Professional Documents
Culture Documents
Fluids and Electrolytes: Presented by
Uploaded by
John Henry ValenciaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluids and Electrolytes: Presented by
Uploaded by
John Henry ValenciaCopyright:
Available Formats
FLUIDS AND ELECTROLYTES
Presented by:
John Henry O. Valencia, RN, RM
Master of Arts in Nursing
Case Study:
Youre taking report on John Miller, an American who had a
colectomy 2 days ago because of a ruptured diverticulus. You learn
that his heart rate has increased over the past 24 hours, yet his
blood pressure has been gradually falling and hes had marginal
urine output (30mL/Hour). Mr. Miller weighs 4kgs. More than before
surgery and he has generalized edema.
The health care team has decided not to increase Mr. Millers
maintenance IV infusion of lactated ringers solution. The nurse from
the previous shift says not to worry: His fluid will mobilize and hell
make urine soon.
Not sure what she means by that, you head off
to check out Mr. Millers condition for yourself.
During your assessment, you find that Mr. Miller has 2+
edema, warm skin and palpable peripheral pulses. His heart
rate is 108bpm, his blood pressure is 110/60mmHg and his
urine output remains marginal at 30mL/hr. Mr. Millers
abdomen is firm and distended, with hypoactive bowel sounds.
He says his pain is well controlled due to the pain medications
that was given.
Mr. Millers edema indicates that he has enough fluid in
his body. But his vital signs and urine output seems to tell a
different tale hypovolemia. How can you reconcile these
differences?
FLUIDS 101
Fluids brings nutrition and oxygen into the cells and remove wastes.
CELLS
ICF
ECF
Fluids within cells of body [major
intracellular electrolytes:
Potassium(K+), Magnesium (Mg +2)
Fluid outside cells; [major extracellular electrolytes:
Sodium (Na+), Chloride(Cl-)]; this is where
transportation of nutrients, oxygen, and waste
products occurs
Interstitial
Intravascular Transcellular:
Fluid between most cells
Fluid within blood vessels;
also called plasma
fluids of body including
urine, digestive
secretion,
cerebrospinal, pleural,
synovial, intraocular,
gonadal, pericardial
On the Move:
(i.e. movement of solutes, solvents across different extracellular locations)
OSMOSIS
From lower concentration to higher
concentration
Normal Osmolality of ICF and ECF: 275 295
mOsm/kg
DIFFUSION
From higher concentration to lower
concentration
ACTIVE TRANSPORT
molecules move across cell membranes against
concentration gradient; requires energy, e.g. Na
K pump
FLUID PRESSURES
HYDROSTATIC PRESSURE:
pushes fluid out of vessels into tissue space;
higher to lower pressure
due to water volume in vessels; greater in
arterial end
swelling: varicose veins, fluid overload, kidney
failure & CHF
OSMOTIC / ONCOTIC PRESSURE:
pulls fluid into vessels; from weaker
concentration to stronger concentration
from plasma proteins; greater in venous end
swelling: liver problems, nephrotic syndrome
Average Value: 25mmHg
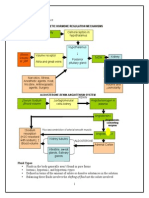
Mechanism of Regulating Body Fluids
and Electrolyte Balance
THIRST MECHANISM
Conscious desire for water
Major factor that determines
fluid intake
Initiated by the
osmoreceptors in
hypothalamus that are
stimulated by increase in
osmotic pressure of body
fluids
Also stimulated by a decrease
in the blood pressue through
the receptor of baroreceptor.
RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM
An Endocrine Pathway that regulates
fluid balance (extracellular volumes
including blood plasma, lymph and
interstitial fluids) as well as arterial
vasoconstriction.
