Professional Documents
Culture Documents
Dka and Honk
Uploaded by
ignasachyntiaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dka and Honk
Uploaded by
ignasachyntiaCopyright:
Available Formats
Diabetic Ketoacidosis &
Hyperosmolar Hyperglycemic
State- Inpatient management
Susan Schayes M.D
Assistant Professor-CT
Family Medicine, Emory University
School of Medicine
2
High Impact Diseases
/
Jonas Brothers
3
Learning objectives
Define diagnostic criteria
for diabetic ketoacidosis
Define diagnostic criteria
for hyperosmolar
hyperglyemia
Understand the five key
components to the
treatment algorithm
.
In 1552 BC
Diabetes 1st Described In Writing
Earliest known record of diabetes
mentioned on 3
rd
Dynasty Eqyptian
papyrus by physician Hesy-Ra: mentions
polyuria as a symptom.
250 BC, Apollonius of Memphis coined the
name "diabetes meaning "to go through"
or siphon. He understood that the disease
drained more fluid than a person could
consume.
.
The Word Diabetes Mellitus
First Used
Gradually the Latin word for honey,
"mellitus," was added to diabetes because
it made the urine sweet.
Up to 11
th
century diabetes was commonly
diagnosed by water tasters who drank the
urine of those suspected of having
diabetes, as it was sweet-tasting.
Early Diabetes Discoveries
In the 1869, Paul Langerhans, a
German medical student announced
in a dissertation, that the pancreas
contains two systems of cells.
1889 Oskar Minkowski and Joseph
von Mering in France, removed the
pancreas from a dog to determine
the effect of an absent pancreas on
digestion
7
Fredrick Banting &
Charles Best
Boss leaves on vacation
May 1921
Banting and his assistant
Best isolate insulin from
dogs, and give it to
diabetic dogs.
Boss returns and is
skeptical that insulin
works
Try extract on
themselves, then on:
8
Leonard Thompson
The first patient to receive injections of
pancreatic extract on January 11, 1922. He was
14. The young Toronto resident had been
diabetic since 1919. He weighed only 65 pounds
and was about to slip into a coma and die. At
first he received Dr, F. Bantings and Dr. Charles
Bests extract. Two weeks later he used the
purified extract of Dr. J.B. Collip and
Thompson's symptoms began to disappear; his
blood sugar returned to normal and he was
brighter and stronger. Thompson lived another
13 years with the insulin. He died at the age of
27 due to pneumonia, a complication of his
diabetes
Type 1 vs. type 2 diabetes
Lambert P, et al. Medicine 2006; 34(2): 47-51
Nolan JJ. Medicine 2006; 34(2): 52-56
Features of type 2 diabetes
Usually presents in over-30s (but
also seen increasingly in
younger people)
Associated with
overweight/obesity
Onset is gradual and diagnosis
often missed (up to 50% of
cases)
Not associated with ketoacidosis,
though ketosis can occur
Immune markers in only 10%
Family history is often positive
with almost 100% concordance
in identical twins
Features of type 1 diabetes
Onset in
childhood/adolescence
Lean body habitus
Acute onset of osmotic
symptoms
Ketosis-prone
High levels of islet
autoantibodies
High prevalence of genetic
susceptibility
Goals of management
Manage symptoms
Prevent acute and late complications
Improve quality of life
Avoid premature diabetes-associated death
An individualized approach
Management
Glycemic
control
BP
Lipids
Patient
education
Lifestyle
(e.g. diet & exercise)
Foot care
Eye care Microalbuminuria
& kidneys
11
Normal Physiologic Insulin
Sensitivity and Cell Function
Produce Euglycemia
Pancreas
Normal Insulin Sensitivity
Liver
Euglycemia
Islet Cell Degranulation;
Insulin Released in Response to
Elevated Plasma Glucose
Muscle
Adipose Tissue
Increased Glucose
Transport
Decreased
Lipolysis
Glucose
Production
Glucose
Uptake
Normal Physiologic
Plasma Insulin
Decreased Glucose Output
Normal Cell Function
Decreased
Plasma FFA
12
Cell Dysfunction and Insulin
Resistance Produce Hyperglycemia in
Type 2 Diabetes
Pancreas
