Professional Documents
Culture Documents
Immunotechniques 2
Uploaded by
Rekha Govindan0 ratings0% found this document useful (0 votes)
26 views17 pagesOriginal Title
Immunotechniques 2.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views17 pagesImmunotechniques 2
Uploaded by
Rekha GovindanCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 17
Animal models are used for the study of a number of human
autoimmune diseases, including multiple sclerosis, diabetes,
rheumatoid
arthritis,
systemic
lupus
erythematosis
and
spondyloarthropathies. Induced, spontaneous and genetically
manipulated animal models can be described in terms of their
parallels to human disease and as valuable tools for the
development of potential therapies. Studies in animal models have
led to a number of important discoveries, which have increased our
understanding of the pathogenesis of autoimmune disease,
including the roles played by regulatory T cells and TH17 cells. In
addition, important therapeutic advances have emerged as a result
of studies of immune intervention in animal models of autoimmunity.
For example, tumour necrosis factor (TNF) blocking drugs, which are
widely used for the treatment of rheumatic diseases, were
developed following preclinical testing in animal models.
Animal models may be either spontaneously occurring or induced as
a result of genetic manipulation, immunization with a selfantigen or
triggered by pathogenassociated molecular patterns (PAMPs) in
genetically susceptible hosts.
No animal model completely mimics human disease.
Animal models can be used to delineate common mammalian
immunological mechanisms, test novel therapeutic concepts and
Immune complexes derive from complex interactions
between antibody, antigens, complement and various
receptors as a part of adaptive immunity. Antigens bound to
antibodies in immune complexes are normally cleared by
various cellular mechanisms physiologically capable of
eliminating even small quantities of foreign antigens from
circulation. Immune complexes can form when humans are
exposed to foreign substances like proteins (infections,
vaccines, drugs, etc.) or nonprotein materials (haptens)
which need a protein carrier to activate the cascade.
Autoimmune disorders develop when immune complexes
deposit pathologically in different organs, initiating
inflammatory cascades which lead to organ damage/disease.
Immune complex disease can manifest in a myriad of ways
when dysregulation in one or more of these components
occur. Even some recombinant protein therapeutic agents
used to treat autoimmunity may paradoxically form immune
complexes,
neutralizing
therapeutic
efficacy
and/or
manifesting as immune complex disease.
Latticed immune complexes are pathologically capable of depositing
systemically in any of a variety of tissue sites, creating downstream
cellular damage with many different clinical presentations, all of
which fall into the category of immune complex disease (the
prototype originally being referred to as serum sickness).
Several experimental animal models of immune complex disease
have emerged yielding useful information on the cellular and soluble
elements involved in its pathogenesis.
Immune complex disease in humans is seen primarily in the setting
of infection and/or in response to various therapeutic agents of
protein or nonprotein nature.
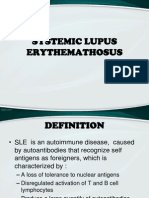
Adaptive immunity has also evolved to readily discriminate between
self and foreign antigens. Loss of ability to recognize selfantigens
results in Autoimmunity in which both cellular and soluble immune
responses against selfantigens pathologically occur.
Many different autoimmune disorders in humans feature immune
complex disease manifestations and generally derive from unknown
selfantigens complexed to selfantibodies. Even some recombinant
protein therapeutic agents used to treat autoimmunity may induce
formation of immune complexes, neutralizing therapeutic efficacy
and/or manifesting as immune complex disease.
You might also like
- UntitledDocument63 pagesUntitledRekha GovindanNo ratings yet
- UntitledDocument115 pagesUntitledRekha GovindanNo ratings yet
- UntitledDocument59 pagesUntitledRekha GovindanNo ratings yet
- UntitledDocument67 pagesUntitledRekha GovindanNo ratings yet
- Report - Session 1Document1 pageReport - Session 1Rekha GovindanNo ratings yet
- T&P Cell, GCAS Androth Brochure 07-01-2023Document21 pagesT&P Cell, GCAS Androth Brochure 07-01-2023Rekha GovindanNo ratings yet
- Nano Particles Conventional Vaccines: Nano Vaccines For Effective Treatment of Hepatitis BDocument1 pageNano Particles Conventional Vaccines: Nano Vaccines For Effective Treatment of Hepatitis BRekha GovindanNo ratings yet
- Poster 17th Dec 2012Document1 pagePoster 17th Dec 2012Rekha GovindanNo ratings yet
