Professional Documents
Culture Documents
Pathology of Teeth and Supporting Structures
Uploaded by
Isak Shatika0 ratings0% found this document useful (0 votes)
174 views45 pagesOriginal Title
Pathology of Teeth and Supporting Structures.ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
174 views45 pagesPathology of Teeth and Supporting Structures
Uploaded by
Isak ShatikaCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 45
Lecture 1
Pathology of Teeth and
Supporting Structures
Prof. Kogan E.A.
2016
Theeth Anatomy
Teeth are firmly implanted in the jaw and are
surrounded by the gingival mucosa .
The anatomic crown of the tooth projects
into the mouth and is covered by enamel, a
hard, inert,acellular tissuethe most highly
mineralized tissue in thebody.
The enamel rests upon dentin, which is a
specialized form of connective tissue that
makes up most of the remaininghard-tissue
portion of the tooth. Unlike enamel, dentin is
cellular and contains numerous dentinal
tubules, which containthe cytoplasmic
extensions of odontoblasts.
Cells line the interface between the dentin
and the pulp and can, when properly
stimulated, produce new (secondary) dentin
within the interior of the tooth
The pulp chamber itself is surroundedby the
dentin and consists of loose connective
tissue stroma rich in nerve bundles,
lymphatics, and capillaries.
Attachment
In mammals, teeth are attached to the alveolar
ridge of the jaws by the periodontal ligament,
which provides a strong yet fl exible attachment
that can withstand the forces of mastication. The
periodontal ligamentattaches to the alveolar
bone of the jaw on one side and to cementum,
present on the roots of the teeth, which acts as
a cement to anchor the periodontal ligament to
the tooth.
CARIES (TOOTH DECAY)
Dental caries, caused by focal degradation of the tooth structure,
is one of the most common diseases throughout the
world and is the most common cause of tooth loss before age
35.
Carious lesions are the result of mineral dissolution of
tooth structure by acid metabolic end products from bacteria
that are present in the oral cavity and are capable of fermenting
sugars.
Traditionally, the rate of caries has been higher in
industrialized countries, where there is ready access to processed
foods containing large amounts of carbohydrates.
Factors influence on
demographics of caries
The rate of caries has markedly dropped in countries
such as the United States, where improved oral hygiene and
fl uoridation of the drinking water has become a standard
practice.
Fluoride incorporates into the crystalline structure
of enamel, forming fl uoroapatite, and contributes to resistance
to degradation by bacterial acids.
Second, with globalization
of the worlds economy, increased amounts of processed
foods with high carbohydrate content are being imported into
developing nations. With these trends, one can expect the rate
of caries to increase dramatically in the less-developed world
over the next several decades
Types and stages of caries
Caries classification
Morphological stages of caries
Base and margines of caries
cavaty
Early caries
Superficial caries
Intermediate caries
Deep caries
Deep caries
Deep caries with pulpa penetration
Reactive changes
Reactive changes in pulpa
Reactive changes in pulpa
Acute and chronic appical pulpitis
Chron sup pulpitis appicalis
GINGIVITIS
Gingiva is the designation of the
squamous mucosa in between the teeth
and around them.
Gingivitis is inflammation of the mucosa
and the associated soft tissues.
Typically, the development of gingivitis is
the result of a lack of proper oral hygiene,
leading to an accumulation of dental
plaque and calculus.
Epidemiology of Gingivites
Gingivitis occurs at any age but is most
prevalent and severe in adolescence
(ranging from 40% to 60%), after which
the incidence tapers off. It is a reversible
disease;
Dental plaque
Dental plaque is a sticky, usually colorless, biofi lm
that builds in between and on the surface of the teeth.
It is formed by a complex of the oral bacteria, proteins
from the saliva, and desquamated epithelial cells. If
plaque continues to build andis not removed, it becomes
mineralized to form calculus (tartar).
The bacteria in the plaque release acids from
sugarrich foods, which erode the enamel surface of the
tooth.
Repeated erosions lead to dental caries. Plaque
build-up beneath the gumline can cause gingivitis.