Insulin Resistance
Liver
Hyperglycemia
Islet Cell Degranulation;
Reduced Insulin Content
Muscle
Adipose Tissue
Decreased Glucose
Transport & Activity
(expression)
of GLUT4
Increased
Lipolysis
Glucose
Production
Glucose
Uptake
Reduced
Plasma Insulin
Increased Glucose Output
Cell Dysfunction
Elevated
Plasma FFA
13
Diabetic Ketoacidosis:
Key features: hyperglycemia, ketosis, acidosis
Clinical presentation: polyuria, polydipsia,
polyphagia, weakness, Kussmaulsrespirations,
nausea and vomiting
Can be mistaken for AGE
14
Diabetic Ketoacidosis
Cause: reduced insulin levels, decreased
glucose use, increased gluconeogenesis
Primarily affects TIDM, but can be T2DM
Precipitating factor: Infection,
Noncompliance,
Other acute event ie MI
15
Diabetic Ketoacidosis:
Treatment involves 5 key components:
Monitoring
Fluid resuscitation
Insulin and dextrose infusion
Electrolyte repletion
Treating underlying cause
PATHOGENESIS
Osmotic
Diuresis
Renal Hypoperfusion
Impaired Excretion of
Ketones & Hydrogen ions
Fluid & Electrolyte
Depletion
Vomiting
Acidosis Hyperglycemia
Glycosuria
Glucose
Ketones
Ketoacidosis
is a state of
uncontrolled catabolism
associated with
insulin deficiency.
CLINICAL FEATURES
Polyuria leading to Oliguria
Dehydration, Thirst
Hypotension, Tachycardia,
Peripheral circulatory failure
Ketosis
Hyperventilation
Vomiting
Abdominal pain (acute abdomen)
Drowsiness, Coma
METABOLIC FEATURES
Hyperglycemia
Glycosuria
Non-respiratory Acidosis
Ketonemia
Uremia
Hyperkalemia
Hypertriglyceridemia
Hemoconcentration
19
Dx Criteria for Mild DKA
Glucose > 250
Arterial pH 7.25-7.30
Serum bicarb 15-18 mEq
Urine and Serum ketones
B-hydroxybutyrate- high
Anion gap >10
Patient is alert
Trachtenbarg David, Diabetic Ketoacidosis, American Family Physician,
2005;71:1705-1714
20
Dx Criteria for Moderate DKA
Glucose > 250
Arterial pH 7.00-7.24
Serum bicarb 10 to <15 mEq
Urine and Serum ketones
B-hydroxybutyrate- high
Anion gap >12
Patient is alert/drowsy
Trachtenbarg David, Diabetic Ketoacidosis, American Family Physician,
2005;71:1705-1714
21
Dx Criteria for Severe DKA
Glucose > 250
Arterial pH <7.00
Serum bicarb <10 mEq
Urine and Serum ketones
B-hydroxybutyrate- high
Anion gap >12
Patient is stupor/coma
Trachtenbarg David, Diabetic Ketoacidosis, American Family Physician,
2005;71:1705-1714
22
Dx Criteria for HHS
Glucose > 600
Arterial pH <7.30
Serum bicarb <15 mEq
Urine and Serum ketones- small
B-hydroxybutyrate- n or elevated
Anion gap-variable
Patient is stupor/coma
Trachtenbarg David, Diabetic Ketoacidosis, American Family Physician,
2005;71:1705-1714
23
DKA- Monitoring
ICU
2 IVs, Oxygen, cardiac monitor,
continuous vitals, pulse ox
Foley to monitor I &O
Initially blood work every 1-2 hours
If pH is less that 6.9 be frightened
24
DKA- Monitoring
Standard blood work
Glucose, lytes with calculated anion gap, Mag
Bun & creatinine, calculate GFR
Beta-hydroxybutyrate or serum ketones
UA
CBC
EKG
Infection-cultures,chest xray
Cardiac status-cardiac enzymes
25
DKA- Fluids
Deficits are typically 100 ml per kg
Fluid replacement will lower glucose
Initial Tx usually fluid, fluid, fluid
Initial resuscitation 15-20 ml/kg stat for severe
dehydration with normal saline
1l,1l,1l,then 500ml X4 hours, reassess/reassess
Once glucose below 250, switch to
D5W/.45% N saline
26
Insulin
Initially 10 units R Insulin IV,
.15 units/kg
Insulin drip, most protocols 5-7
units per hour, .1 units/kg/hr
Patient to ICU
Stop insulin drip when sugar is
less than 250
27
Electrolytes- K
Whole body potassium deficits exist. (3-5
mmol/kg)
Acidosis increases K
Glucose + Insulin lowers K
Start K with K less than 5 mmol and adequate
urine output
If initial K less than 3.3 mmol
replete, and then start insulin when K above
3.3 mmol/L
28
Electrolytes- K
Commonly under repleted
Resident mistakenly uses the replacement of
potassium protocol, which vastly under repletes
potassium
Watch like a hawk!!!!
