Professional Documents
Culture Documents
Acute Kidney Injury - Mini Lecture: Updated 02/2013
Uploaded by
Asmalina AzizanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Kidney Injury - Mini Lecture: Updated 02/2013
Uploaded by
Asmalina AzizanCopyright:
Available Formats
TEACHING RESEARCH PUBLIC SERVICE
Acute Kidney Injury - Mini Lecture
Updated 02/2013
Objectives
Quickly and easily identify and workup acute
kidney injury.
Background
The incidence of AKI is estimated at 1% of patients that
present to the hospital and 7-50% of patients in the ICU.
Part of the initial history should be determining every
patients baseline Cr.
May present as Uremia (malaise, anorexia, nausea,
vomiting), but is usually asymptomatic.
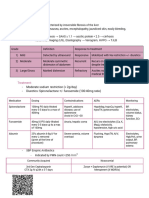
Acute Kidney Injury Network (AKIN) Criteria
Stage Cr Criteria UOP Criteria
1 Crby 1.5-2x baseline or < 0.5 ml/kg/hr for 6hr
Crby 0.3 mg/dl
2 Crby 2-3x < 0.5 ml/kg/hr for 12hr
3 Crby more than 3x or Crby < 0.3 ml/kg/hr for 24hr
0.5 if baseline >4mg/dl Or anuria for 12h
AKI can be Prerenal, Intrinsic or Postrenal
Acute Kideny Injury
Prerenal
Postrenal
Uosm > 5000 mosm/kg
Uosm: variable
Una < 20meq/L
FEna < 1% Intrinsic Renal Diseases Una: low early, high late
FEna: variable
Microscopy - bland
Microscopy - bland
Acute Interstitial Nephritis Acute Glomerulonephritis
Ischemic / Toxic ATN
Uosm: variable, ~300 mosm.kg Uosm: variable (>400 in early GN)
Uosm ~ 300 mosm/kg
Una > 40 meq/L Una: variable (<20meq/l in early GN)
Una > 40meq/L FEna: variable, <1% in early GN
FEna > 2%
FEna > 2% Microscopy hematuria, proteinuria
Microscopy leukocytes,
Microscopy dark pigment cast Erythrocyte casts (dysmorphic)
erythrocyts, leukocyte casts
Prerenal Azotemia
Prerenal azotemia is the most common cause of
acute kidney injury in the outpatient setting
Look for patients with decreased PO, diarrhea,
vomiting, tachycardia, orthostasis.
Order: UA, Uosm, Una, Ucr, BMP, Uurea (if on
diuretics)
The kidney functions properly in patients with
prerenal azotemia.
True volume depletion can be treated with normal
saline.
Decreased effective arterial blood volume can be
present in CHF, Cirrhosis or nephrotic syndrome.
Treatment should focus on the underlying disease.
Intrinsic Kidney Diseases
ATN - Acute Tubular Necrosis
Usually occurs after an ischemic event or exposure to
nephrotoxic agents.
Look for muddy brown casts and FeNa>2%
AIN - Acute Interstitial Nephritis
Classic presentation is fever, rash, eosinophilia and Cr bump 7-
10 days after drug exposure.
Urine may show leukocytes, leukocyte casts and erythrocytes,
cultures will be negative.
CIN - Contrast Induced Nephropathy
Increased Cr of 0.5mg/dl or 25% 48hrs after contrast
administration.
Prevent with NS or isotonic fluid+sodium bicarb, hold NSAIDs,
metformin and diuretics (in patients without fluid overload).
Others Glomerular Disease, Pigmented Nephropathy,
Thrombotic Microangiopathy
Postrenal Disease
Obstruction anywhere in the urinary tract
Bladder outlet obstruction can be seen with bladder
scan and relieved with catheterization
Ureteral obstruction and hydronephrosis may be seen
on ultrasound and noncontrast CT
Order: Order: UA, Uosm, Una, Ucr, BMP, Uurea (if on
diuretics)
Patients often have a history of pelvic tumors,
irradiation, congential abnormalities, kidney
stones, genitourinary, procedures or surgeries,
and prostatic enlargement.