Chronic gingivitis
Chronic gingivitis is characterized by
gingival
erythema,
edema,
bleeding,
Changes in contour,
loss of soft-tissue adaptation to the teeth.
Therapy of Gingivites
Therapy is primarily aimed at reducing the
accumulation of plaque andcalculus via
brushing, fl ossing, and regular dental visit
PERIODONTITIS
Periodontitis refers to an inflammatory process that
affects the supporting structures of the teeth:
periodontal ligaments,
alveolar bone,
cementum.
With progression, periodontitis can lead to serious
sequelae, including the loss of attachment caused by
complete destruction of the periodontal ligament and
alveolar bone.
Loosening and eventual loss of teeth are possible.
Pathogenesis of Periodontitis
Until the 1960s it was believed that longstanding
gingivitis uniformly progressed to periodontal
disease. However, this is no longer thought to be the case.
Development of periodontal disease is now considered
to be an independent process, which, for reasons that
are still unclear, is associated with a marked shift in the
types and proportions of bacteria along the gingiva. This
shift, along with other environmental conditions such as
poor oral hygiene, is believed to be important in the
pathogenesis of periodontitis.
Periodontal and systemic diseases
Periodontal disease can also be a component of several different
systemic diseases, including acquired immunodefi ciency
syndrome (AIDS), leukemia, Crohns disease, diabetes mellitus,
Down syndrome, sarcoidosis, and syndromes associated
with polymorphonuclear defects (Chdiak-Higashi syndrome,
agranulocytosis, and cyclic neutropenia).
Periodontal infections can also be etiologic factors in several
important systemic diseases. These include, for example, infective
endocarditis, pulmonary and brain abscesses, and adverse
pregnancy outcomes.
You might also like
- Powerpoint: Disorders of The EsophagusDocument65 pagesPowerpoint: Disorders of The Esophagusj.doe.hex_8782% (11)
- Undergraduate Medicine Study Notes PDFDocument764 pagesUndergraduate Medicine Study Notes PDFSHAKEEL1991No ratings yet
- Archaeology - October 2016 PDFDocument72 pagesArchaeology - October 2016 PDFOmer CetinkayaNo ratings yet
- Dental CariesDocument25 pagesDental CariesFemi100% (1)
- Code of Ethics Definitions of EthicsDocument6 pagesCode of Ethics Definitions of EthicsRaman SamraoNo ratings yet
- OUTPUT SabellanoDocument18 pagesOUTPUT SabellanoNedeve OznedNo ratings yet
- M.SC - Nursing 2019 20 Final PDFDocument55 pagesM.SC - Nursing 2019 20 Final PDFKinjalNo ratings yet
- Cervical Cancer OverviewDocument22 pagesCervical Cancer OverviewnyseaNo ratings yet
- Anatomy of Oral Cavity and Common DisordersDocument24 pagesAnatomy of Oral Cavity and Common DisordersMuhammad SalmanNo ratings yet
- Alcoholic Liver DiseaseDocument21 pagesAlcoholic Liver DiseaseInsta GrammerNo ratings yet
- Renal Cell CarcinomaDocument10 pagesRenal Cell Carcinoma'asyura Mohd RezaNo ratings yet
- Practical DieteticsDocument30 pagesPractical DieteticsRohit SharmaNo ratings yet
- Mysthenia THEIORY APPLICATIONDocument35 pagesMysthenia THEIORY APPLICATIONPatel Himani100% (1)
- Oral Manifestations of Nutritional Deficiency in Children PedoDocument29 pagesOral Manifestations of Nutritional Deficiency in Children PedoFourthMolar.com100% (1)
