Professional Documents
Culture Documents
CVP
Uploaded by
meisin kuraesin0 ratings0% found this document useful (0 votes)
63 views13 pagesCvp
Original Title
Cvp
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCvp
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
63 views13 pagesCVP
Uploaded by
meisin kuraesinCvp
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 13
Central Venous Pressure and
Central lines
Hery Prayitno, M.Kep
ICU RS IMMANUEL
BANDUNG
Challenging Knowledge
Before starting this module; Answer the
following questions
(1) What sites are used to site a CVL?
(2) What is the normal CVP?
(3) What are the basic treatments for a CVP
of -1cm of H20
(4) What are the essential items required to
measure a CVP?
Learning Outcomes
By the end of this module you should
(1) Be aware of factors which affect the CVP
(2) Recognise normal and abnormal CVP values
(3) Be able to set up the manometer system to
measure a patients CVP
(4) Be able to measure a CVP and interpret the
value
(5) Be aware of the initial management for high and
low values
Factors affecting the CVP
The central venous pressure reflects the right atrial pressure
(RAP) and is similar to measuring the JVP clinically
The factors which affect the CVP are:-
Systemic vasodilatation and hypovolaemia, which leads to
reduced venous return in the vena cava and reduced RAP
Right ventricular failure
Tricuspid and Pulmonary valve disease
Pulmonary hypertension
Right ventricular dysfunction and pulmonary hypertension leads
to raised right atrial pressure, as does tricuspid and pulmonary
stenosis.
Central venous line (CVL)
Indications for CVL
Severe hypovolaemia requiring rapid infusion
(although initial resuscitation may be peripheral through wide bore cannulae)
Infusion of drugs which may cause peripheral
problems e.g. vasoconstriction, phlebitis
Measurement of central venous pressure (CVP)
Confirmation of diagnosis e.g. Right heart failure
Insertion of a pacing wire.
Sites for insertion Internal jugular, subclavian
and femoral vein; Long lines are also inserted in
the brachial vein.
How to measure the CVP using a manometer system
The CVP system
A bag of saline or dextrose = reservoir
Three way tap - connected to
manometer, reservoir and patients CVL
by tubing; System is primed with fluid
before starting
Patient
Patient is lying supine if possible positioned
Manometer has spirit level at zero; supine on
Zero point is aligned with right atrium the bed
using the mid axillary line / 4th ICS
Measurements should be taken with the
patient in the same position each time
using the spirit level; the zero point on
the skin surface is marked for
consistency of measurement Three way tap
How to measure the CVP using a manometer system
Turn the three way tap OFF to the
patient.
Fill the manometer to the top from the
reservoir
Turn the three way tap OFF to the
reservoir
This means the column of fluid is
supported only by the RAP / CV
pressure
The column will fall according to
CVP
The column swings with respiration -
conventionally the level is taken as the
mean.
Three way tap OFF to the Three way tap OFF to the
patient allowing the reservoir allowing the
manometer to be filled CVP to be measured
Normal CVP measurements
The normal CVP is between 5 10 cm of
H2O (it increases 3 5 cm H2O when
patient is being ventilated)
In high dependency areas an electronic
transducer is connected instead of the
manometer system. This gives a continuous
readout of CVP along with a display of the
waveform. This may be measured in
mmHg.
(Note:10 cmH20 = 7.5mmHg =1kPa)
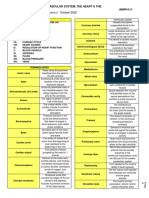
CVP Reading Other clinical Diagnosis Treatment
features
Low Tachycardia Hypovolaemia Fluid challenge until CVP
Low normal or hypotension within normal limits and
Urine output oligo or anuria treat underlying cause
Low Tachycardia Fluid resuscitation (if low)
Sepsis
Signs of infection Antibiotics
( may be normal or Pyrexia
high due to Vasodilatation is most common but May require inotrope
severe sepsis maybe associated with support
venoconstriction) constriction
Normal due to Tachycardia
Hypovolaemia Fluid challenge and treat
Urine output underlying cause
venoconstriction falling below 30ml /hr
Poor capillary refill
High Dyspnoea with pulmonary Diuretics, GTN infusion,
crepitations
Heart failure
may require inotropes
Tachycardia with third heart sound
Tender hepatomegaly
Ascites
Peripheral Oedema
Very High Venous congestion and SVC obstruction Treat underlying
dilatation of face and Cardiac tamponade
neck; associated signs Tension pneumothorax
cause
Case (1) How low can you go?
A 32 year old woman with known
alcohol associated liver disease
presents with melaena. Initially she
is haemodynamically stable and
well perfused. She suddenly
decompensates with fresh blood
and clots being passed PR. Initial
resuscitation with several litres of
crystalloid and some colloid fails to
bring her systolic BP back above
100 mm Hg. A CVP line is inserted
and shows her CVP to be +1
cmH2O.
