Professional Documents
Culture Documents
Headache You Should Know - Surat
Uploaded by
Surat TanprawateOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Headache You Should Know - Surat
Uploaded by
Surat TanprawateCopyright:
Available Formats
Essential in headache
disorder
Surat Tanprawate, MD, MSc(Lond.), FRCP(T)
Headache Clinic, Department of Medicine
Chiangmai University
Facebook page: openneurons
The headache topics you
should know
1. International Classification of Headache Disorder-III
(ICHD-III)
2. Common headache disorder
1. Update evidence for migraine management
Secondary headache
Neuralgias
Primary headache
Migraine
TACs
TTH
Other
primary
headache
The Headache Classification
Classification of Headache Disorder
International Classification in Headache Disorder (ICHD)
ICHD-I: 1988
ICHD-II: 2004
IHC, Boston 2014: ICHD-III Beta version
Jes Olesen, MD, PhD University
of Copenhagen, Glostrup
Hospital, Denmark
http://www.ihs-classification.org/
Migraine
without aura
ICHD-III beta
Component
Algorithm approach
Headache complaint
History taking + Physical exam
Primary
headache
disorder
diagnosed by
ICHD-III Beta
criteria
Alarming s/s, Red
flag signs
S/S of
secondary
headache
Investigation to
detect serious
cause of
secondary
headache
Headache
attributed to .
Mixed headache
- Primary + Primary
- Primary +
Secondary
- Secondary +
secondary
Normal neurological
examination
Abnormal neurological
examination
Focal neurologic s/s
other than typical visual
or sensory aura
Papilledema
Temporal
profile
Concurrent
event
Provoking
activity
Age
Age> 50
Sudden onset
-SAH, ICH, mass
lesion (posterior
fossa)
Worsening
headache
-Mass lesion, SDH,
MOH
Pregnancy, post
partum
-Cerebral vein
thrombosis, carotid
dissection, pituitary
apoplexy
Headache with
cancer, HIV,
systemic illness
(fever, arteritis,
collagen vascular
disease)
Neck stiffness
Triggered by cough,
exertion or Valsava
-SAH, mass lesion
Worse in the
morning
-IICP
Worse on changing
position to upright
-Low CSF pressure
The headache topics you
should know
1. International Classification of Headache Disorder-III
(ICHD-III)
2. Common headache disorder
1. Primary headache disorder
Migraine, TACs, Other primary headache
2. Medication overuse headache (MOH)
Practical point of migraine
diagnosis
Primary headache disorder characterized by
recurrent headache accompanying with specific
phenomena...nausea/vomiting, aura,
photophobia/phonophobia
Migraine diagnostic criteria
A. 5 attacks fulfilling B-D (2 attacks for migraine with aura)
B. 4-72 hours (untreated/unsuccessfully treated)
C. 2/4 of following headache characters
1. unilateral
2. pulsating quality
3. moderate/severe pain intensity
4. aggravated by/cause avoid routine physical activity
D. 1/2 of following symptoms during headache
E. No other disorder
Classic migraine
(Migraine with aura)
The different phases of a migraine attack
Premonitory
symptoms
Premonitory
symptoms
prevalence =
87%-33%
Predictability of
headache at 72 hrs:
72%
Werner JB. Cephalalgia 2012. 33(13) 11171121
Somatosensory aura: Cheiro-oral numbness
Zig-zag lines (fortification)
Zig-zag lines in migraine aura
Visual Aura
Mosaic Illusion
Olomouc (c.1757) bastion fortress in today's
Czech Republic
Body distortion in Migraine
Pain characteristics and location of the acute migraine
attack: A study of 1283 migraine patients
Time of headache: morning in 18.7%, afternoon 13.5%, evening 4.0%,
during night 9.4%, and "anytime" 54.3%
Headache character: throbbing (73.5%), aching (73.8%), pressure
(75.4%), and stabbing (42.6%)
Headache increased by activity: 90.2% of patients
Headache location: eyes (67.1%), temporal (58.0%), and frontal
(55.9%), diffusely (17.5%) and vertex (24.1%)
Hemi-cranial location: 66.6% of patients,
Kelman L. Headache 2006 Jun;46(6):942-53.