Replace/repete/replace/repete
29
Electrolytes- Mg
A serum deficit usually exists
of .5-1 mmol per L
Consider repleting if less than 1.8 mg/dL
30
DKA & HONK
Protocols- but use
Common sense which
is not common
You might also like
- Dka and HonkDocument30 pagesDka and HonkSobha KoduruNo ratings yet
- Diabetes KetoacidosisDocument35 pagesDiabetes KetoacidosisdaniejayanandNo ratings yet
- Diabetic Emergencies and ManagementDocument41 pagesDiabetic Emergencies and ManagementNali peterNo ratings yet
- Acute Care of Diabetes Mellitus: NURS 3071: Acute Health Challenges Feb. 12, 2019Document28 pagesAcute Care of Diabetes Mellitus: NURS 3071: Acute Health Challenges Feb. 12, 2019Savanna ChambersNo ratings yet
- Diabetes Mellitus: Fatimah ElianaDocument61 pagesDiabetes Mellitus: Fatimah ElianaOoy RokayahNo ratings yet
- Medical EmergenciesDocument12 pagesMedical EmergenciesBSN 2 - Sasis, Rusmaryte C.No ratings yet
- TCA Suppression and DM1Document22 pagesTCA Suppression and DM1Rubyrose TagumNo ratings yet
- Metabolic EmergenciesDocument53 pagesMetabolic EmergenciesWengel Redkiss100% (1)
- Diabetic Emergencies: Click To Edit Master Subtitle StyleDocument22 pagesDiabetic Emergencies: Click To Edit Master Subtitle StylenavenNo ratings yet
- Responses To Metabolic Gi Liver Alterations Compiled HandoutsDocument185 pagesResponses To Metabolic Gi Liver Alterations Compiled HandoutsJoanna Taylan100% (1)
- WEEK 15 DiabetesDocument68 pagesWEEK 15 DiabetesEditha LucasNo ratings yet
- Dka Vs Hhs Edit 1Document25 pagesDka Vs Hhs Edit 1Razeen RiyasatNo ratings yet
- DKA Diagnosis and TreatmentDocument16 pagesDKA Diagnosis and TreatmentDina M ElbakaryNo ratings yet
- Hiperosmolar Non KetotikDocument24 pagesHiperosmolar Non KetotikMunawwar AweNo ratings yet
- Project 1Document26 pagesProject 1sanju ShreeNo ratings yet
- Diabetic Ketoacidosis (DKA) : Cindy, Chelsea, Kim, JessaDocument11 pagesDiabetic Ketoacidosis (DKA) : Cindy, Chelsea, Kim, JessaChelsea RuthrauffNo ratings yet
- Diabetic Ketoacidosis (DKA) : Prepared By:yazan Masaied Instructor:Abed AsakrahDocument15 pagesDiabetic Ketoacidosis (DKA) : Prepared By:yazan Masaied Instructor:Abed Asakrahzyazan329No ratings yet
- COMPICATION of DMDocument42 pagesCOMPICATION of DMSaif AliNo ratings yet
- Management of Diabetes Emergencies''Document85 pagesManagement of Diabetes Emergencies''Princewill SeiyefaNo ratings yet
- Diabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineDocument68 pagesDiabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineAs ShahirahNo ratings yet
- Diabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineDocument68 pagesDiabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineAs ShahirahNo ratings yet
- DM Part 1 PDFDocument31 pagesDM Part 1 PDFShaila PiloNo ratings yet
- Diabetes Mellitus Types, Causes, SymptomsDocument12 pagesDiabetes Mellitus Types, Causes, SymptomssshiffanaNo ratings yet
- L11 Diabetes MellitusDocument61 pagesL11 Diabetes MellitusYosra —No ratings yet
- Nursing Care of Patients With Diabetes MellitusDocument43 pagesNursing Care of Patients With Diabetes MellitusRashida RuwaNo ratings yet
