Professional Documents
Culture Documents
Preguntas y Respuestas 5
Uploaded by
Juan de Dios Díaz-Rosales0 ratings0% found this document useful (0 votes)
14 views35 pagesPreguntas y Respuestas
Preparación para el examen USMLE y ENARM
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPreguntas y Respuestas
Preparación para el examen USMLE y ENARM
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views35 pagesPreguntas y Respuestas 5
Uploaded by
Juan de Dios Díaz-RosalesPreguntas y Respuestas
Preparación para el examen USMLE y ENARM
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 35
Preguntas y
Respuestas 5
Ciruga General
Clinical Scenario 1. A 30-year-old man sustains blunt
head trauma and is unconscious. His urine output
exceeds 1,500 mL per hour despite only receiving
maintenance intravenous fluids. He becomes profoundly
hypernatremic. Which of the following is the next step in
the initial management of this patient?
Answer. This patient has blunt head trauma and
diabetes insipidus, characterized by high volume, low
osmolality urine. This, untreated, may result in profound
dehydration and hypernatremia. Treatment is
conservative, with replacement of free water
intravenously
Clinical Scenario 5. A 20-year-old woman presents
after a skiing accident. She is alert and talking but not
moving. Her blood pressure is 80/55 mm Hg, and her
pulse is 80 beats/minute. What is the etiology of her
shock, and what should the workup include to aid in the
diagnosis?
Answer. Neurogenic shock from a probable cervical
spine fracture. Workup should include a complete spine
evaluation.
Clinical Scenario 23. A 39-year-old woman complains
of right upper quadrant pain. She also has nausea and
fatigue. She has a history of ulcerative colitis. Physical
examination reveals icteric sclera. Laboratory studies
reveal elevated transaminases. What is the next step in
the management of this patient?
Answer. This patient likely has primary sclerosing
cholangitis. This condition results in stenosis or
obstruction of the ductal system. ERCP may reveal
thickening and stenosis of the biliary ductal system.
Clinical Scenario 59. A 45-year-old man who smokes
presents with progressively increasing cough, sputum
production, and fever for the past 4 days. In the past
day he has also noticed the development of right upper
quadrant abdominal pain. On examination, he has
diminished breath sounds at the right base, with
dullness to percussion. Abdominal examination shows
minimal tenderness in the right upper quadrant, with no
Murphy sign. What is the diagnosis?
Answer. He most likely has a right lower lobe
pneumonia irritating his diaphragm, which is leading to
his right upper quadrant pain.
Clinical Scenario 63. A 23-year-old man is seen in the
emergency department after a motor vehicle accident.
He was an unrestrained passenger. He is able to breathe
on his own but tells you that each breath is extremely
painful. You note that a segment of his chest wall
appears to sink inwards with each respiration, and that
when he exhales this same segment does not move with
the rest of the chest wall. Vital signs are stable. The
patient has no other obvious traumatic injuries. The
arterial blood gas reads as follows: 7.3/55/85/25. What is
the most appropriate next step in management?
Answer. This describing flail chest. This occurs when four
or more ribs are fractured in at least two locations, leading
to paradoxical movement of the chest wall during
respiration. This commonly occurs after trauma such as a
motor vehicle accident. The true danger in patients with
flail chest is the frequent underlying pulmonary contusion.
In this patient we see a blood gas indicative of a decreased
respiratory effort, suggesting that he is not properly
respiring. We would need to inubate this patient and
provide mechanical ventilation in light of the marked
respiratory distress.
Clinical Scenario 20. A 73-year-old woman undergoes a computed
tomography (CT) scan for abdominal pain and is found to have
thickening of the terminal ileum. She is also noted to have multiple
mesenteric lymph nodes that are enlarged to more than 2 cm. A
colonoscopy is performed that shows no abnormalities of the colon,
but when the terminal ileum is entered, a friable intraluminal mass
is encountered. The biopsies of this mass are read as diffuse large
cell non-Hodgkin lymphoma. Positron emission tomography and CT
confirm involvement of the terminal ileum but are also read as
showing multiple mediastinal nodes involved with the disease. Bone
marrow aspiration is negative for lymphoma.
Should this patient undergo a wide resection of the diseased
terminal ileum prior to starting chemotherapy?