Kelman L. Headache 2005 Sep;45(8):1038-47.
Genetic
Environmental
and factor
Cause
Pathophysiology of
acute migraine
Pathophysiology of episodic
and chronic migraine
- Genetic
: FHM, TREK
-Trigger factor
Pathophysiology
- Aura
- vasodilatation
- neurogenic inflammation
- peripheral and central
sensitization
- Trigemino vascular system
Neurotransmitter
- Serotonergic system
- Dopaminergic system
Structural and functional
brain change
- Brain stem activation
Clinical: chronic and transform
migraine, allodynia, neck pain
Anatomical: PAG, central
sensitization
episodic
constant
episodic become chronic
acute on chronic
Evolution of Migraine
Migraine is considered as a chronic
disorder with episodic attacks (CDEA)
No
migraine
LFEM
0-9 days of
headache/month
HFEM
10-14 days of
headache/month
Chronic
Migraine
Factor for Migraine progression
Conceptualized of clinical course of migraine
- Attack frequency
- Obesity
- Medication overuse
- Stressful life event
- Caffeine overuse
- Snoring
- Other pain
syndrome
- Gene
- Age/Sex
- Triggers
Bigal and Lipton Neurology 2008;71;848-855
The effective treatment for migraine
1.Non-pharmacologic + Pharmacologic therapy
2.Pharmacologic therapy: acute and prevention
1.Right drug-evidence based
2.Right dose-dose recommended
3.Right duration-4-6 months
Indication for preventive
treatment in migraine
Recurring migraine that significantly interferes with quality of
life
Frequency of migraine attacks > 1/weeks
Frequency of acute medication use > 2/week
Failure of, contraindication to, or trouble AE from acute
medication
Uncommon migraine: hemiplegic migraine, basilar migraine,
prolonged, disabling or frequent aura, or migrainous cerebral
infarction
Pract Neurol 2007; 7: 383393
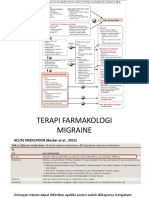
Non-specific
medication
Ever S, Afra J. Eur J Neurol 2009, 16:968-981
Migraine- specific medication
(Imigran)
(Zomig)
(Relpax)
Ergotamine/C
affeine
1 mg/100 mg
Caffeine
B
ER situation
Acute migraine attack
Valproic acid 300-800 mg iv
Chlorpromazine 25 mg
Ketorolac 60 mg im
Magnesium sulfate 1000 mg iv
Metoclopamide 10 mg iv
Tramadol iv
Status migrainosus
Dexamethasone 10 mg iv
Refractory case
Haloperidol 5 mg iv
Occipital nerve block
Ever S, Afra J. Eur J Neurol 2009, 16:968-981
Shrestha M. Arch Intern Med. 1996;156:1725-1728
Pamela D et al. J Head and Face Pain. 2005;45(7):899-903
Bigal ME. Cephalalgia 2002. 22(5):345-353
Evers, S et al. European Journal of Neurology 2009, 16: 968981
Triptans
(Imigran)
(Zomig)
(Relpax)
Sumatriptan 2.5
Zolmitriptan
Eletriptan
3.3
1.0-2.0
Time to peak plasma(h)
Level A: established as effective
Should be offered to patients requiring
migraine prophylaxis
Level B: probably effective
Should be considered for patients requiring
migraine prophylaxis
Vivalproex/sodium valproate 400-1000 mg/d
Metoprolol
47.5-200 mg/d
Petasites (butterbur)
50-75 mg bid
Propranolol 120-240 mg/d
Timolol 10-15 mg/d
Topiramate 25-200 mg/d
Amitryptyline
25-
150 mg/d
Fenoprofen
200-600 md tid
Feverfew 50-300 mg bid
Histamine 1-10 ng sc 2/wk
Ibuprofen 200 bid
Ketoprofen 50 mg tid
Magnesium 600 mg
Naproxen/naproxen sodium 550 mg bid