- DiabetesDocument32 pagesDiabetesaneeshajaiswalNo ratings yet
- Diabetes KetoacidosisDocument23 pagesDiabetes KetoacidosisSalman MajidNo ratings yet
- Diabetc Keto AcidosisDocument13 pagesDiabetc Keto AcidosisVijiNo ratings yet
- DIABETISDocument52 pagesDIABETISNeeraja M SureshNo ratings yet
- Hyperglycemic Crisis in Acute Care: Purwoko Sugeng HDocument49 pagesHyperglycemic Crisis in Acute Care: Purwoko Sugeng HBee DanielNo ratings yet
- Paeda DMDocument38 pagesPaeda DMAmanuel LemiNo ratings yet
- Complications of Diabetes: Maria Aslam Assistant Pofessor (UIDNS)Document47 pagesComplications of Diabetes: Maria Aslam Assistant Pofessor (UIDNS)haya farisNo ratings yet
- Nursing Care of Patients With Diabetes MellitusDocument11 pagesNursing Care of Patients With Diabetes MellitusMarcus, RN100% (32)
- Diabetic Coma: Kabera René, MD PGY III Resident Family and Community Medicine National University of RwandaDocument25 pagesDiabetic Coma: Kabera René, MD PGY III Resident Family and Community Medicine National University of RwandaKABERA RENENo ratings yet
- Dka and HHSDocument25 pagesDka and HHSMouhammad Dawoud100% (2)
- Diabetic Ketoacidosis (DKA) and Hyperosmolar Hyperglycemic State (HHS)Document25 pagesDiabetic Ketoacidosis (DKA) and Hyperosmolar Hyperglycemic State (HHS)Omar Abdillahi100% (1)
- Ketonuria: Huma Imtiaz MLTDocument14 pagesKetonuria: Huma Imtiaz MLTHabib UllahNo ratings yet
- Diabetes MellitusDocument17 pagesDiabetes MellitusRuqayya KobatteNo ratings yet
- Diabetic KetoacidosisDocument5 pagesDiabetic KetoacidosisJill Catherine Cabana100% (3)
- Diabetes BasicsDocument56 pagesDiabetes BasicsRuchi SainiNo ratings yet
- Diabetes Mellitus and Its Emergencies 1Document35 pagesDiabetes Mellitus and Its Emergencies 1Varun R'MenonNo ratings yet
- Hhns CabaisDocument34 pagesHhns CabaisArlyn Mendenilla100% (1)
- EMERGENCIES IN DM (KAD Dan HHS)Document26 pagesEMERGENCIES IN DM (KAD Dan HHS)ozNo ratings yet
- Acute Complications of DMDocument57 pagesAcute Complications of DMMalueth AnguiNo ratings yet
- Dr. Mohamed Ali Hamedh - DKA - 2023Document25 pagesDr. Mohamed Ali Hamedh - DKA - 2023ÁýáFáŕőúgNo ratings yet
- Diabetic EmergenciesDocument41 pagesDiabetic EmergenciesYuNa YoshinoyaNo ratings yet
- Byrne - Med II PresentationDocument20 pagesByrne - Med II Presentationapi-314835901No ratings yet
- Diabetes-Cho 2023 3rd Yr.Document37 pagesDiabetes-Cho 2023 3rd Yr.abdulrahmanbelewa96No ratings yet
- Hyperglycemic Emergencies: Boston University School of Medicine July, 2013 Marie Mcdonnell, MDDocument62 pagesHyperglycemic Emergencies: Boston University School of Medicine July, 2013 Marie Mcdonnell, MDBeyene FelekeNo ratings yet
- Diabetes KetoacidosisDocument27 pagesDiabetes Ketoacidosisyose rizal sinagaNo ratings yet
- Diabetes Nursing CareDocument39 pagesDiabetes Nursing Careapi-385715889% (9)
- Diabetic KetoacidosisDocument34 pagesDiabetic KetoacidosisasucelengbNo ratings yet
- NITHISHDocument96 pagesNITHISHsj computersNo ratings yet
- Diabetes Mellitus.U.iiDocument38 pagesDiabetes Mellitus.U.iitamtamtamtama0No ratings yet