Answer. No. The patient has stage III non-Hodgkin
lymphoma and should be treated with chemotherapy
and possibly radiotherapy to the mediastinum. The only
indication for surgical exploration in this patient would
be if she should start bleeding from the terminal ileum
or if the involved area should perforate.
Clinical Scenario 16. A 25-year-old man presents to the
emergency department with a history of 6 months of variable
right lower quadrant abdominal pain, which acutely worsened
over the past 12 hours so that he now rates it as 8 on a scale of
10, with 10 being the most painful. He also reports that he has
been having diarrhea and low back pain for about 3 months.
Computed tomography scan shows stranding of the mesentery
in the right lower quadrant. On insertion of a laparoscope, you
note that the terminal ileum and cecum are markedly inflamed,
with some fat wrapping of the terminal ileum, although the
appendix appears normal.
What is your next step in this operation?
Answer. Close the camera incision and treat the patient
for Crohn disease. Even if the base of the cecum is
uninvolved, appendectomy is contraindicated in the
presence of Crohn disease due to an unacceptably high
rate of enterocutaneous fistulization.
A 30-year-old man consults a physician because he has been having increasing
difficulty swallowing both solids and liquids. Physical examination of the patient is
noncontributory. Barium swallow studies show a mostly dilated esophagus with
slow passage of barium into the stomach. The very distal part of the esophagus
appears narrowed into a "bird's beak." Esophageal manometry shows incomplete
relaxation of the lower esophageal sphincter in response to swallowing, high
resting lower esophageal pressure, and absent esophageal peristalsis.
Question 1 of 5. The manometry and barium swallow studies most strongly
support which of the following diagnoses?
/ A. Achalasia
/ B. Adenocarcinoma
/ C. Barrett esophagus
/ D. Squamous cell carcinoma
/ E. Systemic sclerosis
The correct answer is A. The most likely diagnosis is
achalasia. This condition is a neurogenic esophageal
disorder that can occur at any age, but frequently is
diagnosed when individuals are between the ages of 20
and 40. Characteristically, the swallowing difficulties
involve both solid food and liquids. The manometry
findings illustrated are typical; the barium swallow
findings may be as illustrated or may instead show
diffuse esophageal dilation without the "bird's beak"
near the lower esophageal sphincter.
Question 2 of 5. This patient's condition is most likely
due to which of the following?
/ A. Acid reflux
/ B. Cancerous destruction
/ C. Candida infection
/ D. Fibrosis of the esophageal wall
/ E. Lack of ganglion cells
The correct answer is E. Individuals who have
achalasia have been found to have a deficiency of
inhibitory ganglion cells within the esophageal wall.
This lack causes an imbalance in excitatory and
inhibitory neurotransmission, with the result that the
lower esophageal sphincter tends to have a higher-thannormal muscle tone and relaxes only with difficulty.
Question 3 of 5. Which of the following regulators
would most likely inhibit the lower esophageal sphincter
in normal individuals?
/ A. Acetylcholine and substance P
/ B. Substance P and nitric oxide
/ C. Substance P only
/ D. Vasoactive intestinal polypeptide and acetylcholine
/ E. Vasoactive intestinal polypeptide and nitric oxide
The correct answer is E. Physiologically important
inhibitors of the lower esophageal sphincter include
nitric oxide and vasoactive intestinal polypeptide.
Physiologically important substances that stimulate the
lower esophageal sphincter include acetylcholine and
substance P.
Question 4 of 5. Which of the following medications is
used to directly relax the lower esophageal sphincter?
/ A. Diphenoxylate
/ B. Famotidine
/ C. Granisetron
/ D. Isosorbide dinitrate
/ E. Metoclopramide
The correct answer is D. Commonly used
medications to relax the lower esophageal sphincter in
patients with achalasia include nitrates such as
isosorbide dinitrate (remember that nitric oxide
physiologically inhibits the lower esophageal sphincter)
and calcium channel blockers such as nifedipine (which
inhibit calcium flow into the smooth muscle of the lower
esophageal sphincter, thereby inhibiting contraction.)