Riboflavin 400 mg/d
Venlafaxine 150 mg/d
Atenolol 100 mg/d
Level C: possible effective
May be considered for patients requiring
migraine prophylaxis
Level U: conflicting or inadequate
evidence
Insufficient data to support or refute use for
migraine prophylaxis
Candesartan 16 mg/d
Carbamazepine
600 mg/d
Clonidine
0.75-0.15 mg
bid
Guanfacine 0.5-1 mg/d
Lisinopril 10-20 mg/d
Nebivolol 5 mg/d
Pindolol
10
mg/d
Flubiprofen 200 mg/d
Mefenamic acid 500 mg/d
Coenzyme Q10 100 mg tid
Cyproheptadine 4 mg/d
Acetazolamide
Hyperbaric
oxygen
Aspirin Indomethacin
Bisoprolol Nicardipine
Coumadin Nifedipine
Cyclandelate Nimodipine
Fluoxetin Omega-3
Fluvoxamine Picotamide
Gabapentin Verapamil
Clonazepam Montelukast
Lamotrigine Nabumetone
Acebutolol Oxcarbazepine
Telmesartan
Medication-overuse
headache (MOH)
Diagnostic criteria:
A. Headache occurring on >15 days per month in a
patient with a pre-existing headache disorder
B. Regular overuse for >3 months of one or more
drugs that can be taken for acute and/or
symptomatic treatment of headache
C. Not better accounted for by another ICHD-3
diagnosis.
ICHD-III beta
1) Patients with MOH should be offered advice and teaching to
encourage withdrawal treatment. (B)
2) Abrupt vs tapering withdrawal : No evidence
For the overuse of analgesics, ergotamine
derivatives, or triptans, abrupt withdrawal is recommended.
For the overuse of opioids, benzodiazepines, or
barbiturates, tapering down of the medication should be
offered. (good practice point)
3) Type of withdrawal: success, relapse rate:
Inpatient = outpatient (A)
Ever S and Jensen R. Eur J Neurol 2011. 18:1115-1121
4) Inpatient withdrawal treatment in patient with
- opioid, benzodiazepine, or barbiturate overuse
- severe psychiatric
- medical comorbidity
- failure of a previous outpatient withdrawal treatment
(good practice point)
5) Individualized preventive medication should be started
at the first day of withdrawal treatment or even before if
applicable. (C)
Ever S and Jensen R. Eur J Neurol 2011. 18:1115-1121
6) Topiramate 100 mg (up to 200 mg maximum) per
day is probably effective in the treatment of MOH. (B)
7) Corticosteroids (at least 60 mg prednisone or
prednisolone) and amitriptyline (up to 50 mg) are
possibly effective in the treatment of withdrawal
symptoms. (good practice point)
Ever S and Jensen R. Eur J Neurol 2011. 18:1115-1121
Thank you
You might also like
- Pre-Extern Tutorial, 2013Document70 pagesPre-Extern Tutorial, 2013Surat TanprawateNo ratings yet
- Unusual Cause of Stroke and Its Mimicker, CNR Stroke Day 56Document53 pagesUnusual Cause of Stroke and Its Mimicker, CNR Stroke Day 56Surat Tanprawate100% (2)
- Pre-Extern Tutorial, 12Document55 pagesPre-Extern Tutorial, 12Surat TanprawateNo ratings yet
- Neurodegenerative Disorder, Jan 54Document75 pagesNeurodegenerative Disorder, Jan 54Surat Tanprawate100% (1)
- Surat Tanprawate, MD, FRCP Division of NeurologyDocument35 pagesSurat Tanprawate, MD, FRCP Division of NeurologyNEuRoLoGisT CoFFeeCuPNo ratings yet
- Anti Platlet and StrokeDocument25 pagesAnti Platlet and StrokeSurat TanprawateNo ratings yet
