Professional Documents
Culture Documents
Systemic Lupus Erythematosus
Uploaded by
Benjamin Agbonze0 ratings0% found this document useful (0 votes)
63 views1 pagelupus
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentlupus
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
63 views1 pageSystemic Lupus Erythematosus
Uploaded by
Benjamin Agbonzelupus
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 1
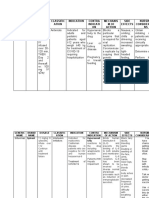
CATEGORY: IMMUNE DYSFUNCTION
SYSTEMIC LUPUS ERYTHEMATOSUS
Systemic Lupus
Erythematosus (SLE)
Angela Midgley, University of Liverpool, UK
Juvenile onset SLE
Juvenile-onset SLE (JSLE) is the childhood form of SLE. It is a relatively rare condition with an
unclear prevalance in the UK. Onset occurs prior to the age of 18, typically between 1216 years
and accounts for up to 20% of all cases of SLE.
The complexity of this disease is reflected in the diverse clinical and immunological symptoms
upon which diagnosis is based. The diagnosis is based upon the revised American College of
Rheumatology classification criteria for adult onset SLE which has been adopted to be used in a
juvenile population. It consists of 11 criteria (which include malar rash, oral or nasal ulceration,
nephritis and a positive test for nuclear antibodies) of which four have to be met, simultaneously
or periodically before a diagnosis can be fulfilled.
A complex interplay between genetic and environmental factors appears to contribute towards its
immunopathogenesis, resulting in activation of all components of both the innate and acquired
immune system.
Immune system dysfunction
The disease is characterised by the production of self (auto) antibodies (directed against nuclear
self (auto) antigens), inflammation and organ damage. The presence of antinuclear antibodies
has been detected in the serum of a majority of patients before the onset of clinical disease
symptoms, and levels of certain auto-antibodies have been found to correlate with disease activity
supporting a role for these antibodies in mediating disease pathology. It is thought that these
antibodies form antibody-nuclear antigen immune complexes, which deposit in tissues and trigger
local inflammation, thereby contributing to tissue injury.
Increased apoptosis (programmed cell death) and defective clearance of apoptotic material are
characteristic of the mouse-model of lupus and human SLE. Autoantigens typical of lupus cluster
in surface blebs of apoptotic cells, increasing their immune-exposure. Saturation of physiological
processes to safely remove apoptotic debris amplifies autoantigen exposure.
B lymphocytes are the cells of the immune system that make antibodies; inappropriate activation
and proliferation of autoreactive memory B cells in the periphery are also characteristic of SLE
T lymphocytes are also thought to contribute to disease progression and pathology.
T cells that reactive with several nuclear autoantigens have been isolated from the peripheral
blood of SLE patients. T cells from SLE patients also display abnormal signalling and secrete
cytokines that promote inflammation. Regulatory T cells (cells important in maintaining cell
tolerance) have been shown to be low in SLE and their suppressive function impaired.
The copyright for this work resides with the author
Systemic lupus erythematosus (SLE) is a severe, relapsing, remitting multisystem autoimmune
disease. The name systemic lupus implies that almost any organ or system within the body might
be affected and lupus is perhaps the classical multi-symptom illness. Onset can occur at any age
however it most typically presents in young adult females at a female to male ratio of 9:1.