For patients in whom medical therapy fails, other
options include paralysis of the lower esophageal
sphincter with intrasphincteric injection of botulinum
toxin, pneumatic dilatation, and a Heller myotomy
(which interrupts the muscles of the lower esophageal
Question 5 of 5. Worldwide, which of the following
parasitic diseases is most likely to produce a disorder
that clinically resembles this patient's condition?
/ A. Ascariasis
/ B. African sleeping sickness
/ C. Chagas disease
/ D. Cysticercosis
/ E. Malaria
The correct answer is C. Chagas disease, which is
found in South and Central America and is due to
infection with Trypanosoma cruzi, can involve the heart,
colon, and esophagus. The esophageal involvement
clinically closely resembles achalasia.
A 35-year-old woman consults a physician because she has been having
trouble swallowing. She also often experiences chronic heartburn. The
physician performs a screening physical examination, and notices that the
skin of her hands appears tight and shiny. On specific questioning, she
reports having often experienced color changes in her hands from white to
blue to red.
Question 1 of 5. Which of the following is the most likely cause of the
patient's difficulties with swallowing?
A. Achalasia
B. Adenocarcinoma
C. Chagas disease
D. Scleroderma
E. Squamous carcinoma
The correct answer is D. The tip-off is the reference
to the patient's skin changes that are typical for
scleroderma, also known as systemic sclerosis.
Scleroderma is a disease that may be either
predominately limited to the skin or involve many body
systems, including the musculoskeletal system,
gastrointestinal tract (with esophageal involvement
most often symptomatic), cardiorespiratory system, and
renal system. Esophageal dysfunction is a common
complication of scleroderma. In most patients, the
skin changes are obvious, even if the patient has not
been previously diagnosed. Rarely, the skin changes
may be noticed at an earlier stage, in which the skin of
Question 2 of 5. The color changes described on the
patient's hand are most likely due to which of the
following?
/ A. Arteriolar spasm
/ B. BIood clots at sites of vascular injury
/ C. Large artery spasm
/ D. PIatelet clots
/ E. Stasis blood clots
The correct answer is A. The color changes described
are typical for Raynaud's phenomenon, which occurs
because of changes in perfusion due to arteriolar
spasm. Raynaud's phenomenon is common in
scleroderma, largely because the subintimal hyperplasia
of small vessels characteristic of scleroderma can
reduce the luminal diameter by more than 75%. Some
authors argue that the vascular changes seen in
scleroderma are actually the insult that triggers the
subsequent development of fibrosis.
Question 3 of 5. Additional findings on physical examination
include noting that the skin changes are limited to areas distal to
the elbow and knee, the presence of calcified nodules on the
extensor surfaces of the forearms, and the presence of
telangiectasias on the forearms. This suggests that this patient
has which of the following?
/ A. Bauer syndrome
/ B. Charcot syndrome
/ C. CREST syndrome
/ D. Crigler-Najjar syndrome
/ E. Dandy-Walker syndrome
The correct answer is C. These findings, together
with esophageal dysfunction and Raynaud's
phenomenon (both of which this patient has), are called
the CREST syndrome, also known as limited
cutaneous scleroderma. This form of scleroderma has a
better long-term prognosis than when the skin changes
also involve the trunk (diffuse scleroderma) and more
internal organs are additionally involved.
Question 4 of 5. If this woman's involved skin were
biopsied, which of the following would most likely be
seen?
/ A. CIeft separating the dermis and subcutaneous
tissues
/ B. Epithelial cell hyperplasia
/ C. Marked dermal fibrosis
/ D. Narrowing of the basal lamina of small capillaries
/ E. Thickening of rete pegs
The correct answer is C. In scleroderma, early
changes (at the point at which the hands appear
swollen, rather than with tight, thick skin) show edema
with perivascular infiltrates of CD4+ T cells. At this
stage, the collagen fibers are swollen and beginning to
degenerate. The smaller vessels may show basal lamina
thickening (not narrowing as in choice D) and
endothelial (not epithelial as in choice B) cell damage
and proliferation. With time, the characteristic marked
dermal fibrosis develops, which tends to both narrow
(not thicken as in choice E) the rete pegs and attach
the dermis tightly (compare with cleft formation as in
choice A) to subcutaneous tissues.