- Leptomenigeal Metastasis, MC Onco 54Document14 pagesLeptomenigeal Metastasis, MC Onco 54Surat TanprawateNo ratings yet
- Neurological Examination - Pre-Med - 401Document73 pagesNeurological Examination - Pre-Med - 401Surat Tanprawate100% (4)
- Approach To Stroke PatientDocument16 pagesApproach To Stroke PatientNEuRoLoGisT CoFFeeCuP100% (2)
- Status Epilepticus PathophysiologyDocument22 pagesStatus Epilepticus PathophysiologySurat TanprawateNo ratings yet
- Neuro-Ophthalmology - Third Year Student - 2018Document126 pagesNeuro-Ophthalmology - Third Year Student - 2018Surat TanprawateNo ratings yet
- Approach To Movement DisorderDocument12 pagesApproach To Movement DisorderSurat Tanprawate100% (1)
- PEDIA Neuromuscular DisorderDocument3 pagesPEDIA Neuromuscular DisorderThakoon TtsNo ratings yet
- MC: MG and The ThymomaDocument10 pagesMC: MG and The ThymomaSurat TanprawateNo ratings yet
- HIV Neurology, 2014Document62 pagesHIV Neurology, 2014Surat Tanprawate100% (2)
- The Neuropathy Resident Tutorial 54Document96 pagesThe Neuropathy Resident Tutorial 54Surat TanprawateNo ratings yet
- Headache Tutorial - Neuro Essential CMU2020Document66 pagesHeadache Tutorial - Neuro Essential CMU2020Surat Tanprawate100% (4)
- Resident Tutorial: AtaxiaDocument50 pagesResident Tutorial: AtaxiaNEuRoLoGisT CoFFeeCuP100% (4)
- Anatomic LocalizationDocument9 pagesAnatomic Localizationkid100% (1)
- Neuroradiology For PsychiatistDocument57 pagesNeuroradiology For PsychiatistSurat Tanprawate100% (1)
- DPP-4 Inhibitor and The BrainDocument19 pagesDPP-4 Inhibitor and The BrainSurat TanprawateNo ratings yet
- Approach To Neurological DiseaseDocument27 pagesApproach To Neurological DiseaseNEuRoLoGisT CoFFeeCuP100% (9)
- Approach To Neurological DiseaseDocument68 pagesApproach To Neurological DiseaseNEuRoLoGisT CoFFeeCuPNo ratings yet
- AIR FlimDocument69 pagesAIR FlimRapid MedicineNo ratings yet
- Headache Case Seminar - RCPTDocument25 pagesHeadache Case Seminar - RCPTSurat TanprawateNo ratings yet
- Basic Neuro For Medical StudentDocument65 pagesBasic Neuro For Medical StudentRapid MedicineNo ratings yet
- Rosh NeuroDocument11 pagesRosh NeuroSoni AliNo ratings yet
- Principle of ElectroDx by Dr. Angkana Nudsasarn, Chiang Mai UniversityDocument113 pagesPrinciple of ElectroDx by Dr. Angkana Nudsasarn, Chiang Mai UniversitySurat Tanprawate100% (3)
- Neurology LocalizationDocument6 pagesNeurology LocalizationPramod ThapaNo ratings yet
- HarrisonsDocument117 pagesHarrisonsEm TimbolNo ratings yet
- Medrano Neuro Notes 2.0Document22 pagesMedrano Neuro Notes 2.0roldan pantojaNo ratings yet
- Neuro Ophthalmology For Med Student - 2016Document120 pagesNeuro Ophthalmology For Med Student - 2016Surat Tanprawate100% (3)
- NEUROPrelims - History Taking in NeurologyDocument4 pagesNEUROPrelims - History Taking in NeurologyRenatoCosmeGalvanJuniorNo ratings yet
- Neurology Board 4330814Document64 pagesNeurology Board 4330814Snezana MihajlovicNo ratings yet
- Neurology Cram NotesDocument19 pagesNeurology Cram Notesrjh1895No ratings yet
- Neuro OphthalmologyDocument114 pagesNeuro OphthalmologySurat TanprawateNo ratings yet
