Professional Documents
Culture Documents
Mortality Report 2
Uploaded by
E=MC2Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mortality Report 2
Uploaded by
E=MC2Copyright:
Available Formats
Mortality Report 2
Patients Particulars
Mrs. S,
78 years old, Malay lady
K/C/O: HPT, BA
( follow up at Hosp K.Kangsar)
Summary of History
Presented with:
- Epigastric pain, radiating to the back.
- SOB
- Lethargy x 2/52.
- Not ambulating due to weak x 1/52
- Fever , cough x 3/7
- LOA 1/52
Physical Examination
On Examination
Weak, dehydrated, mild tachypnoiec
BP: 124/80, PR:76, Temp: 36.3, SpO2: 100%
GCS 15/15, orientated to time/place/people
Per Abdomen:
soft, tender at epigastric,
Lungs: minimal crepts bibasal
CVS: DRNM
Investigations
Noted: Se amylase 632
Urine diastase 2834
Ca 3.43
RP: Urea 11.3; Na 129; K 2.1; Creat 141
LFT: AST 27; ALT 12; Alb 28; LDH 242;
se amylase 632, Ca 3.43
ABG: pH 7.47; pCO2 42; pO2 86;
sO2 97%; HCO2 30; BE 6
IMRIES SCORING:
Management
Treat as 1) Acute Pancreatitis
2) ARDS
3) ARF secondary to dehydration.
- K fast correction.
- IVD 8 pints NS/24H; Strict I/O charting
- Refer medical for AEBA 2 CAP, ARF
- Refer anest for ARDS and ICU care.
* Pt was transferred to ICU D2.
Progression In ICU
and ward
Day 1 (ICU)
Patients condition On HFMO2 10L/min
Not on inotropes
Examination GCS E2V4M5
BP 127/64; PR 77; CVP 9
SpO2 100%
Lungs: Bibasal crepts. A/E reduced B/L.
U/O: 300cc/H
Investigations K 2.0, Ca 3.24
Management KNBM
Cont IVD, keep CVP 8-10
Start IV Rocephine
For U/S HBS Urgent
U/S HBS Urgent (12.05.2012)
No sonographic evidence of cholelithiasis
Gallbladder is distended with regular outline.
There is sludge within the gall bladder.
Gallbladder wall not thickened.
Intrahepatic ducts, CBD and portal vein not dilated.
Pancreas not swollen.
Spleen normal.
Minimal ascites and right pleural effusion.
Imp: 1) No sonographic evidence of cholelithiasis
2) Fatty liver.
Day 2-10 (ICU)
Noted pt fitting, uprolling eyeballs,
hypersalivation and unresponsive to call; GCS
E1M4V1. Then was intubated and sedated.
Treat as pneumonia in septic shock
Was start inotropes and change to IV Cefepime 2g
BD.
Anest team request for CT Abdomen for
comfirmation of diagnosis; to look for pseudocyst
/ abscess / calcification of pancreas.
CECT Abdomen 18/5/2012
The pancreas not enlarged and homogenously
enhanced. No air pocket within to suggest
abscess collection. No calcification within and
the pancreatic duct is not dilated.
Minimal peropancreatic fluid collection and
streakiness noted at the body and tail of
pancreas.
Imp: 1) Features are of acute pancreatitis.
2) Fatty liver.
Day 11 Day 22 (ICU)
Tracheostomy done for prolonged ventilation, still
ventilated, not sedated, on inotropes.
Completed IV Cefepime 2g BD x 1/52.
Then has temp spike again, anest start back IV Unasyn 4.5g
QID.
Sputum C+S (21/5/12): Acinobacter species
Blood C+S: No Growth Obtain.
Urine C+S: No Growth Obtain.
Pt not responding to antibiotic (Given Unasyn for 9/7),
temp still spiking. Then anest change to IV Sulperazone.
Then was change to tachymask and transfer out to ward 17.
Day 23 (In Ward 17).
Sepsis controlled; BP 136/78, PR 97, T 37.
Tolerating RT feeding. Resolved pancreatitis.
On day 3 in ward 17; noted Pt tachypnoeic
and ill, reviewed by anest team, treat as
Ventilated Acquired Pneumonia.
