Professional Documents
Culture Documents
NIPPV
Uploaded by
Anusha VergheseCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NIPPV
Uploaded by
Anusha VergheseCopyright:
Available Formats
Non-invasive Positive Pressure
Ventilation
Introdaction
* Nippv is recent phenomenon, mainly because of
advances in noninvasive interfaces and ventilator
modes
* NIPPV delivered o2 by nasal or oronasal mask
* The efficacy of noninvasive positive-pressure
Ventilation has been demonstrated for acute
pulmonary edema, for respiratory failure in
immunocompromised patients, and to facilitate
extubation in COPD patients.
* Patients who develop respiratory failure or who
refuse intubation are potentially good candidates for
noninvasive positive-pressure ventilation
*Several factors are vital to the success of noninvasive
positive-pressure ventilation: careful patient
selection; properly timed initiation; comfortable,
well-fitting interface; coaching and encouragement;
and careful monitoring.
*Noninvasive ventilation should be used to avert
endotracheal intubation rather than as an alternative to
it.
Definition
The application of positive pressure ventilation
without using an endotracheal tube.
or
As the provision of ventilatory assistance to the
lungs without an invasive artificial airway
History
Until the early 1960s, negative-pressure ventilation in the
form of tank ventilators was the most common type of
mechanical ventilation outside the anesthesia suite
With the introduction of nasal CPAP to treat obstructive sleep
apnea in the early 1980s,
NIPPV rapidly displaced negative-pressure ventilation as the
treatment of choice for chronic respiratory failure in patients with
neuromuscular and chest wall deformitie
The past 12 years, noninvasive ventilation has moved
from the outpatient to the inpatient setting, where it is
used to treat acute respiratory failure.
Non-invasiveVentialtion
1- Positive pressure
2-Negative Pressure
Advantage(NIPPV)
*Decreased direct upper airway trauma & bypass of
the upper airway defense mechanisms
*Allows patients to eat orally, vocalize normally, and
expectorate secretions.
* Noninvasive ventilation reduces infectious hospital
including pneumonia,sinusitis, and sepsis.
* lowers morbidity and mortality
* Shorten hospital length of stay, thus reducing costs.
Goals of NIV
Relieve symptoms
Reduce work of breathing
Offset the effect of i PEEP
Improve gas exchange
Minimize risk of barotrauma
Avoid intubation
Indication
Airway Obstruction
COPD
Asthma
Cystic fibrosis
Obstructive sleep apnea or obesity hypoventilation
Upper airway obstruction
Facilitation of weaning in COPD
Extubation failure in COPD
Indication
Hypoxemic Respiratory Failure
ARDS
Pneumonia
Trauma or burns
Acute pulmonary edema (use of CPAP)
Immuno compromised patients
Restrictive thoracic disorders
Post operative patients
Do-not-intubate patients
During bronchoscopy
Modes of Noninvasive Mechanical Ventilation
* volume ventilation, initial tidal volumes range from
10 to 15 mL.kg.
1-Pressure modes
2-volume modes
Pressure-cycled vents are better tolerated than volume-cycled vents
Pressure modes
**Continuous Positive Airway Pressure(CPAP)
Continuous positive airway pressure (CPAP) is a mode for invasive and
noninvasive mechanical ventilation.
It provides positive airway pressure throughout the respiratory cycle.
This static, positive pressure is maintained constantly during inhalation
and exhalation
CPAP is not a stand-alone mode of assisted mechanical ventilation. It is
equivalent to positive end-expiratory pressure (PEEP) and facilitates
inhalation by reducing pressure thresholds to initiate airflow.
This mode should never be used in patients who may have apneic
episodes because of the lack of a backup rate.
Pressure modes
Spontaneous Modes
In spontaneous mode, the airway pressure cycles between an inspiratory
positive airway pressure (IPAP) and an expiratory positive airway
pressure (EPAP).
This is commonly referred to as bilevel or biphasic positive airway
pressure (BL-PAP or BiPAP). The patient's inspiratory effort triggers the
switch from EPAP to IPAP. The limit during inspiration is the set level of
IPAP.