- Approach To MyopathyDocument22 pagesApproach To MyopathySurat Tanprawate100% (2)
- Neurologic AssessmentDocument36 pagesNeurologic AssessmentJune Regina Mae DublasNo ratings yet
- Headache in Emergency ConditionDocument34 pagesHeadache in Emergency ConditionSurat TanprawateNo ratings yet
- Neurology MnemonicsDocument27 pagesNeurology MnemonicsMuhammad Luqman Nul Hakim100% (1)
- Lesion Localization in NeurologyDocument34 pagesLesion Localization in NeurologyValeria Leon AbadNo ratings yet
- Physical Exam For DiagnosisDocument61 pagesPhysical Exam For DiagnosisSurat Tanprawate100% (2)
- Epilepsy Guideline in AdultsDocument131 pagesEpilepsy Guideline in AdultsNEuRoLoGisT CoFFeeCuP100% (3)
- Autism Spectrum Disorders: Isabelle Rapin Seminar On Developmental DisordersDocument45 pagesAutism Spectrum Disorders: Isabelle Rapin Seminar On Developmental DisordersmeharunnisaNo ratings yet
- Neuroanatomy TractsDocument4 pagesNeuroanatomy TractsLoveHouseMDNo ratings yet
- Pre-Extern Tutorial, 14Document68 pagesPre-Extern Tutorial, 14Surat Tanprawate100% (2)
- Siiriraj Board Review Medicine - 4Document704 pagesSiiriraj Board Review Medicine - 4lippotein100% (3)
- Basic Movement Disorder ApproachDocument96 pagesBasic Movement Disorder ApproachSurat Tanprawate100% (18)
- Migraine Management, Songkra Hospital 13Document53 pagesMigraine Management, Songkra Hospital 13Surat Tanprawate50% (2)
- Neurology Shelf Exam Review - Part 2.newDocument14 pagesNeurology Shelf Exam Review - Part 2.newyogurtNo ratings yet
- DM and NeurologyDocument43 pagesDM and NeurologySurat TanprawateNo ratings yet
- Epilepsy GuidelinesDocument8 pagesEpilepsy GuidelinesSivaraj Raman100% (1)
- Localization of Brain Stem LesionsDocument35 pagesLocalization of Brain Stem LesionsHrishikesh Jha0% (1)
- Nontuberculous Mycobacterial Diseases: Nitiwat Chansuk Internal Medicine KKU July, 4 2011Document55 pagesNontuberculous Mycobacterial Diseases: Nitiwat Chansuk Internal Medicine KKU July, 4 2011Rapid MedicineNo ratings yet
- NeurologyDocument118 pagesNeurologykep1313No ratings yet
- Headache: by Yahya Ibrahim MBCHB 3. Dr. BacwaDocument54 pagesHeadache: by Yahya Ibrahim MBCHB 3. Dr. BacwaHarun MohamedNo ratings yet
- Algoritma Terapi (Becker Et Al., 2015)Document6 pagesAlgoritma Terapi (Becker Et Al., 2015)Elly PurwatiNo ratings yet
- HeadacheDocument92 pagesHeadacheMilap Shah100% (1)
- HeadacheDocument41 pagesHeadacheNatalia Khan100% (1)
- Headache - A Quick TutorialDocument7 pagesHeadache - A Quick TutorialLeilia FibrianasariNo ratings yet
- Headache Tutorial - Neuro Essential CMU2020Document66 pagesHeadache Tutorial - Neuro Essential CMU2020Surat Tanprawate100% (4)
- New Era in Migraine Management - 2019 - HatYaiDocument77 pagesNew Era in Migraine Management - 2019 - HatYaiSurat Tanprawate100% (3)
- Status Epilepticus PathophysiologyDocument22 pagesStatus Epilepticus PathophysiologySurat TanprawateNo ratings yet
- Neuro-Ophthalmology - Third Year Student - 2018Document126 pagesNeuro-Ophthalmology - Third Year Student - 2018Surat TanprawateNo ratings yet
- Neurological Examination - Pre-Med - 401Document73 pagesNeurological Examination - Pre-Med - 401Surat Tanprawate100% (4)