- Animal Biotechnology - ScopeDocument29 pagesAnimal Biotechnology - ScopeRekha GovindanNo ratings yet
- Plant GenomeDocument31 pagesPlant GenomeRekha GovindanNo ratings yet
- Immunotechniques 1Document53 pagesImmunotechniques 1Rekha GovindanNo ratings yet
- Unit II - 3. Protein Super Secondary Structures & Toplogy DiagramsDocument31 pagesUnit II - 3. Protein Super Secondary Structures & Toplogy DiagramsRekha GovindanNo ratings yet
- Human Epidermal Growth Factor (EGF) Is A 6045-Da Protein With 53 Amino Acid Residues and Three Intramolecular Disulfide Bonds (MR: 6,100)Document13 pagesHuman Epidermal Growth Factor (EGF) Is A 6045-Da Protein With 53 Amino Acid Residues and Three Intramolecular Disulfide Bonds (MR: 6,100)Rekha GovindanNo ratings yet
- Sheep Antiserum - Lysis: Cholerae CellsDocument35 pagesSheep Antiserum - Lysis: Cholerae CellsRekha GovindanNo ratings yet
- Immunotechniques 1Document53 pagesImmunotechniques 1Rekha GovindanNo ratings yet
- Alpha Domain StructureDocument35 pagesAlpha Domain StructureRekha Govindan100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Campbell Smith - Harris032311Document2 pagesCampbell Smith - Harris032311Heather X RhodesNo ratings yet
- Foreign Body Reactions, Marginal Bone Loss and Allergies in Relation To Titanium Implants AlbrektssonDocument11 pagesForeign Body Reactions, Marginal Bone Loss and Allergies in Relation To Titanium Implants AlbrektssonImplantologia Oral y ReconstructivaNo ratings yet
- PBL 1 ThyrotoxicosisDocument7 pagesPBL 1 ThyrotoxicosishappyhappylandNo ratings yet
- Get Your Life Back Thyroid Health MANUAL PDF 1 by Kim Wolinski FINALDocument52 pagesGet Your Life Back Thyroid Health MANUAL PDF 1 by Kim Wolinski FINALKrn Glez100% (8)
- SLE MedscapeDocument49 pagesSLE MedscapeAndino FadilNo ratings yet
- Diseases of The Immune System: OBC 231 General PathologyDocument91 pagesDiseases of The Immune System: OBC 231 General PathologyRana MohammadNo ratings yet
- Tolerance and Autoimmunity-NEJMDocument10 pagesTolerance and Autoimmunity-NEJMAsep HrNo ratings yet
- Final Internship PresentationDocument25 pagesFinal Internship PresentationSaira JabeenNo ratings yet
- EBM TerbaruDocument5 pagesEBM TerbaruTetty PrasetyaNo ratings yet
- Eponyms SyndromesDocument23 pagesEponyms Syndromestekennn021No ratings yet
- Systemic Enzyme Therapy Experience With Wobenzym FormulationsDocument124 pagesSystemic Enzyme Therapy Experience With Wobenzym Formulationsfpm5948100% (4)
- MR Supple All 2014Document429 pagesMR Supple All 2014Regita Ayu LestariNo ratings yet
- Genetics) SyllabusDocument33 pagesGenetics) Syllabusb.duttaNo ratings yet
- A Doctor's 4-Step Program To Treat Autoimmune Disease: THE IMMUNE SYSTEM RECOVERY PLAN by Susan BlumDocument65 pagesA Doctor's 4-Step Program To Treat Autoimmune Disease: THE IMMUNE SYSTEM RECOVERY PLAN by Susan BlumSimon and Schuster85% (26)
- COVID-19 and Autoimmune DiseasesDocument8 pagesCOVID-19 and Autoimmune DiseasesMan'SzAr'diAnSyAhNo ratings yet
- Diabetes Mellitus in Children (Pedi Clinics of N. America Vol 52, No 6) WW PDFDocument275 pagesDiabetes Mellitus in Children (Pedi Clinics of N. America Vol 52, No 6) WW PDFEliMihaelaNo ratings yet
- PReS 2022 Final Programme Vscreen2Document88 pagesPReS 2022 Final Programme Vscreen2Mike KrikNo ratings yet
- Lecture 10 AutoimmunityDocument78 pagesLecture 10 AutoimmunitytimcarasNo ratings yet
- Jurnal SleDocument2 pagesJurnal SlePratidina Dwinda HENo ratings yet
- NewsArchives PDFDocument392 pagesNewsArchives PDFkitty katNo ratings yet
- Polyglandular Autoimmune Syndrome FinallDocument24 pagesPolyglandular Autoimmune Syndrome FinallnayabNo ratings yet
- Systemic Lupus ErythemathosusDocument23 pagesSystemic Lupus ErythemathosusFransisca HardimartaNo ratings yet
- Sofia Mubarika 180522Document42 pagesSofia Mubarika 180522Nanik AndianiNo ratings yet
- Low Level Laser Therapy (LLLT) - Photobiomodulation (PBM) - Red - NIR Phototherapy Studies - A Comprehensive Database by Vladimir Heiskanen - Taulukko1Document76 pagesLow Level Laser Therapy (LLLT) - Photobiomodulation (PBM) - Red - NIR Phototherapy Studies - A Comprehensive Database by Vladimir Heiskanen - Taulukko1nepretipNo ratings yet
- The Inflamed Mind by Edward BullmoreDocument12 pagesThe Inflamed Mind by Edward Bullmoresimas100% (1)
- Etiopathogenesis of Diabetes MellitusDocument35 pagesEtiopathogenesis of Diabetes MellitusironNo ratings yet
- Approaches To Diagnosis Celiac DiseaseDocument16 pagesApproaches To Diagnosis Celiac DiseaseJunior GrobeNo ratings yet
- Weetman-Immunology - of - PregnancyDocument4 pagesWeetman-Immunology - of - PregnancyPaul Alwin KhomanNo ratings yet
- Colloidal GoldDocument6 pagesColloidal Goldambertje12No ratings yet
- L24 AutoimmDocument35 pagesL24 AutoimmFadli FadelNo ratings yet