings yet
- Mindy MistakeDocument23 pagesMindy MistakeCine DadaNo ratings yet