(a) What is the likely diagnosis?
(b) List your further management
including investigations and
medications
Case (2) CVP Pat pending
A 31 year old man presents to
A&E with a 3 month history of
night sweats and weight loss. On
examination he is unwell, pyrexial
and has several large cervical
lymph nodes. He is noted to have
poorly palpable radial pulse, a
positive Kussmauls sign and
poorly heard heart sounds. The
SHO decides to site a CVP which
is measured at 28 cm of H2O.
(a) What is the likely underlying
diagnosis?
(b) What is the initial treatment?
(c) How will you prove the
diagnosis?
Case (3)
A 48 year old poorly controlled Type 2 diabetic man is
admitted from the Diabetes clinic with a deep, infected foot
ulcer. His observations are: pulse 120bpm, BP 70/40, CVP +6
cm of H20 and he is noted to be sweaty and vasodilated.
Despite initial resuscitation with 3 litres of crystalloid in 4
hours, his BP and pulse fail to respond. He is electively
ventilated and admitted to ITU where he is started on
inotropes.
(1)What is the descriptive term given to this clinical state?
(2)List your further management?
Learning Outcomes
At the end of this module you should
(a) Be aware of the factors affecting the CVP.
(b) Be able to set up a CVP manometer
system.
(c) Be able to measure a CVP from a patient.
(d) Be able to interpret the result.
(e) Be able to institute initial management
based on the result.
You might also like
- CTS 5500 PDFDocument8 pagesCTS 5500 PDFCarlos GuanipaNo ratings yet
- The Heart Is Not A Pump - The Blood Moves The Heart, Not Vice VersaDocument14 pagesThe Heart Is Not A Pump - The Blood Moves The Heart, Not Vice VersagiovacaneNo ratings yet
- Circulatory SystemDocument22 pagesCirculatory Systemparitosh7_886026No ratings yet
- Grade-9 Lesson PlanDocument9 pagesGrade-9 Lesson PlanPristine Aila RoblesNo ratings yet
- ECMO ExplanationDocument16 pagesECMO Explanationbreaking nurse100% (1)
- 4.krisis Hipertensi IMELS 15Document41 pages4.krisis Hipertensi IMELS 15putusanggraNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- 780 Adult Cardio Resp Assess DSTDocument10 pages780 Adult Cardio Resp Assess DSTGursangeet Kaur100% (1)
- 116 ExamDocument14 pages116 ExamZhailyn Joy DumlaoNo ratings yet
- Medical Terminology LicentaDocument75 pagesMedical Terminology LicentaGabriel BarbarasaNo ratings yet
- Endocrine GlandDocument10 pagesEndocrine GlandRS100% (1)
- CHN Long Quiz 1Document11 pagesCHN Long Quiz 1jovan teopizNo ratings yet
- Chapter 12Document10 pagesChapter 12Mark Laurence GuillesNo ratings yet
- C C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMDocument4 pagesC C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMjohkieNo ratings yet
- AtireviewDocument163 pagesAtireviewGlory Mimi0% (1)
- Practice Questions (F & E)Document5 pagesPractice Questions (F & E)pbiluanNo ratings yet
- Answer Key For Comprehensive Exam XVDocument18 pagesAnswer Key For Comprehensive Exam XVQharts SajiranNo ratings yet
- Hypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumDocument5 pagesHypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumMelodia Turqueza GandezaNo ratings yet
- Lesson Plan: Class: Subject: Topic: Submitted byDocument10 pagesLesson Plan: Class: Subject: Topic: Submitted bysimonjosan67% (3)
- Ms Test-Questio 2Document24 pagesMs Test-Questio 2Jackie AbarraNo ratings yet
- Assessment of Hematologic Function and Treatment Modalities Assessment of Hematologic Function and Treatment ModalitiesDocument26 pagesAssessment of Hematologic Function and Treatment Modalities Assessment of Hematologic Function and Treatment ModalitiesEdelweiss Marie CayetanoNo ratings yet
- COAP-Medical-Surgical-Nursing-Gastrointestinal-System-30-Items-JIZ DE ORTEGADocument9 pagesCOAP-Medical-Surgical-Nursing-Gastrointestinal-System-30-Items-JIZ DE ORTEGANicole OrtegaNo ratings yet