AKI can be Prerenal, Intrinsic or Postrenal
Acute Kideny Injury
Prerenal
Postrenal
Uosm > 5000 mosm/kg
Uosm: variable
Una < 20meq/L
FEna < 1% Intrinsic Renal Diseases Una: low early, high late
FEna: variable
Microscopy - bland
Microscopy - bland
Acute Interstitial Nephritis Acute Glomerulonephritis
Ischemic / Toxic ATN
Uosm: variable, ~300 mosm.kg Uosm: variable (>400 in early GN)
Uosm ~ 300 mosm/kg
Una > 40 meq/L Una: variable (<20meq/l in early GN)
Una > 40meq/L FEna: variable, <1% in early GN
FEna > 2%
FEna > 2% Microscopy hematuria, proteinuria
Microscopy leukocytes,
Microscopy dark pigment cast Erythrocyte casts (dysmorphic)
erythrocyts, leukocyte casts
Practice Question
A 74 year old man was hospitalized 3 days ago with
cellulitis. He has a history of HTN, HLD, PVD and has
been non-compliant with his medications. At presentation,
his vitals were T-37, BP-170/90, HR-90, RR-20 and Cr was
1.5. He was started on Cefazolin and his home meds
(Lisinopril, Metoprolol, HCTZ, Amolodipine, Pravastatin and
ASA) were restarted.
Today, his vitals are T-37, BP-110/55, HR-60, RR-16
and his Cr is 2.7, FeNa-2.3%, FeUrea-51%, UA shows
trace protein and occasional Granular casts. UOP has been
stable.
What is the most likely cause of his AKI?
A. Acute Interstitial Nephritis
B. Benign Prostate Hypertrophy
C. Acute Tubular Necrosis
D. Prerenal Azotemia
Take Home Points
Identify AKI early on
Monitor serum Cr for at risk patients
Make sure I/Os are recorded correctly
Diagnose as Prerenal, Intrinsic or Postrenal
Detailed history
Order routine labs including BMP, UA, Uosm, Ucr,
Una (Urine Urea if on diuretics)
Imaging studies as necessary
Begin appropriate treatment
Stop offending agent
Fluids if appropriate
Relieve obstruction
Renal dosing of meds
Thank You
You might also like
- Acute Kidney Injury (AKI) GuideDocument26 pagesAcute Kidney Injury (AKI) GuideWhulandary DyaswaraNo ratings yet
- 35 Rivara Matthew Workup and Management of Acute KidnDocument50 pages35 Rivara Matthew Workup and Management of Acute KidnDenisse Tinajero SánchezNo ratings yet
- 12a. Kuliah Aki 2017Document36 pages12a. Kuliah Aki 2017yussikafernandaNo ratings yet
- Acute Kidney Injury (AKI)Document50 pagesAcute Kidney Injury (AKI)Omar AbdillahiNo ratings yet
- Gagal GinjalDocument75 pagesGagal GinjalAndi HeriantoNo ratings yet
- Acute Kidney Injury Ok Prof SyakibDocument49 pagesAcute Kidney Injury Ok Prof SyakibIndrawati MalotesNo ratings yet
- Renal Acute Kidney InjuryDocument41 pagesRenal Acute Kidney InjuryTim SilvaNo ratings yet
- Acute Kidney Injury (AKI) : Haerani Rasyid FK Unhas 2016Document46 pagesAcute Kidney Injury (AKI) : Haerani Rasyid FK Unhas 2016Ana Yusriana AzzahraNo ratings yet
- Aki - CKDDocument51 pagesAki - CKDAyu Luh Ratri WeningNo ratings yet
- 11.0 Acute Kidney InjuryDocument26 pages11.0 Acute Kidney InjuryHeny KsNo ratings yet
- Acute Kidney Injury: Syakib BakriDocument46 pagesAcute Kidney Injury: Syakib BakriBhisma D. SyaputraNo ratings yet
- AKI FlowchartDocument1 pageAKI FlowchartTush RameNo ratings yet
- Acute Kidney InjuryDocument26 pagesAcute Kidney InjuryUmmuhani AbubakarNo ratings yet
- Acute Renal Failure Definition and CausesDocument33 pagesAcute Renal Failure Definition and Causesimranqazi11No ratings yet
- 1 Acute Renal FailureDocument65 pages1 Acute Renal FailureDammaqsaa W BiyyanaaNo ratings yet