Cont IV Sulperazone.
Blood C+S (in ward): So far no growth.
CXR: pneumonic changes, left pleural effusion.
Day 4 inn ward: patient collapse at 2.50am,
CPR commenced, adrenaline and atropine
given. CPR for 30 minutes, unable to revived
patient.
Asystole on cardiac monitor, B/L pupil fixed
and dilated. Peripheral and central pulse not
felt.
Pronounced death at 3.30am
Cause of death: Ventilated acquired
pneumonia.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- A Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)Document434 pagesA Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)AbdulraHman KhalEd100% (2)
- Abdominal Aortic AneurysmDocument20 pagesAbdominal Aortic AneurysmPortia Rose RodriguezNo ratings yet
- My Sister's KeeperDocument3 pagesMy Sister's Keeperbetsyk1No ratings yet
- Emotional Causes of CancerDocument6 pagesEmotional Causes of CancerstudiocrocNo ratings yet
- Mini Question Bank - Vety Sci - For Students PDFDocument106 pagesMini Question Bank - Vety Sci - For Students PDFRakesh Prajapati100% (3)
- Acute Care TestingDocument222 pagesAcute Care TestingAdel ChaabaneNo ratings yet
- Sample 20715Document16 pagesSample 20715Sachin KumarNo ratings yet
- Buku AnestesiDocument33 pagesBuku AnestesiAan AnharNo ratings yet
- r4f Pastest MnemonicsDocument23 pagesr4f Pastest MnemonicsplayuhzNo ratings yet
- Appendicitis: Navigation SearchDocument9 pagesAppendicitis: Navigation SearchE=MC2No ratings yet
- CHDDocument136 pagesCHDAfiqah So JasmiNo ratings yet
- BK Back Slab U Slab PDFDocument1 pageBK Back Slab U Slab PDFE=MC2No ratings yet
- BPJ 43 Urticaria Pages 6-13Document8 pagesBPJ 43 Urticaria Pages 6-13Zulis ChairaniNo ratings yet
- Analytic Study DesignsDocument43 pagesAnalytic Study DesignsKay KhineNo ratings yet
- AnencephalyDocument21 pagesAnencephalyE=MC2No ratings yet
- Hyaline Membrane DiseaseDocument20 pagesHyaline Membrane DiseaseE=MC2No ratings yet
- Urticaria and AngioedemaDocument10 pagesUrticaria and AngioedemaUchiha ItachiNo ratings yet
- Lower RTIDocument29 pagesLower RTIE=MC2No ratings yet
- Analytic Study DesignsDocument43 pagesAnalytic Study DesignsKay KhineNo ratings yet
- Research MethodologyDocument41 pagesResearch MethodologyRomit Machado83% (6)
- Pearls Nov Dec 2010Document2 pagesPearls Nov Dec 2010MohammadAwitNo ratings yet
- AppendectomyDocument3 pagesAppendectomyE=MC2No ratings yet
- Retinopathy of PrematurityDocument26 pagesRetinopathy of PrematurityE=MC2No ratings yet
- Oligohydramnios 11Document32 pagesOligohydramnios 11E=MC2No ratings yet
- Acute Stroke ManagementDocument22 pagesAcute Stroke ManagementE=MC2No ratings yet
- Amnoitic FluidDocument20 pagesAmnoitic FluidAnees SiddiquiNo ratings yet
- A Guide To Digital Radiographic DiagnosisDocument12 pagesA Guide To Digital Radiographic DiagnosisE=MC2No ratings yet
- A Guide To Digital Radiographic DiagnosisDocument12 pagesA Guide To Digital Radiographic DiagnosisE=MC2No ratings yet
- Amnoitic FluidDocument20 pagesAmnoitic FluidAnees SiddiquiNo ratings yet
- CTG Cinical Application of Cardiotocography Terence LaoDocument42 pagesCTG Cinical Application of Cardiotocography Terence LaoE=MC2No ratings yet
- P ArtographDocument40 pagesP ArtographE=MC2No ratings yet
- Relations Between Umbilical Troponin T Levels and Fetal DistressDocument5 pagesRelations Between Umbilical Troponin T Levels and Fetal DistressE=MC2No ratings yet