- Small Pox (CHN)Document13 pagesSmall Pox (CHN)Getom NgukirNo ratings yet
- Futuristic NursingDocument14 pagesFuturistic NursingPooja JanghelNo ratings yet
- Fractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaDocument50 pagesFractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaJustin Ahorro-DionisioNo ratings yet
- Mechanism of Respiration 2018Document48 pagesMechanism of Respiration 2018MomentaNo ratings yet
- Lesson Plan On FractureDocument27 pagesLesson Plan On FractureVaishali Singh100% (1)
- TRACHEOSTOMY CARE (Repaired) (Repaired)Document18 pagesTRACHEOSTOMY CARE (Repaired) (Repaired)DhAiRyA ArOrANo ratings yet
- Cushing's SyndromeDocument68 pagesCushing's SyndromeKaye De Guzman, BSN - Level 3ANo ratings yet
- Nursing and End-of-Life CareDocument26 pagesNursing and End-of-Life CareShafiq Ur RahmanNo ratings yet
- Types of FractureDocument45 pagesTypes of Fractureanupama varghese100% (1)
- Oral Complications FromDocument104 pagesOral Complications FromNndaydnaNo ratings yet
- World Patient Safety DayDocument17 pagesWorld Patient Safety DayNam PHẠM THÀNHNo ratings yet
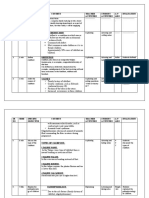
- TI M E Contrib Utory Objecti VE Content Teaching Learning Activity A.V.Aids Evalua-TionDocument11 pagesTI M E Contrib Utory Objecti VE Content Teaching Learning Activity A.V.Aids Evalua-TionBinal JoshiNo ratings yet
- Disorder of Oral CavityDocument4 pagesDisorder of Oral CavitySiva0726No ratings yet
- Brief History of The DiseaseDocument17 pagesBrief History of The DiseaseJon Corpuz AggasidNo ratings yet
- Esophageal CancerDocument25 pagesEsophageal CancerK poojithaNo ratings yet
- Diagnosis and Management of Oral MucositisDocument20 pagesDiagnosis and Management of Oral MucositisAlfyGototronNo ratings yet
- CSOM TreatmentDocument21 pagesCSOM TreatmentSarwinder SinghNo ratings yet
- MSC - Medical Surgical Sub Specialty Orthopedic Nursing PDFDocument42 pagesMSC - Medical Surgical Sub Specialty Orthopedic Nursing PDFBlessy SekarNo ratings yet
- Theories of Human Development: General Psychology Handouts 1 Sem AY 17-18Document8 pagesTheories of Human Development: General Psychology Handouts 1 Sem AY 17-18MariaMirandaJrNo ratings yet
- Worm Infestation in ChildrenDocument4 pagesWorm Infestation in ChildrenOleOhhNo ratings yet
- NCP On AppendicitisDocument7 pagesNCP On Appendicitisshweta singhNo ratings yet
- SR NO Time Specific Objective Content Teacher Activities Student Activities A.V Aids EvaluationDocument16 pagesSR NO Time Specific Objective Content Teacher Activities Student Activities A.V Aids EvaluationJuhi Johnson JadhavNo ratings yet
- Care Plan Pneumonia CompressDocument18 pagesCare Plan Pneumonia CompressAahad AmeenNo ratings yet
- Jabalpur (M.P.) : Subject - Management Nursing Assignment ONDocument9 pagesJabalpur (M.P.) : Subject - Management Nursing Assignment ONNikkiNo ratings yet
- Seminar ON HepatitisDocument41 pagesSeminar ON HepatitissomivipinNo ratings yet
- Ovarian DisordersDocument5 pagesOvarian DisordersNada MuchNo ratings yet
- Chronic Kidney Disease OverviewDocument15 pagesChronic Kidney Disease Overviewjames100% (1)
- Gastritis. Ulcer DiseaseDocument60 pagesGastritis. Ulcer DiseaseShambhu AshokNo ratings yet