- Acute Kidney InjuryDocument34 pagesAcute Kidney Injury* mokhtar !!No ratings yet
- C370 Lecture 1 Lecture Notes Part 2Document54 pagesC370 Lecture 1 Lecture Notes Part 2Yan Mui ChanNo ratings yet
- Pulmonology algorithms and pneumonia risk factorsDocument117 pagesPulmonology algorithms and pneumonia risk factorsEm TimbolNo ratings yet
- Acute Kidney Injury AKIDocument6 pagesAcute Kidney Injury AKIfazeel shah vlogsNo ratings yet
- OR CommsDocument4 pagesOR CommsAngela NeriNo ratings yet
- Cardinal Manifestations of Renal DiseaseDocument36 pagesCardinal Manifestations of Renal DiseaseJewelNo ratings yet
- MRCP 2 Nephrology NOTESDocument74 pagesMRCP 2 Nephrology NOTESMuhammad HaneefNo ratings yet
- Acute Kidney InjuryDocument42 pagesAcute Kidney InjurysushmaNo ratings yet
- Acute Kidney Injury: Dana BabaDocument31 pagesAcute Kidney Injury: Dana Babanaheel98shNo ratings yet
- Infectiile de tract urinar: cazuri cliniceDocument55 pagesInfectiile de tract urinar: cazuri cliniceMădălina Mihaela LuchianNo ratings yet
- AKI in OBSTETRICSDocument41 pagesAKI in OBSTETRICSDebajyoti DasNo ratings yet
- Urological Emergencies: Julian ManderDocument43 pagesUrological Emergencies: Julian ManderDara MirandaNo ratings yet
- Adult T-Cell Leukemia Lymphoma (Atll) A Rare Case Associated With Human T-Cell Virus (Htlv-1)Document19 pagesAdult T-Cell Leukemia Lymphoma (Atll) A Rare Case Associated With Human T-Cell Virus (Htlv-1)Priya ChandakNo ratings yet
- Acute Renal FailureDocument196 pagesAcute Renal FailureyvonneNo ratings yet
- Acute Kidney Injury (AKI) : by Prof Grace Irimu Consultant Pediatrician and NephrologistDocument43 pagesAcute Kidney Injury (AKI) : by Prof Grace Irimu Consultant Pediatrician and Nephrologistokwadha simionNo ratings yet
- Management of Acute Kidney InjuryDocument31 pagesManagement of Acute Kidney InjurysumitNo ratings yet
- AKI - Icu Diagnosis and Management: Dr. Muhamed Al Rohani, MD, FISNDocument39 pagesAKI - Icu Diagnosis and Management: Dr. Muhamed Al Rohani, MD, FISNlisaNo ratings yet
- Contora, Isah TblrenalDocument7 pagesContora, Isah TblrenalisahNo ratings yet
- 22.AKI ProtocolDocument2 pages22.AKI ProtocolRed DevilNo ratings yet
- An Update On Diagnosis Treatment: Ilson DiseaseDocument46 pagesAn Update On Diagnosis Treatment: Ilson DiseaseJuwita PratiwiNo ratings yet
- TURP Procedure ExplainedDocument36 pagesTURP Procedure ExplainedRight VentricleNo ratings yet
- AKI, CKD SummaryDocument4 pagesAKI, CKD SummaryMuathNo ratings yet
- Acute Renal Failure: Anthony R Mato, MDDocument81 pagesAcute Renal Failure: Anthony R Mato, MDasad_channa1No ratings yet
- Prof. Syakib Acute Kidney Injury - Internal Medicine Emergency Course - Agustus 2019-DikonversiDocument35 pagesProf. Syakib Acute Kidney Injury - Internal Medicine Emergency Course - Agustus 2019-DikonversidrroytambunanNo ratings yet
- Table of Content: Post-Streptococcal Glomerulonephritis 3Document5 pagesTable of Content: Post-Streptococcal Glomerulonephritis 3rup100% (1)
- Pulmonary EmbolismDocument27 pagesPulmonary EmbolismEfren Ezekiel AlbiosNo ratings yet
- Nefrologi: I Gusti Ngurah Agung Tresna ErawanDocument69 pagesNefrologi: I Gusti Ngurah Agung Tresna ErawanDian PritaNo ratings yet