Activation of RAAS leads to increase
fluid retention and increased blood
pressure
Many drugs are available which
interrupt different steps in the
system; they lower blood pressure
and reduces stress on the heart
Hypotension / Hypovolemia
Renal Hypoperfusion
Pressure sensed by cardiac
& Arterial Baroreceptors
Circulating
Catecholamines
Activity of Sympathetic nerves
innervating afferent arteriole
Stimulation of afferent arteriole
1-adrenergic receptors
Stretch of
baroreceptors in
afferent arteriole
wall
NaCl delivery to
Macula Densa
Renin Release from JGC in the
afferent arteriole = Angiotensin II
Liver normally synthesizes
angiotensinogen at a basal
rate, releasing it into the
blood
Angiotensinogen
Angiotensin I
Angiotensin II
RENIN
ACE
Angiotensin II constricts efferent arteriole
Fraction of water filtered out
Hydrostatic Pressure in Glomerulus
Protein concentration
of blood remaining in
glomerulus
Concentrated blood
moves from glomerulus
to peritubular
cappilaries
in peritubular
cappilaries
Peritubular
hydrostatic
pressure
GLOMERULOTUBULAR BALANCE
(Intrinsic renal mechanism not unique to RAAS)
*Only part of the mechanism represented below
Aldosterone
secretion from
adrenal cortex
Activity of NHE3
transporters in the
PCT
Systematic
Arteriolar
vasoconstriction
Insertion of ENaC
in principal cells
of CD
Reabsorption of Na into
the blood, drawing H2O
into the blood by
osmosis
Reabsorption of H2O directly into the
bloodstream
Excretion of
Potassium
BP
ACE: Angiotensin
Converting Enzymes
CD: Collecting Duct
PCT: Proximal
Convuluted Tubules
NHE3: Sodium-
Hydrogen Exchanger
ENaC: Epithelial
Sodium Channel
: Oncotic Pressure
LEGEND:
PHYSIOLOGY OF RENIN-
ANGIOTENSIN-ALDOSTERONE
SYSTEM (RAAS)
Angiotensinogen Angiotensin I Angiotensin II
Sympathetic division of ANS
Reabsorption of Na
+
, Cl
-
,
water; excretion of K
+
Aldosterone
Arterial
Vasoconstrictio
n
Vasopressin (ADH)
Water Reabsorption in
the collecting Duct
Angiotensin Converting Enzyme (ACE)
Renin
Physiology of
Angiotensin Conversion
in RAAS
Atrial Natriuretic Peptides
Stored in the cells of the Atria
Counteracts the effects of RAAS
by decreasing blood pressure
and reducing intravascular
blood volume
Suppresses serum renin
Decreases aldosterone release
from the adrenal glands
Increases GFR which increases
excretion of sodium and water
Vasodilatation
(causes afferent arterial vasodilation
and relaxes mesangial cells)
(inhibits sympathetic output
from cardiovascular center)
Amount Intake = Amount Eliminated
To eliminate waste produced
by metabolism, at least 500ml
of urine must be excreted
everyday.
DISORDERS
Disorder of Water and Sodium Metabolism
Sodium is the primary cation in the extracellular fluid
sodium content determine the osmolality in ECF
while osmolality gradient across cell membrane is the
driving force of water movement so disturbance of
sodium is always accompanied with water
disturbance
BACK to Mr. Miller:
Mr. Miller is Experiencing THIRD-
SPACE FLUID SHIFTING
Please see PATHOPHYSIOLOGIC
BASIS on your handouts.