- Universidad de Zamboanga Tiguma, Pagadian City Competency Appraisal II Pre Final ExamDocument5 pagesUniversidad de Zamboanga Tiguma, Pagadian City Competency Appraisal II Pre Final ExamKirsten SabanalNo ratings yet
- Gastrointestinal Disorders 1st ClassDocument70 pagesGastrointestinal Disorders 1st ClassBharat ThapaNo ratings yet
- Grand Coaching: Medical Surgical NursingDocument22 pagesGrand Coaching: Medical Surgical NursingEsarpy (Nana)No ratings yet
- Endocrine System Prepared By: Prof. Mike Chavez RN, USRNDocument7 pagesEndocrine System Prepared By: Prof. Mike Chavez RN, USRNMeiJoyFlamianoIINo ratings yet
- Nursing Management Pancreatic CancerDocument2 pagesNursing Management Pancreatic CancerKit NameKo100% (2)
- Hypertension NclexDocument5 pagesHypertension Nclexハニファ バランギNo ratings yet
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- CHNDocument3 pagesCHNDeen Philip OlegarioNo ratings yet
- CHN RVW 2Document51 pagesCHN RVW 2Michael UrrutiaNo ratings yet
- NCM 122 Ratio FinalsDocument2 pagesNCM 122 Ratio FinalsLorenz Jude CańeteNo ratings yet
- Diuretic Cases and Self-Test Questions With AnswersDocument19 pagesDiuretic Cases and Self-Test Questions With AnswersRoxana CaravețeanuNo ratings yet
- CetirizineDocument2 pagesCetirizinelintangNo ratings yet
- Siadh and Di QuestionsDocument18 pagesSiadh and Di QuestionsRegiever Salvante100% (1)
- Assessment Leadership Community Health 4 1Document14 pagesAssessment Leadership Community Health 4 1Royal Shop100% (1)
- GitDocument302 pagesGitjgcriste100% (7)
- Nur 111 Session 18 Sas 1Document11 pagesNur 111 Session 18 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Medical Surgical Nursing Review Questions Part 3Document8 pagesMedical Surgical Nursing Review Questions Part 3angelfire23phNo ratings yet
- P1 MS 3 Nur 200Document16 pagesP1 MS 3 Nur 200Xandra Joie Ondoy TabotaboNo ratings yet
- Biologic Crisis: Prepared By: Ronnie M. Amazona, RN, ManDocument162 pagesBiologic Crisis: Prepared By: Ronnie M. Amazona, RN, ManLex CatNo ratings yet
- Cushing's SyndromeDocument5 pagesCushing's SyndromesummerduskNo ratings yet
- ISBAR PneumoniaDocument1 pageISBAR PneumoniaLerma Pagcaliwangan0% (1)
- Volume ImpairmentDocument32 pagesVolume ImpairmentAcohCChaoNo ratings yet
- Infectious DiseasesDocument2 pagesInfectious DiseasesChuckie Miguel Axalan BacolodNo ratings yet
- Chapter 30 Nutrition and Digestive SystemDocument8 pagesChapter 30 Nutrition and Digestive SystemNeil Dave SuarezNo ratings yet
- Post Op Worksheet FinalDocument5 pagesPost Op Worksheet FinalRiza Angela BarazanNo ratings yet
- P1 RleDocument34 pagesP1 RleMary Jean GicaNo ratings yet
- 5 Bullets MS 3Document21 pages5 Bullets MS 3rihamNo ratings yet
- 100 Item MEDICAL SURGICAL Nursing Examination Correct Answers andDocument12 pages100 Item MEDICAL SURGICAL Nursing Examination Correct Answers andZyntrx VillasNo ratings yet
- Question Text: Clear My ChoiceDocument13 pagesQuestion Text: Clear My ChoiceLylibette Anne H. CalimlimNo ratings yet
- Body Fluid DistributionDocument56 pagesBody Fluid DistributionZoya Morani100% (1)
- Competency Appraisal - Diagnostic TestsDocument7 pagesCompetency Appraisal - Diagnostic TestsMj BrionesNo ratings yet
- Medical Surgical by Nursing CribDocument7 pagesMedical Surgical by Nursing Cribnursegian13100% (1)
- VerA Ok-Prelim Ncm104 (Autosaved) VeraDocument30 pagesVerA Ok-Prelim Ncm104 (Autosaved) Verajesperdomincilbayaua100% (1)
- IVT Procedure IDocument47 pagesIVT Procedure Izhallene813No ratings yet
- SKILL 8-16 Drawing Blood From A Central Venous Catheter: Key TermsDocument7 pagesSKILL 8-16 Drawing Blood From A Central Venous Catheter: Key TermsElizalde HusbandNo ratings yet
- GYNECOLOGICALNURSINGDocument4 pagesGYNECOLOGICALNURSINGSheana TmplNo ratings yet
- Discharge Planning ChecklistDocument6 pagesDischarge Planning ChecklistcutevivesNo ratings yet
- Dialysis Round Work Plan 2022 - للطلابDocument16 pagesDialysis Round Work Plan 2022 - للطلابAhmed SalahNo ratings yet