- Post Traumatic Headache Disorder - 2020Document26 pagesPost Traumatic Headache Disorder - 2020Surat TanprawateNo ratings yet
- Headche:Dizzy Med Stud - 2016Document51 pagesHeadche:Dizzy Med Stud - 2016Surat TanprawateNo ratings yet
- Status Epilepticus in Adult PDFDocument22 pagesStatus Epilepticus in Adult PDFSurat TanprawateNo ratings yet
- Headache Case Seminar - RCPTDocument25 pagesHeadache Case Seminar - RCPTSurat TanprawateNo ratings yet
- Neuro Ophthalmology For Med Student - 2016Document120 pagesNeuro Ophthalmology For Med Student - 2016Surat Tanprawate100% (3)
- Refractory-Primary-Headache Surat PornchaiDocument51 pagesRefractory-Primary-Headache Surat PornchaiSurat TanprawateNo ratings yet
- Migraine SubtypeDocument55 pagesMigraine SubtypeSurat Tanprawate100% (1)
- Headache Case Seminar - RCPTDocument25 pagesHeadache Case Seminar - RCPTSurat TanprawateNo ratings yet
- DPP-4 Inhibitor and The BrainDocument19 pagesDPP-4 Inhibitor and The BrainSurat TanprawateNo ratings yet
- Channelopathy of CNSDocument55 pagesChannelopathy of CNSSurat TanprawateNo ratings yet
- Headache in Emergency ConditionDocument34 pagesHeadache in Emergency ConditionSurat TanprawateNo ratings yet
- Ambulatory Conference: Approach To Parkinson's DiseaseDocument37 pagesAmbulatory Conference: Approach To Parkinson's DiseaseSurat Tanprawate100% (1)
- Physical Exam For DiagnosisDocument61 pagesPhysical Exam For DiagnosisSurat Tanprawate100% (2)
- Resident Tutorial 57-Part 1Document81 pagesResident Tutorial 57-Part 1Surat Tanprawate100% (1)
- Physical Exam For DiagnosisDocument61 pagesPhysical Exam For DiagnosisSurat Tanprawate100% (2)
- Basic Movement Disorder ApproachDocument96 pagesBasic Movement Disorder ApproachSurat Tanprawate100% (18)
- Neuro OphthalmologyDocument114 pagesNeuro OphthalmologySurat TanprawateNo ratings yet
- Acute Migraine Management, Chiangmai 2015Document60 pagesAcute Migraine Management, Chiangmai 2015Surat Tanprawate100% (1)
- PD SubtypeDocument11 pagesPD SubtypeSurat TanprawateNo ratings yet
- Role AEDs in Migraine PreventionDocument61 pagesRole AEDs in Migraine PreventionSurat TanprawateNo ratings yet
- Occam's Razor and Hickam's DictumDocument6 pagesOccam's Razor and Hickam's DictumSurat TanprawateNo ratings yet
- MS and NMO Update From ECTRIMS - Boston 2014 PDFDocument43 pagesMS and NMO Update From ECTRIMS - Boston 2014 PDFSurat TanprawateNo ratings yet
- MS and NMO Update From ECTRIMS - Boston 2014 PDFDocument43 pagesMS and NMO Update From ECTRIMS - Boston 2014 PDFSurat TanprawateNo ratings yet
- WN - jun14.BB M CohenDocument12 pagesWN - jun14.BB M CohenSurat TanprawateNo ratings yet
- Line Differential Protection Red670Document8 pagesLine Differential Protection Red670igorsfaceNo ratings yet
- Qasr Al Sarab Desert Resort Location Map June2012Document1 pageQasr Al Sarab Desert Resort Location Map June2012Anant GârgNo ratings yet
- SR No Service CodeDocument30 pagesSR No Service CodeShiva KrishnaNo ratings yet