- Shift Work Disorder and Associated Health Problems Among Nursing Staffs Working in A Tertiary Health Centre, Chennai, South IndiaDocument4 pagesShift Work Disorder and Associated Health Problems Among Nursing Staffs Working in A Tertiary Health Centre, Chennai, South IndiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Case Study 2Document37 pagesCase Study 2api-391842100No ratings yet
- Early Childhood Caries - A Review PDFDocument7 pagesEarly Childhood Caries - A Review PDFdr parveen bathlaNo ratings yet
- PneumoniaDocument12 pagesPneumoniaRola Miranda Guiang-ManaliliNo ratings yet
- Acute Pancreatitis - WikipediaDocument14 pagesAcute Pancreatitis - WikipediaSambamurthi Punninnair NarayanNo ratings yet
- Time Specific Objective Content Teaching Learning Activities Evaluati ONDocument20 pagesTime Specific Objective Content Teaching Learning Activities Evaluati ONAnnette BainesNo ratings yet
- MSC Nursing Dissertation Synopsis: Era University LucknowDocument19 pagesMSC Nursing Dissertation Synopsis: Era University LucknowNazia GulzarNo ratings yet
- Dog BiteDocument17 pagesDog BiteSanjeev BhatiaNo ratings yet
- Renal Cell CarcinomaDocument1 pageRenal Cell CarcinomaBobet ReñaNo ratings yet
- Ms. Meghana Goswami 1 Year M.SC M.B.N.CDocument12 pagesMs. Meghana Goswami 1 Year M.SC M.B.N.CmeghanaNo ratings yet
- Ethical Issues in NeonateDocument11 pagesEthical Issues in Neonatethilaga880% (1)
- Case Presentation - GASTRODocument46 pagesCase Presentation - GASTROalidudeNo ratings yet
- Bone Tumor: A. Nithya 1 Year M.SC (Nursing)Document46 pagesBone Tumor: A. Nithya 1 Year M.SC (Nursing)nithya nithyaNo ratings yet
- Cleft Lip Palate 9801Document27 pagesCleft Lip Palate 9801Achmad HariyantoNo ratings yet
- Diseases of ParadontDocument71 pagesDiseases of ParadontIsak ShatikaNo ratings yet
- Lec2/ Epidemiology of Dental CariesDocument7 pagesLec2/ Epidemiology of Dental Cariesمحمد العراقيNo ratings yet
- Lec2/ Epidemiology of Dental CariesDocument7 pagesLec2/ Epidemiology of Dental Cariesمحمد العراقيNo ratings yet
- Etiology of Periodontal Diseases: Dental Plaque (Microorganisms)Document9 pagesEtiology of Periodontal Diseases: Dental Plaque (Microorganisms)محمد محمود القحيفNo ratings yet
- What Is Dental PlaqueDocument9 pagesWhat Is Dental PlaqueHesham100% (1)
- Prevetion of Dental CariesDocument76 pagesPrevetion of Dental CariesmithunjithNo ratings yet
- Test - 18 Specific Diseases - Actinomycosis, TB, Syphilis, HIVDocument4 pagesTest - 18 Specific Diseases - Actinomycosis, TB, Syphilis, HIVIsak ShatikaNo ratings yet
- Test - 20 Dental ImplantsDocument5 pagesTest - 20 Dental ImplantsIsak ShatikaNo ratings yet
- CV Example - 2019 Issak1Document3 pagesCV Example - 2019 Issak1Isak ShatikaNo ratings yet
- Test - 14 Diseases of The TMJ PDFDocument4 pagesTest - 14 Diseases of The TMJ PDFIsak ShatikaNo ratings yet
- Test - 18 Specific Diseases - Actinomycosis, TB, Syphilis, HIVDocument4 pagesTest - 18 Specific Diseases - Actinomycosis, TB, Syphilis, HIVIsak ShatikaNo ratings yet
- Test - 8 Retension, Dystopia, PericoronitisDocument5 pagesTest - 8 Retension, Dystopia, PericoronitisIsak ShatikaNo ratings yet
- Test - 4 Intensive Therapy of Somatic Complicaton. Cardio Pulmonary Resuscitation (CPR)Document6 pagesTest - 4 Intensive Therapy of Somatic Complicaton. Cardio Pulmonary Resuscitation (CPR)Isak ShatikaNo ratings yet
- Schedule Classes 4th Years Ist SemesterDocument1 pageSchedule Classes 4th Years Ist SemesterIsak ShatikaNo ratings yet