You might also like
- Shock - Types Pathophysiology and Management: DR - Ravichandra Kumar Anaesthesia ResidentDocument64 pagesShock - Types Pathophysiology and Management: DR - Ravichandra Kumar Anaesthesia ResidentHarika BandaruNo ratings yet
- Haemorrhagic Shock, Resuscitation and HaemodynamicsDocument31 pagesHaemorrhagic Shock, Resuscitation and HaemodynamicsNinaNo ratings yet
- Fluids & ElectrolytesDocument15 pagesFluids & Electrolytesarvinnnn100% (2)
- Pemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220Document137 pagesPemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220fahmi rosyadiNo ratings yet
- Fluid & Electrolytes Balance NewDocument21 pagesFluid & Electrolytes Balance NewPamela Ria Aguinaldo HensonNo ratings yet
- Fluid & ElectrolyteDocument26 pagesFluid & Electrolytesanjana bhatia100% (1)
- Kidney Anatomy & Physiology Modified. Anas ElianDocument11 pagesKidney Anatomy & Physiology Modified. Anas ElianAnas Abu ElianNo ratings yet
- Shock: Departemen Anestesiologi Dan Reanimasi Fakultas Kedokteran USUDocument54 pagesShock: Departemen Anestesiologi Dan Reanimasi Fakultas Kedokteran USURuki HartawanNo ratings yet
- NCM 3114 Electrolyte Imbalance-2Document21 pagesNCM 3114 Electrolyte Imbalance-2Nicole Sherry M. CHEENo ratings yet
- Compensatory Mechanism of Circulatory ShockDocument29 pagesCompensatory Mechanism of Circulatory ShockWan Razin Wan Hassan100% (1)
- Screenshot 2023-03-17 at 12.32.32 AMDocument1 pageScreenshot 2023-03-17 at 12.32.32 AMRenadNo ratings yet
- (Pathophysiology, Types & MGT) : ShockDocument37 pages(Pathophysiology, Types & MGT) : ShockApriliani Nur Puspita SariNo ratings yet
- ReninDocument3 pagesReninAli GalaNo ratings yet
- Fluid and Electrolytes: Ma. Medine L. Amorsolo RN ManDocument29 pagesFluid and Electrolytes: Ma. Medine L. Amorsolo RN ManMichael Baylon Dueñas100% (1)
- Shock: DR Vishwabharathi TDocument51 pagesShock: DR Vishwabharathi TSumaNo ratings yet
- Fluids and ElectrolytesDocument7 pagesFluids and ElectrolytesNeweeJoonYowNo ratings yet
- CVS Pathophysiology: Components, Regulation and HypertensionDocument24 pagesCVS Pathophysiology: Components, Regulation and HypertensionVikash KushwahaNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- Fluids & Electrolytes: A. 2 Body CompartmentsDocument5 pagesFluids & Electrolytes: A. 2 Body CompartmentsJULIUS ART VINCENT A. PADINITNo ratings yet
- Special CirculationsDocument29 pagesSpecial Circulationslessank12100% (1)
- 10 CLS 382 443 Electrolytes I Na and Fluid Balance FINALDocument16 pages10 CLS 382 443 Electrolytes I Na and Fluid Balance FINALamalNo ratings yet
- Emd166 Slide Shock-1Document53 pagesEmd166 Slide Shock-1THuthi MUktiNo ratings yet
- 3 - Mechanical Ventilation - Trisna PrasDocument47 pages3 - Mechanical Ventilation - Trisna PraspuspwNo ratings yet
- Renal Notes Unit 1Document66 pagesRenal Notes Unit 1Zha-Raa'iaam L SamoriNo ratings yet
- SHOCKDocument28 pagesSHOCKMohammad Azzlan Abd RahmanNo ratings yet
- Unit 3 Blood As A Transport MediumDocument43 pagesUnit 3 Blood As A Transport MediumKemoy FrancisNo ratings yet
- Sistem SirkulasiDocument54 pagesSistem SirkulasiIhedi SacramentoNo ratings yet
- 4.shock & MonitoringDocument21 pages4.shock & MonitoringDr.G.Bhanu PrakashNo ratings yet
- Approach To ShockDocument19 pagesApproach To Shocksarath100% (1)
- Drugs Acting in CVSDocument63 pagesDrugs Acting in CVSMeghan Norico Cristuta100% (1)
- CBL HypertensionDocument23 pagesCBL HypertensionWan AswanNo ratings yet