- Segmentation of Blood Vessels Using Rule-Based and Machine-Learning-Based Methods: A ReviewDocument10 pagesSegmentation of Blood Vessels Using Rule-Based and Machine-Learning-Based Methods: A ReviewRainata PutraNo ratings yet
- OPTCL-Fin-Bhw-12Document51 pagesOPTCL-Fin-Bhw-12Bimal Kumar DashNo ratings yet
- Worksheet - 143760187HS-II, TUTORIAL ON CH-5Document14 pagesWorksheet - 143760187HS-II, TUTORIAL ON CH-5A MusaverNo ratings yet
- Clocks (New) PDFDocument5 pagesClocks (New) PDFAbhay DabhadeNo ratings yet
- Vanish Magic Magazine VANISH MAGIC MAGAZINE 58 May 2019Document118 pagesVanish Magic Magazine VANISH MAGIC MAGAZINE 58 May 2019mick byrnes100% (1)
- Manual GA 55 VSD Atlas CompresorDocument114 pagesManual GA 55 VSD Atlas Compresormondaxa_mme50% (4)
- Dairy Products Theory XIIDocument152 pagesDairy Products Theory XIIDskNo ratings yet
- Harmonic Analysis of Separately Excited DC Motor Drives Fed by Single Phase Controlled Rectifier and PWM RectifierDocument112 pagesHarmonic Analysis of Separately Excited DC Motor Drives Fed by Single Phase Controlled Rectifier and PWM RectifierGautam Umapathy0% (1)
- Islam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamDocument18 pagesIslam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamLoveth KonniaNo ratings yet
- Compiled LecsDocument24 pagesCompiled LecsNur SetsuNo ratings yet
- Recruitment and Selection in Canada 7Th by Catano Wiesner Full ChapterDocument22 pagesRecruitment and Selection in Canada 7Th by Catano Wiesner Full Chaptermary.jauregui841100% (51)
- Ecall Vs NG EcallDocument6 pagesEcall Vs NG EcallTrần Văn DũngNo ratings yet
- Conceptual Artist in Nigeria UNILAGDocument13 pagesConceptual Artist in Nigeria UNILAGAdelekan FortuneNo ratings yet
- T.A.T.U. - Waste Management - Digital BookletDocument14 pagesT.A.T.U. - Waste Management - Digital BookletMarieBLNo ratings yet
- Sap Ewm OverviewDocument11 pagesSap Ewm OverviewsachinNo ratings yet
- EDS-A-0101: Automotive Restricted Hazardous Substances For PartsDocument14 pagesEDS-A-0101: Automotive Restricted Hazardous Substances For PartsMuthu GaneshNo ratings yet
- Ap, Lrrsisal of Roentgenograph, Ic: I SsayDocument30 pagesAp, Lrrsisal of Roentgenograph, Ic: I SsayMindaugasStacevičiusNo ratings yet
- Maritime Management SystemsDocument105 pagesMaritime Management SystemsAndika AntakaNo ratings yet
- Integration ConceptDocument34 pagesIntegration ConceptJANELLA ALVAREZNo ratings yet
- Bagpipe LV 1-5Document228 pagesBagpipe LV 1-5Sathia Kdms100% (2)
- Pellicon 2 Validation Guide PDFDocument45 pagesPellicon 2 Validation Guide PDFtakwahs12135No ratings yet
- Diagnosis of TrypanosomiasisDocument82 pagesDiagnosis of TrypanosomiasisDrVijayata Choudhary100% (1)
- Armadio Presentation-2019Document45 pagesArmadio Presentation-2019Subhash Singh TomarNo ratings yet
- End of Summer Course Test August 2021Document16 pagesEnd of Summer Course Test August 2021Thanh Nguyen vanNo ratings yet
- Kaged Muscle Magazine Issue 1Document41 pagesKaged Muscle Magazine Issue 1hashimhafiz1100% (1)
- ContempoDocument4 pagesContempoPrincess Jonette YumulNo ratings yet
- CCNA Training New CCNA - RSTPDocument7 pagesCCNA Training New CCNA - RSTPokotete evidenceNo ratings yet