The inspiratory phase cycles off, and the machine switches back to EPAP
when it detects a cessation of patient effort, indicated by a decrease in
inspiratory flow rate, or a maximum inspiratory time is reached, typically
2-3 seconds.
Tidal volume (Vt) varies breath to breath and is determined by degree of
IPAP, patient effort, and lung compliance.
Spontaneous mode depends on patient effort to trigger inhalation. A
patient breathing at a low rate can develop a respiratory acidosis.
Spontaneous/timed (ST) mode
The trigger in the ST mode can be the patient's effort or an elapsed time
interval, predetermined by a set respiratory backup rate.
If the patient does not initiate a breath in the prescribed interval, then
IPAP is triggered. For machine-generated breaths, the ventilator cycles
back to EPAP based on a set inspiratory time.
For patient-initiated breaths, the ventilator cycles as it would in the
spontaneous mode.
Pressure modes
Conceptually:
One can consider BiPAP as PEEP with pressure support (PS).
The pressure during the inspiratory phase is termed IPAP and
is analogous to PS.
The pressure during the expiratory phase is termed EPAP and
is analogous to PEEP.
The IPAP is necessarily set higher than EPAP by a minimum
of 5cm H
2
O, and the difference between the two settings is
equivalent to the amount of PS provided
I nitiating Noninvasive Mechanical Ventilation
Either a face mask or a nasal mask can be used, but a nasal mask is
generally better tolerated.
A respiratory therapist must measure the patient to ensure a good fit and
seal.
Initially supply 3 to 5 cm H
2
O of CPAP with supplemental oxygen.
sequentially increase the CPAP pressure by 2 to 3 cm H
2
O increments
every 5 to 10 minutes (ABG-Pulse oximetry)
Recommended initial settings for BiPAP machines in the noninvasive
support of patients in respiratory distress or failure are IPAP of 8 cm H
2
O
and EPAP of 3 cm H
2
O, for a pressure support (IPAP minus EPAP) of 5
cm H
2
O.
The level of supplemental oxygen flowing into the circuit should be
governed by goal pulse oximetry and corroborated by ABG results as
necessary; it is appropriate to initiate therapy with 2 to 5 L/minute, but
this amount should be adjusted with each titration of IPAP or EPAP.
The intrinsic positive end-expiratory pressure
(PEEP
i
), or auto-PEEP, cannot be measured by
a noninvasive ventilator; therefore, EPAP
should generally be maintained below 8 to 10
cm H
2
O to be certain that it does not exceed
PEEP
i
in patients with obstructive lung disease.
The IPAP must always be set higher than EPAP
Conceptually:
Management Strategies
COPD
Main goal to decrease work of breathing (decreasing V/Q
mismatch) and provide adequate ventilation
Relatively low EPAP: 5-8cm H2O (assuming no obesity or
sleep disordered breathing)
Relatively moderate IPAP+EPAP: 10-14cm H2O
Goal to have at least a 5cm H2O differential between EPAP
and IPAP+EPAP; may need to go higher depending on
ventilation requirements
ie BiPAP 14/10 or 8/5
Management Strategies
CHF
Goal is to decrease work of breathing, decrease
afterload and decrease overall static pressure
Relatively moderate EPAP: 6-12 cm H2O
Relatively low IPAP+EPAP: 12-18cm H2O
Patient will benefit mostly with EPAP unless other
concurrent disease ( COPD, Obesity-
Hypoventilation)
Typical starting point: BiPAP 10/6
Management Strategies
Obesity-Hypoventilation Syndrome
Goal of therapy is to decrease work of breathing and
increase ventilation
Combined disease as >90% will also have concurrent
Obstraction sleep Apnea(OSA)
EPAP: usually on the higher side; enough to overcome
OSA and cardiopulm disease: ~10cmH2O, more for
bigger individuals
IPAP+EPAP: at least a 4cm H2O differential
Need to adjust according to ventilation requirements;
may benefit from back up rate
Management Strategies
Sleep Disordered Breathing
Most often post-op with known OSA or as a
complication associated with admit (CHF or
Obesity-Hypoventilation)
For elective admit with known OSA: usual
CPAP/BiPAP unless physiologic changes with acute
illness, surgery or narcotics.