- General Medical Principles for Electrolytes, Insulin, Ventilators & MoreDocument5 pagesGeneral Medical Principles for Electrolytes, Insulin, Ventilators & MoreNisha DNo ratings yet
- Acute Kidney Injury: Anwesha Mukherjee PGT ICHDocument27 pagesAcute Kidney Injury: Anwesha Mukherjee PGT ICHSabyasachi RoyNo ratings yet
- Acute Renal FailureDocument50 pagesAcute Renal FailureEster Libunao DollagaNo ratings yet
- Acute Kidney Injury: Causes, Stages, and ManagementDocument62 pagesAcute Kidney Injury: Causes, Stages, and ManagementApidha KartinasariNo ratings yet
- Kidney Emergency: M. Syamsul BakhriDocument30 pagesKidney Emergency: M. Syamsul BakhrierahadeNo ratings yet
- Bloody vomiting and melena case summariesDocument16 pagesBloody vomiting and melena case summariesmiaNo ratings yet
- UPDATE ON SNAKE BITE MANAGEMENTDocument24 pagesUPDATE ON SNAKE BITE MANAGEMENTkholishatul widadNo ratings yet
- Anestesi Pada Pasien Gangguan GinjalDocument28 pagesAnestesi Pada Pasien Gangguan GinjallovianettesherryNo ratings yet
- Kidney Disease Stages: When to Refer for Specialist CareDocument50 pagesKidney Disease Stages: When to Refer for Specialist CareRogerQuxNo ratings yet
- Nephrology DR ZeinabDocument101 pagesNephrology DR ZeinabZeinab Muhammad100% (1)
- Renal EmergenciesDocument8 pagesRenal EmergenciesRENEROSE TORRESNo ratings yet
- Pharma Pass Medicin 2020Document654 pagesPharma Pass Medicin 2020VikrantNo ratings yet
- Cirrhosis SBPDocument9 pagesCirrhosis SBPapi-690342013No ratings yet
- Urological Emergencies: DR Ahmed BekeerDocument31 pagesUrological Emergencies: DR Ahmed BekeerAh BakaNo ratings yet
- Tubules and Interstitium: Diseases of The KidneyDocument46 pagesTubules and Interstitium: Diseases of The Kidneyعوض الكريمNo ratings yet
- Acute Renal Failure - Dr. Wael Omar (AQH) : Functions of The KidneyDocument3 pagesAcute Renal Failure - Dr. Wael Omar (AQH) : Functions of The KidneyasdddNo ratings yet
- Fast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteFrom EverandFast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteNo ratings yet
- Fast Facts: Acute and Recurrent Pancreatitis: Using evidence to support treatmentFrom EverandFast Facts: Acute and Recurrent Pancreatitis: Using evidence to support treatmentNo ratings yet
- Fluid TherapiDocument158 pagesFluid TherapiAsmalina AzizanNo ratings yet
- CKD Presentation1Document19 pagesCKD Presentation1Husnawaty DayuNo ratings yet
- The Primary/secondary Care InterfaceDocument48 pagesThe Primary/secondary Care InterfaceAsmalina AzizanNo ratings yet
- Dear SirDocument1 pageDear SirAsmalina AzizanNo ratings yet
- Cedera SpinalDocument45 pagesCedera SpinalAsmalina AzizanNo ratings yet
- Dear SirDocument1 pageDear SirAsmalina AzizanNo ratings yet
- What Is Congestive Heart Failure (CHF)Document17 pagesWhat Is Congestive Heart Failure (CHF)Asmalina AzizanNo ratings yet
- Mutabaah AmalDocument1 pageMutabaah AmalAsmalina AzizanNo ratings yet
- Life Is Too Short To Be Taken Insignifican TLYDocument3 pagesLife Is Too Short To Be Taken Insignifican TLYAsmalina AzizanNo ratings yet
- Mutabaah AmalDocument1 pageMutabaah AmalAsmalina AzizanNo ratings yet
- Cell DivisionDocument9 pagesCell DivisionAsmalina AzizanNo ratings yet
- Task 1 - Email Template v2Document2 pagesTask 1 - Email Template v2Amardeep TayadeNo ratings yet
- Chemisty - How Hot Are ChillisDocument6 pagesChemisty - How Hot Are ChillisMSHYDERABAD4334No ratings yet