- Diabetic Ketoacidosis: Presented by NG YHDocument32 pagesDiabetic Ketoacidosis: Presented by NG YHYuki NgNo ratings yet
- Understanding Acute Diabetic EmergenciesDocument41 pagesUnderstanding Acute Diabetic EmergenciesBeyene FelekeNo ratings yet
- Diabetic Recipes for One and TwoFrom EverandDiabetic Recipes for One and TwoRating: 3 out of 5 stars3/5 (1)
- Low Blood Sugar: The Nutritional Plan to Overcome Hypoglycaemia, with 60 RecipesFrom EverandLow Blood Sugar: The Nutritional Plan to Overcome Hypoglycaemia, with 60 RecipesNo ratings yet
- Diabetic Cooking for One and TwoFrom EverandDiabetic Cooking for One and TwoRating: 3 out of 5 stars3/5 (1)
- Solutions to Diabetes and Hypoglycemia (Translated): How to prevent and get rid of it in a natural way, without resorting to medicines but adopting a correct way of lifeFrom EverandSolutions to Diabetes and Hypoglycemia (Translated): How to prevent and get rid of it in a natural way, without resorting to medicines but adopting a correct way of lifeNo ratings yet
- Ucm 319628Document46 pagesUcm 319628ignasachyntiaNo ratings yet
- 120-Review of Internal Hernias. Radiographic and Clinical FindingsDocument20 pages120-Review of Internal Hernias. Radiographic and Clinical FindingsbobbylaksanaNo ratings yet
- Student Guide to Musculoskeletal PharmacologyDocument2 pagesStudent Guide to Musculoskeletal PharmacologyignasachyntiaNo ratings yet
- Needle Thoracocentesis AnastesiDocument5 pagesNeedle Thoracocentesis AnastesiignasachyntiaNo ratings yet
- Ade AmiDocument48 pagesAde AmiignasachyntiaNo ratings yet
- Ich Magistris, 2013Document8 pagesIch Magistris, 2013ignasachyntiaNo ratings yet
- Dr. Ery Olivianto, Sp.A: Division of Gastrohepatology, Child Health DepartmentDocument15 pagesDr. Ery Olivianto, Sp.A: Division of Gastrohepatology, Child Health DepartmentignasachyntiaNo ratings yet
- Intro To CHDDocument91 pagesIntro To CHDignasachyntiaNo ratings yet
- Bells PalsyDocument15 pagesBells PalsyDavid SugiartoNo ratings yet
- Study Design Epidemology-HoliDocument49 pagesStudy Design Epidemology-HoliignasachyntiaNo ratings yet
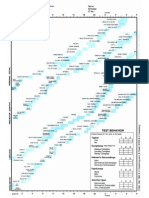
- Formato Denver IIDocument1 pageFormato Denver IIMelly AnidaNo ratings yet
- PPS - Revised Dengue Guidelines Fluid Management Oct 2012Document22 pagesPPS - Revised Dengue Guidelines Fluid Management Oct 2012lovelots1234100% (3)
- Perioperative NursingDocument32 pagesPerioperative NursingMaria Garcia Pimentel Vanguardia II100% (2)
- 4hyperosmolar Hyperglycemic State (HHS)Document121 pages4hyperosmolar Hyperglycemic State (HHS)desy f sarahNo ratings yet
- Managing Diabetes Through Medical, Nutritional and Nursing InterventionsDocument6 pagesManaging Diabetes Through Medical, Nutritional and Nursing InterventionsSittie Nashieva A. UsmanNo ratings yet
- ASPEN Clinical Nutrition Research in PandemicDocument19 pagesASPEN Clinical Nutrition Research in PandemicAlimah YasminNo ratings yet
- Proficiency Testbuilder 4th EditionDocument27 pagesProficiency Testbuilder 4th EditionNgan LeNo ratings yet