Question 5 of 5. More than 90% of the patients with
the limited cutaneous form of this disorder make which
of the following autoantibodies?
/ A. Anti-centromere
/ B. Anti-DNA topoisomerase l
/ C. Anti-double-stranded DNA
/ D. Anti-Golgi
/ E. Anti-ScI-70
The correct answer is A. All forms of scleroderma are
thought to have a strong autoimmune component, and
glucocorticoids and azathioprine are used to suppress
the inflammatory complications of scleroderma. (Other
drugs that can be used in therapy include penicillamine,
which inhibits collagen cross-linking, NSAIDS for pain,
and ACE inhibitors to protect the kidney if hypertension
or renal damage occurs.) The anti-centromere
antibody is quite specific for CREST syndrome (96% of
cases), and is only seen in a minority of patients with
diffuse scleroderma (mainly those with Raynaud's
phenomenon) and rarely in systemic lupus
erythematosus and mixed connective tissue disease.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Marketing Strategy of Singapore AirlinesDocument48 pagesMarketing Strategy of Singapore Airlinesi_sonet96% (49)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Recommendation Letter - One Young WorldDocument2 pagesRecommendation Letter - One Young WorldNabeel K. AdeniNo ratings yet
- Leukocytosis in Penetrating Trauma. Across Sectional Study. Arch Med 2015Document6 pagesLeukocytosis in Penetrating Trauma. Across Sectional Study. Arch Med 2015Juan de Dios Díaz-RosalesNo ratings yet
- Adult Intussussception Int J Student Res 2012Document3 pagesAdult Intussussception Int J Student Res 2012Juan De Dios Diaz-RosalesNo ratings yet
- Association of Obesity and Severity in Cholelithiasis. WJMMSR 2015Document3 pagesAssociation of Obesity and Severity in Cholelithiasis. WJMMSR 2015Juan de Dios Díaz-RosalesNo ratings yet
- Difference in Hematic Biometry Pre and PostsurgicalDocument4 pagesDifference in Hematic Biometry Pre and PostsurgicalJuan de Dios Díaz-RosalesNo ratings yet
- Oesophageal Perforation by Gunshot. Calicut Med J 2009Document4 pagesOesophageal Perforation by Gunshot. Calicut Med J 2009Juan de Dios Díaz-RosalesNo ratings yet
- Preguntas y Respuestas 7Document33 pagesPreguntas y Respuestas 7Juan de Dios Díaz-RosalesNo ratings yet
- Carcinoid Tumour in Second Part of Duodenum. Calicut Med J 2009Document3 pagesCarcinoid Tumour in Second Part of Duodenum. Calicut Med J 2009Juan de Dios Díaz-RosalesNo ratings yet
- Penetrating Pelvic Trauma. Panam J Trauma Crit Care 2013Document3 pagesPenetrating Pelvic Trauma. Panam J Trauma Crit Care 2013Juan de Dios Díaz-RosalesNo ratings yet
- Leukocytosis and Penetrating Trauma. Cir Cir 2012Document6 pagesLeukocytosis and Penetrating Trauma. Cir Cir 2012Juan de Dios Díaz-RosalesNo ratings yet
- Preguntas y Respuestas 6Document33 pagesPreguntas y Respuestas 6Juan de Dios Díaz-RosalesNo ratings yet
- Cirugía General. Preguntas y Respuestas 3Document21 pagesCirugía General. Preguntas y Respuestas 3Juan de Dios Díaz-Rosales100% (1)
- Cirugía General. Preguntas y Respuestas 4Document17 pagesCirugía General. Preguntas y Respuestas 4Juan de Dios Díaz-RosalesNo ratings yet
- Cirugía General: Preguntas y Respuestas 1Document31 pagesCirugía General: Preguntas y Respuestas 1Juan de Dios Díaz-RosalesNo ratings yet
- Cirugía General: Preguntas y Respuestas 2Document31 pagesCirugía General: Preguntas y Respuestas 2Juan de Dios Díaz-RosalesNo ratings yet