- Is English's Status as the Global Language AssuredDocument5 pagesIs English's Status as the Global Language AssuredfsdfsdfasdfasdsdNo ratings yet
- Proteose Peptone for Cultivating MicroorganismsDocument1 pageProteose Peptone for Cultivating MicroorganismscinthiaNo ratings yet
- Is 3427-1997 (Iec 298-1990) - Switch Gear &contrl GearDocument68 pagesIs 3427-1997 (Iec 298-1990) - Switch Gear &contrl Gearjerinmathew2220No ratings yet
- Suzuki DieselDocument746 pagesSuzuki DieselDante Allegro100% (1)
- HE7200A HE100A Flight Manual Supplement (FMS)Document7 pagesHE7200A HE100A Flight Manual Supplement (FMS)HozyaNo ratings yet
- BSBCRT511 Project Portfolio - Revised - Answers IncludedDocument26 pagesBSBCRT511 Project Portfolio - Revised - Answers IncludedShivanee JhaumalNo ratings yet
- CORRELATION RANK COEFFICIENTDocument23 pagesCORRELATION RANK COEFFICIENTSomhita Chakraborty100% (3)
- 40L Insufflator Repair ProcedureDocument13 pages40L Insufflator Repair ProcedureErnesto GarcíaNo ratings yet
- Cekungan Tomori Dan SalawatiDocument17 pagesCekungan Tomori Dan SalawatiDimas WijayaNo ratings yet
- Optimal Diet and Furniture Shop ProductionDocument7 pagesOptimal Diet and Furniture Shop ProductionBeatriz ArevaloNo ratings yet
- Review Development Economics - 2020 - Memon - Income Inequality and Macroeconomic InstabilityDocument32 pagesReview Development Economics - 2020 - Memon - Income Inequality and Macroeconomic InstabilityTAhmedNo ratings yet
- RFBT-13 (Banking Laws)Document10 pagesRFBT-13 (Banking Laws)Alliah Mae ArbastoNo ratings yet
- If TRLDocument38 pagesIf TRLbdNo ratings yet
- OTTO - SMART ROBOT ARCHITECTUREDocument1 pageOTTO - SMART ROBOT ARCHITECTURESuscripcion BelaundeNo ratings yet
- Entreprenuership - Case Example 1 Double HappinessDocument2 pagesEntreprenuership - Case Example 1 Double HappinessRonan FerrerNo ratings yet
- RtclogDocument89 pagesRtclogMalvin ReynNo ratings yet
- IA 3 - ViscosityDocument9 pagesIA 3 - ViscosityManav Shah100% (1)
- MCC Codes 0220Document37 pagesMCC Codes 0220JoelNo ratings yet
- Hyster H135-155XL Parts Manual G006 PDFDocument376 pagesHyster H135-155XL Parts Manual G006 PDFEwerton Bianchi89% (9)
- The Munda LanguagesDocument808 pagesThe Munda LanguagesAjenjo Mata100% (2)
- Intermediary Details Name Code Contact Number Care Health Insurance Ltd. Direct 1800-102-6655Document4 pagesIntermediary Details Name Code Contact Number Care Health Insurance Ltd. Direct 1800-102-6655Mahakaal Digital PointNo ratings yet
- Virtual SAN (VSAN) DatasheetDocument2 pagesVirtual SAN (VSAN) DatasheetOscarNo ratings yet
- Anatomy of EarDocument42 pagesAnatomy of EarHesti hasanNo ratings yet
- Student Pain Management Fundamental ReasoningDocument7 pagesStudent Pain Management Fundamental ReasoningSharon TanveerNo ratings yet
- Food Crices in IndiaDocument4 pagesFood Crices in IndiaAkhi GuveraNo ratings yet
- Philippines: Asian Development Bank Member Fact SheetDocument4 pagesPhilippines: Asian Development Bank Member Fact SheetShekinah CastrosantoNo ratings yet
- MCS in NepalDocument8 pagesMCS in NepalSourabh InaniNo ratings yet
- Castle Leasing Corporation Which Uses Ifrs Signs A Lease Agreement PDFDocument1 pageCastle Leasing Corporation Which Uses Ifrs Signs A Lease Agreement PDFFreelance WorkerNo ratings yet