Management Strategies
Neuromuscular Disease
Goal to decrease work of breathing, decrease
fatigue, assist ventilation
EPAP: usually low; 4-5cm H2O
IPAP+EPAP: at least 4cmH2O differential
May benefit from backup rate
Management Strategies
Other causes of respiratory failure
Pneumonia/ARDS
Cancer and respiratory failure
Post-op management
Settings depend on disease and other cardiopulmonary
disease
Most often used as a bridge to mechanical ventilation
or for pts DNR/DNI
Usually moderate settings: 12/8 or 14/8
Nasal masks are widely used for the administration of
CPAP or noninvasive ventilation, particularly for chronic
applications.
Nasal masks are usually better tolerated than full face masks for
long-term applications, because they cause less claustrophobia
and discomfort and allow eating,conversation, and expectoration.
The standard nasal mask is a triangular or cone-shaped
clear plastic device that fits over the nose and uses a soft cuff
that forms an air seal over the skin.
Full facemasks cover both the nose and the mouth
and are preferable to nasal masks in the acute
setting.
The efficacy of both nasal and oronasal masks in
lowering PaC02 and avoiding intubation is similar in the
acute setting,
but in a recent randomized,
patients tolerated the full facemask better because of reduced
air leakage through the mouth.
Selection of a comfortable mask that fits properly is key
to the success of noninvasive ventilation.
The full facemask
should be tried first in the acute setting, and if possible,
The mask straps are then tightened with the least tension
necessary to avoid excessive air leakage.
NIPPV masks
Nasal mask
NIPPV masks
Full face mask
NIPPV masks
Full face mask
Most of our patients!!
NIPPV machines
BiPAP
NIPPV machines
CPAP machine
Head straps hold the mask in place and are important for
patient comfort.
Straps attach at two to five points, depending
on the type of mask. More points of attachment add to
stability.
Head straps
OXYGENATION AND HUMIDIFICATION
Oxygen is titrated to achieve a desired oxygen saturation,
usually greater than 90% to 92%
Either by using oxygen
blenders on critical care and some bilevel ventilators or
By adjusting liter flow (up to 15 L/min) delivered via oxygen tubing connected
directly to the mask or ventilator circuit.
Bilevel ventilators
have limited oxygenation capabilities (maximal inspired oxygen fraction( %45 to
50)
so ventilators with oxygen blenders should be used for patients with hypoxemic
respiratory failure.
A heated humidifier should be used to prevent drying of the nasal passage and
oropharynx when the duration of application is anticipated to be more than a
few hours.
MONITORING
Once noninvasive ventilation is initiated, patients should be
closely monitored in a critical care unit or a step-down unit
until they are sufficiently stable to be moved to a regular
medical floor.
The aim of monitoring is
Relief of symptoms, reduced work of breathing, improved or stable
gas exchange, good patient-ventilator synchrony, and patient comfort
A drop in the respiratory rate with improved oxygen saturation or
improving pH with a lower PaCO2, reduce heart rate, within the first
1 to 2 hours portends a successful outcome.
The absence of these propitious signs indicates a poor response to
noninvasive ventilation
MONITORING OF PATIENTS RECEIVING
NON-INVASIVE VENTILATION IN ACUTE CARE SETTINGS
Location
Critical care or step-down unit
Medical or surgical ward if able to breathe unassisted for >20-30 min
"Eyeball test
Dyspnea
Comfort (mask, air pressure)
Anxiety
Asynchrony
Leaks
Vital signs
Respiratory and heart rates
Blood pressure
Continuous electrocardiography
Gas exchange
Continuous oximetry
Arterial blood gases (baseline after 2 h ,and as clinically indicated)
ADVERSE EFFECTS AND COMPLI CATI ONS in
NI V
The mask,
Discomfort and erythema or skin ulcers.
Airflow or pressure,
Conjunctival irritation. Ear pain. nasal or oral dryness .
Nasal congestion and discharge. Gastric insufflation.