- Shock in The Pediatric Patient: or Oxygen Don't Go Where The Blood Won't Flow!Document63 pagesShock in The Pediatric Patient: or Oxygen Don't Go Where The Blood Won't Flow!Nishanth BabuNo ratings yet
- Kegagalan Fungsi Jantung Dan SyockDocument74 pagesKegagalan Fungsi Jantung Dan SyockreavondNo ratings yet
- MTE Diagnosis and Manag ShockDocument52 pagesMTE Diagnosis and Manag ShockGarbha JmrsNo ratings yet
- Arterial Blood Pressure Regulation MechanismsDocument21 pagesArterial Blood Pressure Regulation Mechanismsnaresh sharmaNo ratings yet
- Shock: (Pathophysiology, Types & MGT)Document37 pagesShock: (Pathophysiology, Types & MGT)yusufNo ratings yet
- T2 Ans PDFDocument53 pagesT2 Ans PDFMiles HuiNo ratings yet
- Fluid ElectrolyteDocument115 pagesFluid ElectrolytePaul EbenezerNo ratings yet
- Diagnosis and Treatment of Shock: Dr. Refli Hasan SPPD, SPJP (K) FihaDocument37 pagesDiagnosis and Treatment of Shock: Dr. Refli Hasan SPPD, SPJP (K) FihaWinson ChitraNo ratings yet
- EDEMA - 2023-2024 - 15 ModuleDocument7 pagesEDEMA - 2023-2024 - 15 Modulerislariyas13No ratings yet
- Fluid and Electrolyte ImbalanceDocument27 pagesFluid and Electrolyte ImbalanceSimmi Sidhu100% (1)
- Medical Surgical Nursing: Fluids and ElectrolytesDocument28 pagesMedical Surgical Nursing: Fluids and ElectrolytesDhen MarcNo ratings yet
- Renal Physiol-OGY: DR I.GDocument55 pagesRenal Physiol-OGY: DR I.GAmanuel DinaNo ratings yet
- Anaesthesia in Renal Failure: Nadia Van Heerden Kimberley Hospital Complex 30 January 2015Document56 pagesAnaesthesia in Renal Failure: Nadia Van Heerden Kimberley Hospital Complex 30 January 2015Khaeril IrfanNo ratings yet
- Pleno Minggu 2 Blok 3.4Document84 pagesPleno Minggu 2 Blok 3.4Devi Yunita PurbaNo ratings yet
- RenalDocument8 pagesRenalLoislane RullNo ratings yet
- Lecture FMS 3 2015-2016 (Nata) - Pathophysiology and Pathogenesis of Shock (Restored)Document52 pagesLecture FMS 3 2015-2016 (Nata) - Pathophysiology and Pathogenesis of Shock (Restored)BritneyNo ratings yet
- Physiology 1 Fluid ElectrolyteDocument38 pagesPhysiology 1 Fluid ElectrolyteHaziq KamardinNo ratings yet
- Lung InflammationDocument44 pagesLung InflammationOnSolomonNo ratings yet
- 2long Term Regulation of Blood PressureDocument21 pages2long Term Regulation of Blood PressureamrendraNo ratings yet
- Management of ShockDocument18 pagesManagement of ShockObongsamuel IdiongNo ratings yet
- Dr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalDocument81 pagesDr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalvaishnaviNo ratings yet
- Conivaptan MedicalDocument38 pagesConivaptan MedicalSanjay NavaleNo ratings yet
- Kidneys BiochemistryDocument53 pagesKidneys BiochemistryMi PatelNo ratings yet
- Anti Diuretic Hormone Dr. EricDocument28 pagesAnti Diuretic Hormone Dr. EricIda Bagus Putu SwabawaNo ratings yet
- Pre Exam Surgical Notes 2Document166 pagesPre Exam Surgical Notes 2flor vickyNo ratings yet
- Renal Physiology NotesDocument6 pagesRenal Physiology Notescipa920% (1)
- Posterior Pituitary Hormones: ADH and OTCDocument39 pagesPosterior Pituitary Hormones: ADH and OTCMowlidAbdirahman Ali madaaleNo ratings yet
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- The Offender Commits Any Act of Lasciviousness or LewdnessDocument1 pageThe Offender Commits Any Act of Lasciviousness or LewdnessJohn Henry ValenciaNo ratings yet
- APP 1 FinalsDocument6 pagesAPP 1 FinalsJohn Henry ValenciaNo ratings yet