- Pathology of Diabetic Ketoacidosis - Romeo Rivera Jr.Document1 pagePathology of Diabetic Ketoacidosis - Romeo Rivera Jr.romeo riveraNo ratings yet
- Insulin Nursing ResponsibilitiesDocument9 pagesInsulin Nursing Responsibilitieskuro hanabusaNo ratings yet
- Diabetes 101: A Brief Overview of Diabetes and The American Diabetes AssociationDocument32 pagesDiabetes 101: A Brief Overview of Diabetes and The American Diabetes AssociationEliana MuisNo ratings yet
- IELTS Reading - DiabetesDocument3 pagesIELTS Reading - Diabeteshhos6190% (2)
- Metabolic and Endocrine ManagementDocument42 pagesMetabolic and Endocrine ManagementAlyssa MontimorNo ratings yet
- Diabetes Management: OverviewDocument20 pagesDiabetes Management: Overviewlaloo01No ratings yet
- Relation of A Variant in Adiponectin Gene (rs266729) With Metabolic Syndrome and Diabetes Mellitus Type 2 in Adult Obese SubjectsDocument7 pagesRelation of A Variant in Adiponectin Gene (rs266729) With Metabolic Syndrome and Diabetes Mellitus Type 2 in Adult Obese SubjectsVivi yenni aryantiNo ratings yet
- Beyond Pregnancy Understanding The Long-Term Implications of Gestational Diabetes MellitusDocument9 pagesBeyond Pregnancy Understanding The Long-Term Implications of Gestational Diabetes MellitusKIU PUBLICATION AND EXTENSIONNo ratings yet
- Standards of Medical Care in Diabetes - 2021: Abridged For Primary Care ProvidersDocument30 pagesStandards of Medical Care in Diabetes - 2021: Abridged For Primary Care Providersmỹ duyên đoànNo ratings yet
- Concept: Myocardial Infarction, AnginaDocument15 pagesConcept: Myocardial Infarction, AnginaHassen ZabalaNo ratings yet
- Concept MapDocument2 pagesConcept Mapapi-506386001No ratings yet
- NPH Insulin NPHDocument1 pageNPH Insulin NPHE100% (1)
- Steroid Tapering and Supportive Treatment Guidance V1.0 PDFDocument1 pageSteroid Tapering and Supportive Treatment Guidance V1.0 PDFNthutagaol TrusNo ratings yet
- Utsav2, Et AlDocument16 pagesUtsav2, Et Alnadin nNo ratings yet
- Winter Gerst 2006Document9 pagesWinter Gerst 2006Dr XNo ratings yet
- NozinanDocument18 pagesNozinanTom StNo ratings yet
- Nclex Questions - Medical Surgical NursingDocument15 pagesNclex Questions - Medical Surgical NursingRegine Gozo100% (1)
- Magnesium and Type 2 Diabetes: Mario Barbagallo, Ligia J DominguezDocument7 pagesMagnesium and Type 2 Diabetes: Mario Barbagallo, Ligia J DominguezbayuwinotoNo ratings yet
- Acarbose: Prescriber HighlightsDocument4 pagesAcarbose: Prescriber HighlightsDr. Anil Virani AlliedNo ratings yet
- Screening For Type 2 Diabetes Mellitus - UpToDateDocument17 pagesScreening For Type 2 Diabetes Mellitus - UpToDatePriscillaNo ratings yet
- Diabetic KetoacidosisDocument16 pagesDiabetic Ketoacidosisdrtpk100% (2)
- Ziabeen ThesisDocument109 pagesZiabeen ThesisHuma Hameed DogarNo ratings yet
- 5 Steps To Control High Blood SugarDocument56 pages5 Steps To Control High Blood Sugarjha.sofcon5941100% (1)
- Pathogenesis of Type 2 Diabetes MellitusDocument44 pagesPathogenesis of Type 2 Diabetes MellitusAsmat BurhanNo ratings yet
- DiabetesDocument11 pagesDiabetesRitesh SoorkiaNo ratings yet