Patient-ventilator asynchrony
Caused by high airflow is usually indicative of air leaking
through the mouth.
You might also like
- Noninvasive VentilationDocument6 pagesNoninvasive VentilationEma MagfirahNo ratings yet
- Care and Basic Settings of Portable Ventilator 2Document27 pagesCare and Basic Settings of Portable Ventilator 2febian_henryNo ratings yet
- Registered Respiratory TherapistDocument3 pagesRegistered Respiratory Therapistapi-76909521No ratings yet
- Respiratory Therapy Cave - Ventilator Graphics Cheat SheetDocument2 pagesRespiratory Therapy Cave - Ventilator Graphics Cheat SheetMarwa El-DegwiNo ratings yet
- Respiratory Therapist, NICU/ICUDocument5 pagesRespiratory Therapist, NICU/ICUapi-77517256No ratings yet
- Acute Coronary SyndromeDocument21 pagesAcute Coronary SyndromeNabil Mosharraf Hossain100% (2)
- PEEP (Positive-End Expiratory Pressure)Document5 pagesPEEP (Positive-End Expiratory Pressure)Valcrist BalderNo ratings yet
- COPD Acute Management ABCDEDocument11 pagesCOPD Acute Management ABCDESSNo ratings yet
- Critical Thinking in Respiratory Care Practice PDFDocument17 pagesCritical Thinking in Respiratory Care Practice PDFFernando MorenoNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- Ventilator GraphicsDocument38 pagesVentilator GraphicsShaliniNo ratings yet
- Basic VentilationDocument64 pagesBasic VentilationGBJ VisionNo ratings yet
- Bilevel Made Easy Nursingpdf LshieldsrrtDocument1 pageBilevel Made Easy Nursingpdf LshieldsrrtmilleralselmoNo ratings yet
- Fabian VentilatorDocument17 pagesFabian VentilatorRohana AnaNo ratings yet
- Pulmonary Function Testing1Document51 pagesPulmonary Function Testing1kusaarNo ratings yet
- Mechanical Ventilation TherapyDocument17 pagesMechanical Ventilation TherapyFaizal FlNo ratings yet
- Extubation CriteriaDocument17 pagesExtubation CriteriaOliver TabagNo ratings yet
- Acute Respiratory Distress SyndromeDocument30 pagesAcute Respiratory Distress SyndromeNikhil GhubadeNo ratings yet
- Overview of Respiratory Failure & Use of Mechanical VentilationDocument89 pagesOverview of Respiratory Failure & Use of Mechanical VentilationsheharyarNo ratings yet
- Ventilator WaveformsDocument37 pagesVentilator Waveformsfifa_0304535No ratings yet
- Patient-Ventilator Dyssynchrony in The Intensive Care Unit A PracticalDocument12 pagesPatient-Ventilator Dyssynchrony in The Intensive Care Unit A PracticalBrenda Serrano LaraNo ratings yet
- Respiratory Therapy PresentationDocument11 pagesRespiratory Therapy Presentation003cbty9No ratings yet
- Breathing and Exchange of GasesDocument5 pagesBreathing and Exchange of Gaseslpc4944No ratings yet
- Sleep Apnoea - Prof - DR K.K.PDocument44 pagesSleep Apnoea - Prof - DR K.K.PjialeongNo ratings yet
- Atelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Document10 pagesAtelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Gan BangNo ratings yet
- Basic Mechanical Ventilation 2014Document62 pagesBasic Mechanical Ventilation 2014dragon66No ratings yet
- The Ins and Outs of Ventilation 2. Mechanical VentilatorsDocument9 pagesThe Ins and Outs of Ventilation 2. Mechanical VentilatorsjhonvetNo ratings yet
- Optiflow Presentation-Carly TorgersenDocument12 pagesOptiflow Presentation-Carly Torgersenapi-252628311100% (1)