- Nle - July 2011Document12 pagesNle - July 2011shenric16100% (1)
- All The Questions in The Quiz Along With Their Answers Are Shown BelowDocument26 pagesAll The Questions in The Quiz Along With Their Answers Are Shown BelowRey Pama SaguireNo ratings yet
- Levofloxacin 500mg Film-Coated Tablets - Summary of Product Characteristics (SMPC)Document10 pagesLevofloxacin 500mg Film-Coated Tablets - Summary of Product Characteristics (SMPC)OdunlamiNo ratings yet
- Comprehensive Edited)Document82 pagesComprehensive Edited)mikrobyo_ng_wmsuNo ratings yet
- NCLEX Questions PneumoniaDocument2 pagesNCLEX Questions PneumoniaLovely Laranjo100% (1)
- Post Test ArellanoDocument11 pagesPost Test ArellanoMho Pimentel VanguardiaNo ratings yet
- Assessment TAsk PharmacodynamicsDocument2 pagesAssessment TAsk PharmacodynamicsMelvin Lazaro CabusoNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Journal Heptojugular RefluxDocument5 pagesJournal Heptojugular RefluxFarhan RezaNo ratings yet
- Diagnostic Assessment BeforeDocument4 pagesDiagnostic Assessment BeforeBinod KumarNo ratings yet
- Deep Breathing Relaxation For Decreasing Blood Pressure in People With HypertensionDocument5 pagesDeep Breathing Relaxation For Decreasing Blood Pressure in People With HypertensionFriska HarianjaNo ratings yet
- LA Myxoma Case PresentationDocument34 pagesLA Myxoma Case PresentationWiwik Puji LestariNo ratings yet
- Slide Deck ACS Referral Forum - DR Adhitia MIni Simposium ACSDocument20 pagesSlide Deck ACS Referral Forum - DR Adhitia MIni Simposium ACSsyahrial fazaNo ratings yet
- Nursing Care Plan and Drug StudyDocument4 pagesNursing Care Plan and Drug StudyEllaNo ratings yet
- Aortic StenosisDocument28 pagesAortic StenosisRizwanhoneyNo ratings yet
- Histo Lab Exercise #12Document8 pagesHisto Lab Exercise #12Gela ReyesNo ratings yet
- Medical Management: Medical and Surgical Management of Acute Myocardial InfarctionDocument4 pagesMedical Management: Medical and Surgical Management of Acute Myocardial InfarctionLouie ParillaNo ratings yet
- 1992 - Kaplan - Blood Pressure Measurement and MonitoringDocument33 pages1992 - Kaplan - Blood Pressure Measurement and MonitoringKTKL RSABNo ratings yet
- Simulation of The Cardiovascular Mechanical System Based On Pressure-Flow Model Rest ConditionDocument12 pagesSimulation of The Cardiovascular Mechanical System Based On Pressure-Flow Model Rest ConditionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Conceito de Pré Carga e Pós Carga em CardiologiaDocument9 pagesConceito de Pré Carga e Pós Carga em CardiologiarmesquitajrNo ratings yet
- IVABRADINEDocument9 pagesIVABRADINEIvan Darío Castillo OrozcoNo ratings yet
- Anatomy and Physiology of Cardiovascular SystemDocument2 pagesAnatomy and Physiology of Cardiovascular SystemKezzel Grace MaquillaNo ratings yet
- (Antonio Bayes de Luna, Miquel Fiol-Sala) The Surf (BookFi) PDFDocument349 pages(Antonio Bayes de Luna, Miquel Fiol-Sala) The Surf (BookFi) PDFherkamayaNo ratings yet
- Renal Blood Flow RegulationDocument3 pagesRenal Blood Flow RegulationTawhid ZihadNo ratings yet
- Austin Journal of Clinical CardiologyDocument15 pagesAustin Journal of Clinical CardiologyAustin Publishing GroupNo ratings yet
- Avoid Blood Clots in LegsDocument10 pagesAvoid Blood Clots in Legslewako4040No ratings yet
- Penyakit Jantung Iskemik: Dr. Abraham Avicenna, SPJPDocument31 pagesPenyakit Jantung Iskemik: Dr. Abraham Avicenna, SPJPradian diptaNo ratings yet
- P17F06.036.01 - Occlutech Patient Brochure PDA PDFDocument2 pagesP17F06.036.01 - Occlutech Patient Brochure PDA PDFHandyka Vb GNo ratings yet
- Hypertensive Urgency EmergencyDocument5 pagesHypertensive Urgency Emergencydamondouglas100% (3)
- 1.08 - The Cardiovascular System, The Heart & The Blood VesselsDocument9 pages1.08 - The Cardiovascular System, The Heart & The Blood Vessels13PLAN, SENTH RUEN, ANo ratings yet