You might also like
- Consumer Behaviour Towards AppleDocument47 pagesConsumer Behaviour Towards AppleAdnan Yusufzai69% (62)
- CH 13 Pediatric Practice Problems AnswersDocument6 pagesCH 13 Pediatric Practice Problems AnswersJm EstigoyNo ratings yet
- Child and Adolescent Growth and DevelopmentDocument4 pagesChild and Adolescent Growth and DevelopmentNicole DealaNo ratings yet
- Poems by Betty Fox Frazer - Psychiatric NurseDocument4 pagesPoems by Betty Fox Frazer - Psychiatric NurseBetty FoxNo ratings yet
- Medication AdministrationDocument12 pagesMedication AdministrationDinah RealNo ratings yet
- Medication ErrorDocument37 pagesMedication ErrorJitendra PanthiNo ratings yet
- Understanding Culture, Society and PoliticsDocument62 pagesUnderstanding Culture, Society and PoliticsTeds TV89% (84)
- Systemic Lupus ErythematosusDocument22 pagesSystemic Lupus ErythematosusYaska MusaNo ratings yet
- Systemic Lupus ErythematosusDocument16 pagesSystemic Lupus ErythematosusSaharNo ratings yet
- Antifungal AgentsDocument37 pagesAntifungal AgentsChandrashekhar UnakalNo ratings yet
- Philosophy of Health EssayDocument2 pagesPhilosophy of Health Essayapi-479101429No ratings yet
- Mclemore Synthesis EssayDocument4 pagesMclemore Synthesis Essayapi-283558804No ratings yet
- Pathophysiology of Systemic Lupus ErythematosusDocument14 pagesPathophysiology of Systemic Lupus ErythematosusChairunisa AnggrainiNo ratings yet
- Medication ErrorDocument19 pagesMedication ErrorEvitaIrmayantiNo ratings yet
- Medication ErrorsDocument11 pagesMedication ErrorsJayson V Caranto RN100% (1)
- Parathyroid Gland and Other Endocrine Glands OverviewDocument35 pagesParathyroid Gland and Other Endocrine Glands OverviewDrRahma Ali HeissNo ratings yet
- Blood Transfusion ESSAY 1 1Document3 pagesBlood Transfusion ESSAY 1 1Ednilson Domingos0% (1)
- Pharmacology IntroductionDocument138 pagesPharmacology Introductioncoosa liquorsNo ratings yet
- Pediatric Dosage CalculationsDocument1 pagePediatric Dosage Calculationssmckenzie1964No ratings yet
- Metformin: Dosing & UsesDocument8 pagesMetformin: Dosing & UsesMaria Alejandra Siachoque JaraNo ratings yet
- Anti-Fungal Drugs SushDocument31 pagesAnti-Fungal Drugs SushCheng XinvennNo ratings yet
- Systemic Lupus ErythematosusDocument51 pagesSystemic Lupus ErythematosusEmma AndayaNo ratings yet
- Medication Administration 1Document2 pagesMedication Administration 1CR ChicNo ratings yet
- HepatoblastomaDocument38 pagesHepatoblastomaSaroj PandaNo ratings yet
- 6.antifungal AgentsDocument51 pages6.antifungal Agentsmulatumelese0% (1)
- Systemic Lupus ErythematosusDocument14 pagesSystemic Lupus ErythematosusArun ArachelvanNo ratings yet
- Topical AntifungalsDocument14 pagesTopical AntifungalsRasha Mohammad100% (1)
- Anticancer Drugs: Pharmacology 2Document74 pagesAnticancer Drugs: Pharmacology 2Hannah Laput100% (1)
- MumpsDocument7 pagesMumpsKristine DolatreNo ratings yet
- BeneficenceDocument3 pagesBeneficenceAngelique Jade EnriquezNo ratings yet
- Cleft Lip and PalateDocument39 pagesCleft Lip and PalateBiswaroop ChandraNo ratings yet
- DOH ProgramsDocument6 pagesDOH ProgramsrobotkabaNo ratings yet
- Alteration in Inflammatory and Immunologic Response 2012Document22 pagesAlteration in Inflammatory and Immunologic Response 2012Pamela BagabaldoNo ratings yet
- Nursing AssessmentDocument3 pagesNursing AssessmentJanine PelayoNo ratings yet
- Pediatric Drug Calculations 03Document38 pagesPediatric Drug Calculations 03Leia Avriele TankiamcoNo ratings yet
- Systemc Lupus EritematousDocument41 pagesSystemc Lupus EritematousCanis MajorisNo ratings yet
- Wound DebridementDocument3 pagesWound DebridementRoseben SomidoNo ratings yet
- CVA Case AnalysisDocument11 pagesCVA Case AnalysisFrancis PeterosNo ratings yet
- Riehl's Self-Concept Module of NursingDocument1 pageRiehl's Self-Concept Module of NursingRachelle Geronimo100% (1)