- Pulmonary Function Test, JARA CSUDocument73 pagesPulmonary Function Test, JARA CSUJohn NicoleNo ratings yet
- Vent Workshop NP Boot CampDocument47 pagesVent Workshop NP Boot CampChing WeiNo ratings yet
- Respiratory EmergenciesDocument34 pagesRespiratory EmergenciesRoshana MallawaarachchiNo ratings yet
- Basics of Waveform Interpretation: RET 2284 Principles of Mechanical VentilationDocument66 pagesBasics of Waveform Interpretation: RET 2284 Principles of Mechanical VentilationNanda MinndinNo ratings yet
- Suctioning Artificial Airways - AdultsDocument27 pagesSuctioning Artificial Airways - AdultssdaNo ratings yet
- Basics of Ventilatory SupportDocument43 pagesBasics of Ventilatory SupportAdhithya BhatNo ratings yet
- Rapid Sequence InductionDocument8 pagesRapid Sequence InductionAngela Mitchelle NyanganNo ratings yet
- Persistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarDocument31 pagesPersistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarAbhay BarnwalNo ratings yet
- Bivent PittsDocument63 pagesBivent PittsFarook BaigNo ratings yet
- Mechanical Ventilation AulaDocument47 pagesMechanical Ventilation Aulaapi-3820606100% (1)
- Updated: Dec 07, 2016 Author: Justina Gamache, MD Chief Editor: Guy W Soo Hoo, MD, MPHDocument42 pagesUpdated: Dec 07, 2016 Author: Justina Gamache, MD Chief Editor: Guy W Soo Hoo, MD, MPHgita suci arianiNo ratings yet
- Respiratory Case StudiesDocument6 pagesRespiratory Case Studiesadom09No ratings yet
- Pulmonary Function TestsDocument20 pagesPulmonary Function TestsMohamedSalah100% (2)
- Registry Examination For Advanced Respiratory Therapists (RRT)Document6 pagesRegistry Examination For Advanced Respiratory Therapists (RRT)Sandy HartmanNo ratings yet
- ArdsDocument81 pagesArdsAmit KlNo ratings yet
- Lung Sounds: An Assessment of The Patient in Respiratory DistressDocument40 pagesLung Sounds: An Assessment of The Patient in Respiratory DistressJoseph Rodney de LeonNo ratings yet
- 161111163114Document31 pages161111163114lejizixNo ratings yet
- AnticoagulantsDocument19 pagesAnticoagulantsOsama ZbedaNo ratings yet
- RT 220 B C AirwaystudyguideDocument25 pagesRT 220 B C Airwaystudyguiderpebdani0% (2)
- Basics of Mechanical Ventilation For Residents: DR Ghaleb Almekhlafi MD, SFCCM PSMMCDocument43 pagesBasics of Mechanical Ventilation For Residents: DR Ghaleb Almekhlafi MD, SFCCM PSMMCGHALEB A. Almekhlafi100% (1)
- Auto PEEPDocument16 pagesAuto PEEPVishwajith Murthy100% (1)
- Chronic BronchitisDocument2 pagesChronic BronchitisEimhie Lee CasiNo ratings yet
- Managing Mechanical VentilationDocument7 pagesManaging Mechanical VentilationArden QuiambaoNo ratings yet
- Acute Resp FailureDocument52 pagesAcute Resp FailureAlex ChiuNo ratings yet
- Mechanical VentDocument24 pagesMechanical VentRochim CoolNo ratings yet
- Respiratory System MedicationsDocument2 pagesRespiratory System Medicationsmlbrown8No ratings yet
- APRVDocument20 pagesAPRVivanrom100% (1)
- Cardiovascular Pathology 1:: Blood VesselsDocument48 pagesCardiovascular Pathology 1:: Blood VesselsRaiver CadenNo ratings yet
- Basic Principles of Mechanical VentilationDocument34 pagesBasic Principles of Mechanical VentilationMohamed KorieshNo ratings yet