- Court Explains Lewd Acts and Environmental Circumstances in Amplayo vs People of PhilippinesDocument1 pageCourt Explains Lewd Acts and Environmental Circumstances in Amplayo vs People of PhilippinesJohn Henry ValenciaNo ratings yet
- RA 7721 - Liberalizing Entry and Scope of Foreign BanksDocument4 pagesRA 7721 - Liberalizing Entry and Scope of Foreign BanksRem RamirezNo ratings yet
- Remrev1 Midterms Reviewer TipsDocument24 pagesRemrev1 Midterms Reviewer TipsJohn Henry ValenciaNo ratings yet
- Border Anxieties - The Poetics and Predicaments of A Transnational Pollution-2Document16 pagesBorder Anxieties - The Poetics and Predicaments of A Transnational Pollution-2John Henry ValenciaNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- RA 8791 General Banking ActDocument22 pagesRA 8791 General Banking ActStephanie Mei100% (1)
- Labor 2 CasesDocument163 pagesLabor 2 CasesJohn Henry ValenciaNo ratings yet
- Transboundary PollutionDocument7 pagesTransboundary PollutionJohn Henry ValenciaNo ratings yet
- Court Explains Lewd Acts and Environmental Circumstances in Amplayo vs People of PhilippinesDocument1 pageCourt Explains Lewd Acts and Environmental Circumstances in Amplayo vs People of PhilippinesJohn Henry ValenciaNo ratings yet
- Evid Reflection PaperDocument2 pagesEvid Reflection PaperJohn Henry ValenciaNo ratings yet
- ADMELEC Drop Request PDFDocument1 pageADMELEC Drop Request PDFJohn Henry ValenciaNo ratings yet
- Peter Jones Human Rights Group Rights and Peoples Rights Human Rights Quarterly 21 - 1 PDFDocument23 pagesPeter Jones Human Rights Group Rights and Peoples Rights Human Rights Quarterly 21 - 1 PDFJohn Henry ValenciaNo ratings yet
- Evid Reflection PaperDocument2 pagesEvid Reflection PaperJohn Henry ValenciaNo ratings yet
- Grab Investigation and Feedback Report: Customer Name: Subject of Report: Report IDDocument1 pageGrab Investigation and Feedback Report: Customer Name: Subject of Report: Report IDJohn Henry ValenciaNo ratings yet
- Affidavit Lost Credit CardDocument2 pagesAffidavit Lost Credit CardJohn Henry ValenciaNo ratings yet
- Transboundary PollutionDocument7 pagesTransboundary PollutionJohn Henry ValenciaNo ratings yet
- Manila Port Services Vs American Home Assurance CorporationDocument2 pagesManila Port Services Vs American Home Assurance CorporationJohn Henry ValenciaNo ratings yet
- Henry Additional LoadDocument1 pageHenry Additional LoadJohn Henry ValenciaNo ratings yet
- Labor 2 CasesDocument118 pagesLabor 2 CasesJohn Henry ValenciaNo ratings yet
- 01 Doa Rosana Realty v. Molave TAWANTAWANsDocument3 pages01 Doa Rosana Realty v. Molave TAWANTAWANsJohn Henry ValenciaNo ratings yet
- Sps. Biesterbos v. CA de LUNADocument1 pageSps. Biesterbos v. CA de LUNAJohn Henry ValenciaNo ratings yet
- Criminal Procedure FlowchartDocument6 pagesCriminal Procedure FlowchartAizaFerrerEbina91% (136)
- RN Development Corporation Vs AII System Inc.Document1 pageRN Development Corporation Vs AII System Inc.John Henry ValenciaNo ratings yet
- Jazmin Espiritu Vs Vladimir LazaroDocument2 pagesJazmin Espiritu Vs Vladimir LazaroJohn Henry ValenciaNo ratings yet
- Fontanilla PNB v. Intestate Estate of de GuzmanDocument1 pageFontanilla PNB v. Intestate Estate of de GuzmanJohn Henry ValenciaNo ratings yet
- Raytheon Vs RouzieDocument1 pageRaytheon Vs RouzieJohn Henry ValenciaNo ratings yet
- Saguid Vs CA-civproDocument1 pageSaguid Vs CA-civproJohn Henry ValenciaNo ratings yet