- Fetal Distress Causes, Signs, and TreatmentDocument16 pagesFetal Distress Causes, Signs, and TreatmentE=MC2No ratings yet
- Stages of LaborDocument11 pagesStages of LaborE=MC2No ratings yet
- Fetal Distress InpartumDocument3 pagesFetal Distress InpartumandartuasihombingNo ratings yet
- Idiopathic Nephrotic Syndrome: DR - Fahad Gadi, MD Pediatrics Demonstrator King Abdulaziz University Rabigh Medical SchoolDocument61 pagesIdiopathic Nephrotic Syndrome: DR - Fahad Gadi, MD Pediatrics Demonstrator King Abdulaziz University Rabigh Medical SchoolE=MC2No ratings yet
- Periodontal DressingDocument9 pagesPeriodontal DressingDilaC.FareshaNo ratings yet
- Combat Lifesaver Guide to One-Person Bag Valve Mask VentilationDocument1 pageCombat Lifesaver Guide to One-Person Bag Valve Mask VentilationSae TumNo ratings yet
- 13497-Texto Del Artículo-48998-1-10-20150925Document7 pages13497-Texto Del Artículo-48998-1-10-20150925Pipe Contecha BernatteNo ratings yet
- Acute otitis media in adults: An overviewDocument15 pagesAcute otitis media in adults: An overviewchristineNo ratings yet
- Meier Et Al, 1996Document4 pagesMeier Et Al, 1996boni_sebayangNo ratings yet
- Treatment Head LiceDocument26 pagesTreatment Head LiceCherry Amor Betita MadronaNo ratings yet
- Top 10 Pharma Companies in India 2022Document8 pagesTop 10 Pharma Companies in India 2022Royal MarathaNo ratings yet
- A Brief History of Evidence-Based Medicine in Four PeriodsDocument31 pagesA Brief History of Evidence-Based Medicine in Four PeriodsSaad MotawéaNo ratings yet
- Pathology of JointsDocument13 pagesPathology of JointswobblegobbleNo ratings yet
- Footnote To YouthDocument6 pagesFootnote To YouthVanityHughNo ratings yet
- Ducharme Et Al, 1996Document20 pagesDucharme Et Al, 1996GokushimakNo ratings yet
- Amir Bin Tamin 2Document3 pagesAmir Bin Tamin 2Akram KastiranNo ratings yet
- BHP Formula No 55 Refrence - Bioplasgen 20 Homeopathic Medicine For Skin DiseasesDocument2 pagesBHP Formula No 55 Refrence - Bioplasgen 20 Homeopathic Medicine For Skin DiseasesKazy Habibur RahmanNo ratings yet
- Medical Council of Inida Declaration Form 2010-2011for FacultyDocument9 pagesMedical Council of Inida Declaration Form 2010-2011for FacultydrtpkNo ratings yet
- MinoxidilDocument2 pagesMinoxidilHenna AhmedNo ratings yet
- Ayurveda Today IndexDocument15 pagesAyurveda Today IndexrajrajNo ratings yet
- Epidemiology of AsthmaDocument8 pagesEpidemiology of AsthmaMaria Alejandra Siachoque JaraNo ratings yet
- Emergency Welfare FormDocument2 pagesEmergency Welfare FormKristopher HarperNo ratings yet
- Isolating Staphylococcus SPDocument4 pagesIsolating Staphylococcus SPHani HairullaNo ratings yet
- Congenital Talipes Equino-Varus (Congenital Clubfoot) : Prof. Sohail Iqbal Sheikh Hod/Orthopaedics Iimct/PrhDocument66 pagesCongenital Talipes Equino-Varus (Congenital Clubfoot) : Prof. Sohail Iqbal Sheikh Hod/Orthopaedics Iimct/Prhawaisjinnah100% (1)
- Mink Dissection InstructionsDocument15 pagesMink Dissection InstructionsMark PenticuffNo ratings yet
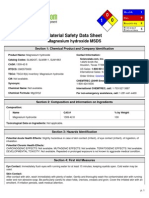
- Msds MgOHDocument5 pagesMsds MgOHCahyaGeriyanaNo ratings yet
- Periampullary TumorDocument22 pagesPeriampullary Tumorlovelots1234No ratings yet