- Pilbeam - Mechanical Ventilation Physiological and Clinical Applications-59-73.en - EsDocument15 pagesPilbeam - Mechanical Ventilation Physiological and Clinical Applications-59-73.en - EsAdriana MartinezNo ratings yet
- 406 - Respiratory Therapy Consult Service HandbookDocument28 pages406 - Respiratory Therapy Consult Service HandbookIkhsan JohnsonNo ratings yet
- SMART Learning Goals.Document3 pagesSMART Learning Goals.Anusha VergheseNo ratings yet
- Medical TerminologyDocument2 pagesMedical TerminologyAnusha VergheseNo ratings yet
- Roy's Adaptation ModelDocument2 pagesRoy's Adaptation ModelAnusha VergheseNo ratings yet
- INDIVIDUAL CASE ANALYSIS ScribdDocument2 pagesINDIVIDUAL CASE ANALYSIS ScribdAnusha VergheseNo ratings yet
- TerminologyDocument2 pagesTerminologyAnusha VergheseNo ratings yet
- Endotracheal IntubationDocument1 pageEndotracheal IntubationAnusha VergheseNo ratings yet
- Allergic Reactions: What To Look ForDocument2 pagesAllergic Reactions: What To Look ForAnusha VergheseNo ratings yet
- Procedure Trays ListDocument1 pageProcedure Trays ListAnusha VergheseNo ratings yet
- ColicDocument1 pageColicAnusha VergheseNo ratings yet
- Bites and StingsDocument1 pageBites and StingsAnusha VergheseNo ratings yet
- Care Guidelines For Minor Open WoundsDocument1 pageCare Guidelines For Minor Open WoundsAnusha VergheseNo ratings yet
- Chemical Burns First AidDocument1 pageChemical Burns First AidAnusha VergheseNo ratings yet
- Prevent Water Related InjuriesDocument1 pagePrevent Water Related InjuriesAnusha VergheseNo ratings yet
- Gastric LavageDocument2 pagesGastric LavageAnusha VergheseNo ratings yet
- Chest Xray InterpretationDocument3 pagesChest Xray InterpretationAnusha VergheseNo ratings yet
- TB DiseaseDocument3 pagesTB DiseaseAnusha VergheseNo ratings yet
- Inducing Hypothermia in Post Cardiac Arrest PatientsDocument2 pagesInducing Hypothermia in Post Cardiac Arrest PatientsAnusha VergheseNo ratings yet
- S.N o Criteria Yes No Remarks: Checklist For Intra-Hospital Transport of PatientDocument2 pagesS.N o Criteria Yes No Remarks: Checklist For Intra-Hospital Transport of PatientAnusha VergheseNo ratings yet
- Protocol On Transcutaneous PacingDocument7 pagesProtocol On Transcutaneous PacingAnusha VergheseNo ratings yet
- IV Lines and Safety Measures in Its Use For PatientsDocument2 pagesIV Lines and Safety Measures in Its Use For PatientsAnusha VergheseNo ratings yet
- CholeraDocument9 pagesCholeraAnusha VergheseNo ratings yet
- S.N o Criteria Yes No Remarks: Checklist For Intra-Hospital Transport of PatientDocument2 pagesS.N o Criteria Yes No Remarks: Checklist For Intra-Hospital Transport of PatientAnusha VergheseNo ratings yet
- Leukemias Nursing ManagementDocument20 pagesLeukemias Nursing ManagementAnusha Verghese100% (5)
- Infection and Its Mode of TransmissionDocument33 pagesInfection and Its Mode of TransmissionAnusha Verghese100% (1)
- What Is Hodgkin's Disease?: Lymphoma CancerDocument4 pagesWhat Is Hodgkin's Disease?: Lymphoma CancerAnusha VergheseNo ratings yet
- Blood TransfusionDocument20 pagesBlood TransfusionAnusha VergheseNo ratings yet
- Leukemia 5Document26 pagesLeukemia 5Anusha VergheseNo ratings yet
- Lymphomas 5Document32 pagesLymphomas 5Anusha VergheseNo ratings yet
- Multiple MyelomaDocument10 pagesMultiple MyelomaFadina RizkiNo ratings yet