- Colangitis AgudaDocument22 pagesColangitis AgudaJuan de Dios Díaz-RosalesNo ratings yet
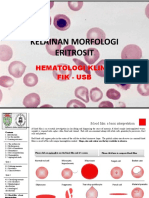
- Kelainan Morfologi EritrositDocument19 pagesKelainan Morfologi EritrositAdel shbelNo ratings yet
- Proceedings of The 2012 PNLG Forum: General AssemblyDocument64 pagesProceedings of The 2012 PNLG Forum: General AssemblyPEMSEA (Partnerships in Environmental Management for the Seas of East Asia)No ratings yet
- The Ten Commandments For Network MarketersDocument3 pagesThe Ten Commandments For Network MarketersJustin Lloyd Narciso PachecoNo ratings yet
- Certificate of Compliance ATF F 5330 20Document2 pagesCertificate of Compliance ATF F 5330 20Jojo Aboyme CorcillesNo ratings yet
- Bhagavad Gita: Chapter 18, Verse 47Document3 pagesBhagavad Gita: Chapter 18, Verse 47pankaj kararNo ratings yet
- Ass. No.1 in P.E.Document8 pagesAss. No.1 in P.E.Jessa GNo ratings yet
- Jamaica's Unemployment Aims, Causes and SolutionsDocument23 pagesJamaica's Unemployment Aims, Causes and Solutionsnetzii300067% (3)
- Mar 2021Document2 pagesMar 2021TanNo ratings yet
- Siege by Roxane Orgill Chapter SamplerDocument28 pagesSiege by Roxane Orgill Chapter SamplerCandlewick PressNo ratings yet
- Lecture 9-EVENT BUDGETDocument19 pagesLecture 9-EVENT BUDGETAlbina AbilkairNo ratings yet
- It - Unit 14 - Assignment 2 1Document8 pagesIt - Unit 14 - Assignment 2 1api-669143014No ratings yet
- Boston Consulting Group Portfolio Analysis MatrixDocument16 pagesBoston Consulting Group Portfolio Analysis MatrixNimish SharmaNo ratings yet
- The Rescue FindingsDocument8 pagesThe Rescue FindingsBini Tugma Bini Tugma100% (1)
- Understanding key abdominal anatomy termsDocument125 pagesUnderstanding key abdominal anatomy termscassandroskomplexNo ratings yet
- Music Literature (Western Music)Document80 pagesMusic Literature (Western Music)argus-eyed100% (6)
- Plusnet Cancellation FormDocument2 pagesPlusnet Cancellation FormJoJo GunnellNo ratings yet
- Buckling of Thin Metal Shells 58Document1 pageBuckling of Thin Metal Shells 58pawkomNo ratings yet
- Minotaur Transformation by LionWarrior (Script)Document7 pagesMinotaur Transformation by LionWarrior (Script)Arnt van HeldenNo ratings yet
- DDAL05-02 The Black RoadDocument45 pagesDDAL05-02 The Black Roadlpokm100% (1)
- Dalit LiteratureDocument16 pagesDalit LiteratureVeena R NNo ratings yet
- Questions DR JekyllDocument4 pagesQuestions DR JekyllMaRieNo ratings yet
- 5.2.1 1539323575 2163Document30 pages5.2.1 1539323575 2163Brinda TNo ratings yet
- Application of Neutralization Titrations for Acid-Base AnalysisDocument21 pagesApplication of Neutralization Titrations for Acid-Base AnalysisAdrian NavarraNo ratings yet
- Safe Handling of Solid Ammonium Nitrate: Recommendations For The Environmental Management of Commercial ExplosivesDocument48 pagesSafe Handling of Solid Ammonium Nitrate: Recommendations For The Environmental Management of Commercial ExplosivesCuesta AndresNo ratings yet
- 14.marifosque v. People 435 SCRA 332 PDFDocument8 pages14.marifosque v. People 435 SCRA 332 PDFaspiringlawyer1234No ratings yet
- Brinker Insider Trading SuitDocument5 pagesBrinker Insider Trading SuitDallasObserverNo ratings yet
- Topic 8 - Managing Early Growth of The New VentureDocument11 pagesTopic 8 - Managing Early Growth of The New VentureMohamad Amirul Azry Chow100% (3)
- The Beatles - Allan Kozinn Cap 8Document24 pagesThe Beatles - Allan Kozinn Cap 8Keka LopesNo ratings yet