- Nurse RoleDocument8 pagesNurse RoleMia100% (1)
- Orthotics - ProstheticsDocument8 pagesOrthotics - Prostheticsalpriani patrasNo ratings yet
- A A A A C C C C A A A A D D D D Eeee M M M M IIII C C C C S S S S C C C C IIII Eeee N N N N C C C C Eeee S S S SDocument3 pagesA A A A C C C C A A A A D D D D Eeee M M M M IIII C C C C S S S S C C C C IIII Eeee N N N N C C C C Eeee S S S SnelisaNo ratings yet
- 2nd Quarter Exam in Beauty Care - Nail Care ServicesDocument5 pages2nd Quarter Exam in Beauty Care - Nail Care ServicesMabeth Jabon Candido100% (16)
- Summit TM-40 MSDSDocument5 pagesSummit TM-40 MSDSVfuentes14No ratings yet
- Nepafenac Drug StudyDocument3 pagesNepafenac Drug StudyLucky Rius0% (1)
- Common Herbs For Natural Health-1Document284 pagesCommon Herbs For Natural Health-1muhteva83% (12)
- Paramedic: Duties and FunctionsDocument1 pageParamedic: Duties and FunctionsWhite BoxNo ratings yet
- Pharmacology OpioidDocument58 pagesPharmacology OpioidCitra Wulandari SofyanNo ratings yet
- Panacea Photonics User ManualDocument36 pagesPanacea Photonics User Manualliterarysh1980No ratings yet
- Neurontin (Gabapentin) : General InformationDocument3 pagesNeurontin (Gabapentin) : General InformationSoundarya SoundararajanNo ratings yet
- Case Study PneumoniaDocument14 pagesCase Study PneumoniaJester GalayNo ratings yet
- Fibromyalgia Syndrome Clinical Picture, Diagnosis, TreatmentDocument6 pagesFibromyalgia Syndrome Clinical Picture, Diagnosis, TreatmentCentral Asian StudiesNo ratings yet
- Cis 101 Research ReportDocument6 pagesCis 101 Research Reportleslie_arredondoNo ratings yet
- Sun Pharma Presentation on Problems and SolutionsDocument7 pagesSun Pharma Presentation on Problems and SolutionsKriti SoniNo ratings yet
- Pilo Herb Capsule for Piles ReliefDocument2 pagesPilo Herb Capsule for Piles ReliefOVVCMOULI100% (1)
- Digestive System FINALDocument43 pagesDigestive System FINALSean Lorenzo TumacderNo ratings yet
- Hospitals: Design Media Publishing LimitedDocument146 pagesHospitals: Design Media Publishing LimitedLuisa PintoNo ratings yet
- Block 4 OPP Lecture NotesDocument59 pagesBlock 4 OPP Lecture Notesjeremy_raineyNo ratings yet
- Nursing History and Development of NursingDocument11 pagesNursing History and Development of NursingNurses Professional EducationNo ratings yet
- Handbook of PEDIATRIC SURGERY PDFDocument43 pagesHandbook of PEDIATRIC SURGERY PDFPETERNo ratings yet
- HOSPITAL LISTINGDocument12 pagesHOSPITAL LISTINGSiddharth KumarNo ratings yet
- Antibacterial Resistance: DR Ance Roslina.,M.Kes Bagian Mikrobiologi Fk-Umsu 2019Document45 pagesAntibacterial Resistance: DR Ance Roslina.,M.Kes Bagian Mikrobiologi Fk-Umsu 2019RahmiNo ratings yet
- Reading Holter ECG Reports and Understanding Key FindingsDocument50 pagesReading Holter ECG Reports and Understanding Key FindingsOpptimuss Prime100% (2)
- SPIRULINA (Huge Health Benefits)Document10 pagesSPIRULINA (Huge Health Benefits)junver100% (1)
- Module 3 Practice ProblemsDocument11 pagesModule 3 Practice ProblemsAli Veer Ali Veer0% (1)
- 2478 13318 1 PB PDFDocument8 pages2478 13318 1 PB PDFAurellia MaharaniNo ratings yet
- Parasites of PoultryDocument8 pagesParasites of PoultrylisaNo ratings yet
- Funda ConceptsDocument201 pagesFunda ConceptsEncee Mian0% (1)
- The KT/V by Ionic Dialysance: Interpretation Limits: Original ArticleDocument7 pagesThe KT/V by Ionic Dialysance: Interpretation Limits: Original Articleahmed AlayoudNo ratings yet