- LeukemiasDocument8 pagesLeukemiasAr-jay JubaneNo ratings yet
- Drug Profile 2015Document75 pagesDrug Profile 2015api-324380555100% (1)
- Swa 4 Eng 219Document2 pagesSwa 4 Eng 219api-425903925No ratings yet
- Asuhan PrenatalDocument25 pagesAsuhan PrenatalRifqiyah Al-ManshurNo ratings yet
- Front Matter 2021Document18 pagesFront Matter 2021Евгений ПанковецNo ratings yet
- My ResearchDocument6 pagesMy Researchmaya vermaNo ratings yet
- In Vitro Anti-Cancer Activity of Piper Betel Leaf Extract On HA - 29 and Its Anti-Oxidant ActivityDocument4 pagesIn Vitro Anti-Cancer Activity of Piper Betel Leaf Extract On HA - 29 and Its Anti-Oxidant ActivityEditor IJTSRDNo ratings yet
- Nodular Goiter Concept MapDocument5 pagesNodular Goiter Concept MapAllene PaderangaNo ratings yet
- Lecture 15 PDFDocument20 pagesLecture 15 PDFSrramNo ratings yet
- Arixtra: (Fondaparinux Sodium) InjectionDocument26 pagesArixtra: (Fondaparinux Sodium) InjectionTri Purma SariNo ratings yet
- NewDocument122 pagesNewKalimpasha PathanNo ratings yet
- Chapter 7 of 10 - The FDA vs. Dr. BurzynskiDocument10 pagesChapter 7 of 10 - The FDA vs. Dr. BurzynskispiritualbeingNo ratings yet
- OSCE of Ear Nose & ThroatDocument23 pagesOSCE of Ear Nose & Throatmasood alam100% (1)
- Scientific ProgramDocument27 pagesScientific ProgramYash SharmaNo ratings yet
- 7 08 Ristic RDocument13 pages7 08 Ristic RsucrooNo ratings yet
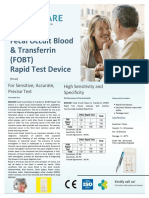
- Brosur Produk BIOCARE Fecal Occult Blood & Transferrin (FOBT) Rapid Test DeviceDocument1 pageBrosur Produk BIOCARE Fecal Occult Blood & Transferrin (FOBT) Rapid Test DeviceMarek SamektoNo ratings yet
- Opt Halm OlogyDocument87 pagesOpt Halm OlogyAya MahmoudNo ratings yet
- Penile CancerDocument25 pagesPenile CancerFlorencia Adys Bennington100% (1)
- Pharmacotherapy Handbook, 7th Edition 2009 (0376-0383)Document8 pagesPharmacotherapy Handbook, 7th Edition 2009 (0376-0383)rahmawatimrNo ratings yet
- Nalco 2000 MSDSDocument10 pagesNalco 2000 MSDSImanuel MarpaungNo ratings yet
- Interrobang Issue For January 23rd, 2012Document24 pagesInterrobang Issue For January 23rd, 2012interrobangfsuNo ratings yet
- Surgery 2 Case ReportDocument12 pagesSurgery 2 Case ReportElvis NgNo ratings yet
- Stages of GingivitisDocument42 pagesStages of Gingivitislia wardinaNo ratings yet
- Mapei Mapetop N Ar 6Document9 pagesMapei Mapetop N Ar 6Milos Sholim RadovanovicNo ratings yet
- Urine AnalysisDocument31 pagesUrine AnalysisajaysomNo ratings yet
- Final UnodDocument33 pagesFinal UnodApryle FedelesNo ratings yet
- Management of Metastatic Spinal Cord Compression: Southern Medical Journal September 2017Document9 pagesManagement of Metastatic Spinal Cord Compression: Southern Medical Journal September 2017Rudy Arindra WijayaNo ratings yet
- Sterile Parenteral Products: A Narrative Approach: Journal of Drug Delivery and TherapeuticsDocument8 pagesSterile Parenteral Products: A Narrative Approach: Journal of Drug Delivery and TherapeuticsArinta Purwi SuhartiNo ratings yet
- Smokers' MelanosisDocument9 pagesSmokers' Melanosisnwhator32No ratings yet
- Breast MassesDocument12 pagesBreast MassesTrivedi NisargNo ratings yet
- An Approach To Thyroid EnlargementDocument3 pagesAn Approach To Thyroid EnlargementHardik JeenaNo ratings yet