- Antifungal Drugs: University of Nairobi Department of Public Health, Pharmacology & ToxicologyDocument32 pagesAntifungal Drugs: University of Nairobi Department of Public Health, Pharmacology & ToxicologyAnonymous RA6sVagiNo ratings yet
- The Heart of A NurseDocument2 pagesThe Heart of A Nurseflex gyNo ratings yet
- Pharmacodynamic InteractionsDocument12 pagesPharmacodynamic InteractionsIshita SharmaNo ratings yet
- ASHP Guidelines On Preventing Medication Errors in HospitalsDocument9 pagesASHP Guidelines On Preventing Medication Errors in HospitalsMedarabiaNo ratings yet
- Case Presentation On Central Nervous System InfectionDocument7 pagesCase Presentation On Central Nervous System Infectionnarseya100% (1)
- Final ThesisDocument22 pagesFinal Thesiserika100% (3)
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- Paper C - Nurs 324-3-3Document10 pagesPaper C - Nurs 324-3-3api-242367576No ratings yet
- Sample Teaching PlanDocument3 pagesSample Teaching Planmine2515No ratings yet
- Geriatrics, Gerontology, GeronticDocument5 pagesGeriatrics, Gerontology, GeronticTsaabitah AnwarNo ratings yet
- Drug StudyDocument4 pagesDrug StudyFrances Oscar GaviolaNo ratings yet
- Chapter 007Document34 pagesChapter 007calfornianursingacadNo ratings yet
- Polycythemia Guide: Causes, Symptoms & TreatmentDocument16 pagesPolycythemia Guide: Causes, Symptoms & TreatmentVanessa Camille DomingoNo ratings yet
- CarbohydrateDocument116 pagesCarbohydrateManoj SigdelNo ratings yet
- Systemic Lupus ErythematosusDocument37 pagesSystemic Lupus ErythematosusFirman Ichlasul AmalNo ratings yet
- Pediatric Atopic DermatitisDocument101 pagesPediatric Atopic DermatitisTara Sefanya Kairupan100% (1)
- Human Growth And Development: A Comprehensive Look At Stage Theory And Learning ProcessesDocument11 pagesHuman Growth And Development: A Comprehensive Look At Stage Theory And Learning ProcessesChris MerriqueNo ratings yet
- Nasopharyngeal Cancer OverviewDocument31 pagesNasopharyngeal Cancer OverviewMae UsquisaNo ratings yet
- Burns MGNT and CalculationDocument7 pagesBurns MGNT and CalculationPoova RagavanNo ratings yet
- Insights from entrepreneursDocument2 pagesInsights from entrepreneursyeahboyman100% (1)
- Antimicrobial DrugsDocument20 pagesAntimicrobial Drugsnadar shahNo ratings yet
- C (SLE) Is A Multiorgan System Autoimmune Disease With Numerous ImmunologicalDocument4 pagesC (SLE) Is A Multiorgan System Autoimmune Disease With Numerous Immunologicalbebe qNo ratings yet
- Q Banks Points PDFDocument246 pagesQ Banks Points PDFmarwaNo ratings yet
- MicrobiologyDocument1,299 pagesMicrobiologyBenjamin Agbonze100% (1)
- TB Neg Symptom Form PDFDocument1 pageTB Neg Symptom Form PDFBenjamin AgbonzeNo ratings yet
- Things To Know On Your OB PDFDocument2 pagesThings To Know On Your OB PDFKatherynNo ratings yet
- Week 12 Study GuideDocument2 pagesWeek 12 Study GuideBenjamin AgbonzeNo ratings yet
- Usmle Hy Images: By: MeduploaderDocument62 pagesUsmle Hy Images: By: Meduploaderdamodarpatil100% (18)
- Usmle Hy Images: By: MeduploaderDocument62 pagesUsmle Hy Images: By: Meduploaderdamodarpatil100% (18)
- Thyroid Gland in the NeckDocument767 pagesThyroid Gland in the NeckMack LinfidioNo ratings yet
- NBME 7 BLOCK 1-4 (With Answers)Document206 pagesNBME 7 BLOCK 1-4 (With Answers)Benjamin Agbonze100% (1)
- NHPCO ChiPPS Pediatric Palliative Care NewsletterDocument32 pagesNHPCO ChiPPS Pediatric Palliative Care NewsletterBenjamin AgbonzeNo ratings yet
- The Article I SelectedDocument2 pagesThe Article I SelectedBenjamin AgbonzeNo ratings yet
- Health Care Access For Latino Mixed-StatDocument20 pagesHealth Care Access For Latino Mixed-StatBenjamin AgbonzeNo ratings yet
- Md3 Quiz: E. T CellsDocument17 pagesMd3 Quiz: E. T CellsBenjamin AgbonzeNo ratings yet
- Systemic Lupus Erythematosus (SLE)Document42 pagesSystemic Lupus Erythematosus (SLE)louradelNo ratings yet
- NHPCO ChiPPS Pediatric Palliative Care NewsletterDocument32 pagesNHPCO ChiPPS Pediatric Palliative Care NewsletterBenjamin AgbonzeNo ratings yet
- Embryologic DefectsDocument62 pagesEmbryologic DefectsBenjamin AgbonzeNo ratings yet
- Hip Fracture in Elderly Patients: Outcomes For Function, Quality of Life and Type of ResidenceDocument18 pagesHip Fracture in Elderly Patients: Outcomes For Function, Quality of Life and Type of ResidenceBenjamin AgbonzeNo ratings yet
- Masonry Brickwork 230 MMDocument1 pageMasonry Brickwork 230 MMrohanNo ratings yet
- COT EnglishDocument4 pagesCOT EnglishTypie ZapNo ratings yet
- Sheqxel Bbs Participation Dashboard TemplateDocument39 pagesSheqxel Bbs Participation Dashboard TemplateMuhammad Adytio DarmawanNo ratings yet
- Kastanakis 2014Document8 pagesKastanakis 2014Andreea Georgiana MocanuNo ratings yet
- LGFL Service GuideDocument24 pagesLGFL Service GuideThe Return of the NoiristaNo ratings yet
- Phys114 Ps 1Document11 pagesPhys114 Ps 1Reine Amabel JarudaNo ratings yet
- Write 10 Lines On My Favourite Subject EnglishDocument1 pageWrite 10 Lines On My Favourite Subject EnglishIrene ThebestNo ratings yet
- Maximizing modular learning opportunities through innovation and collaborationDocument2 pagesMaximizing modular learning opportunities through innovation and collaborationNIMFA SEPARANo ratings yet
- Universal Robina Co. & Bdo Unibank Inc.: Research PaperDocument25 pagesUniversal Robina Co. & Bdo Unibank Inc.: Research PaperSariephine Grace ArasNo ratings yet
- Manju Philip CVDocument2 pagesManju Philip CVManju PhilipNo ratings yet
- 9AKK101130D1664 OISxx Evolution PresentationDocument16 pages9AKK101130D1664 OISxx Evolution PresentationfxvNo ratings yet
- Aquafine Optivenn Series Data SheetDocument8 pagesAquafine Optivenn Series Data SheetKenz ZhouNo ratings yet
- Choose the Best WordDocument7 pagesChoose the Best WordJohnny JohnnieeNo ratings yet
- Main Hoon Na - WikipediaDocument8 pagesMain Hoon Na - WikipediaHusain ChandNo ratings yet
- Compare and Contrast High School and College EssayDocument6 pagesCompare and Contrast High School and College Essayafibkyielxfbab100% (1)
- Done by Akansha Bharti Harshitha K.N. Ishika Sunil Rajput Rashmi NaikDocument12 pagesDone by Akansha Bharti Harshitha K.N. Ishika Sunil Rajput Rashmi NaikRamya BalanNo ratings yet
- 153C Final Exam Study Guide-2Document6 pages153C Final Exam Study Guide-2Soji AdimulaNo ratings yet
- Color Codes and Irregular Marking-SampleDocument23 pagesColor Codes and Irregular Marking-Samplemahrez laabidiNo ratings yet
- Merchandise Floor Ready Standards - Supplier InformationDocument46 pagesMerchandise Floor Ready Standards - Supplier InformationGarmentLearner100% (1)
- The Life and Works of Jose RizalDocument20 pagesThe Life and Works of Jose RizalBemtot Blanquig100% (1)
- Grade 10Document39 pagesGrade 10amareNo ratings yet
- Scholars of Hadith Methodology in Dealing With The Two Sahihs: The Criticized Ahadith As A Model. Ammar Ahmad Al-HaririDocument37 pagesScholars of Hadith Methodology in Dealing With The Two Sahihs: The Criticized Ahadith As A Model. Ammar Ahmad Al-HaririSalah KhanNo ratings yet
- Indian Institute OF Management, BangaloreDocument20 pagesIndian Institute OF Management, BangaloreGagandeep SinghNo ratings yet
- SOP for Troubleshooting LT ACB IssuesDocument9 pagesSOP for Troubleshooting LT ACB IssuesAkhilesh Kumar SinghNo ratings yet
- Strain Gauge Sensor PDFDocument12 pagesStrain Gauge Sensor PDFMario Eduardo Santos MartinsNo ratings yet
- CH - 3Document3 pagesCH - 3Phantom GamingNo ratings yet
- The Invisible Hero Final TNDocument8 pagesThe Invisible Hero Final TNKatherine ShenNo ratings yet
- Lab ReportDocument5 pagesLab ReportHugsNo ratings yet