- Test - 12 Odontogenic Maxillary SinusitisDocument5 pagesTest - 12 Odontogenic Maxillary SinusitisIsak ShatikaNo ratings yet
- Test - 10 Root (Radicular) CystsDocument5 pagesTest - 10 Root (Radicular) CystsIsak ShatikaNo ratings yet
- Test - 9 Chronic PeriodontitisDocument5 pagesTest - 9 Chronic PeriodontitisIsak ShatikaNo ratings yet
- Test - 13 Odontogenic Osteomyelitis of The Jaws, Furuncles, Carbuncles, ErysipelasDocument5 pagesTest - 13 Odontogenic Osteomyelitis of The Jaws, Furuncles, Carbuncles, ErysipelasIsak ShatikaNo ratings yet
- Schedule Classes 5th Years 1st SemesterDocument1 pageSchedule Classes 5th Years 1st SemesterIsak ShatikaNo ratings yet
- Test - 6 Methods of Extractions (Tooth Removal)Document4 pagesTest - 6 Methods of Extractions (Tooth Removal)Isak ShatikaNo ratings yet
- Schedule Four Years First SemesterDocument1 pageSchedule Four Years First SemesterIsak ShatikaNo ratings yet
- Schedule Fifth Year 1st SemesterDocument1 pageSchedule Fifth Year 1st SemesterIsak ShatikaNo ratings yet
- Viral Hepatitis (Part II)Document10 pagesViral Hepatitis (Part II)Isak ShatikaNo ratings yet
- Lecture: Erysipelas: Basic Clinical PrinciplesDocument15 pagesLecture: Erysipelas: Basic Clinical PrinciplesIsak ShatikaNo ratings yet
- Salmon Ellos IsDocument5 pagesSalmon Ellos IsIsak ShatikaNo ratings yet
- Short Table of Infectious DiseasesDocument9 pagesShort Table of Infectious DiseasesIsak ShatikaNo ratings yet
- TularemiaDocument5 pagesTularemiaIsak ShatikaNo ratings yet
- Yersiniosis: Yersinia Pathogenic Kinds and VariantsDocument7 pagesYersiniosis: Yersinia Pathogenic Kinds and VariantsIsak ShatikaNo ratings yet
- Infectious Disease Assignment 2018Document3 pagesInfectious Disease Assignment 2018Isak ShatikaNo ratings yet
- Chapter 3. Clinical Forms of Tuberculosis: Tuberculosis Course For English-Speaking StudentsDocument20 pagesChapter 3. Clinical Forms of Tuberculosis: Tuberculosis Course For English-Speaking StudentsIsak ShatikaNo ratings yet
- Cases InfectiousDocument20 pagesCases InfectiousIsak ShatikaNo ratings yet
- Yersiniosis: Yersinia Pathogenic Kinds and VariantsDocument7 pagesYersiniosis: Yersinia Pathogenic Kinds and VariantsIsak ShatikaNo ratings yet
- Food Poisoning: Major Infectious Causes of Acute DiarrheaDocument7 pagesFood Poisoning: Major Infectious Causes of Acute DiarrheaIsak ShatikaNo ratings yet
- Cases InfectiousDocument20 pagesCases InfectiousIsak ShatikaNo ratings yet
- 03 2 2 0 Primary Complex Eng 2014Document11 pages03 2 2 0 Primary Complex Eng 2014Isak ShatikaNo ratings yet
- What Is E-CollaborationDocument7 pagesWhat Is E-CollaborationToumba LimbreNo ratings yet
- Impact of Technology On Our LivesDocument3 pagesImpact of Technology On Our LivesKim ErandioNo ratings yet
- B - ELSB - Cat - 2020 PDFDocument850 pagesB - ELSB - Cat - 2020 PDFanupamNo ratings yet
- Listening 3b Skills Test 1aDocument3 pagesListening 3b Skills Test 1aPticaSelicaNo ratings yet
- Pset 2Document13 pagesPset 2rishiko aquinoNo ratings yet
- Term Paper - 2022964Document17 pagesTerm Paper - 2022964Md. Ahbab HasanNo ratings yet
- Markov Decision Processes For Path Planning in Unpredictable EnvironmentDocument8 pagesMarkov Decision Processes For Path Planning in Unpredictable EnvironmentVartolomeiDumitruNo ratings yet
- Reading The Bible From Feminist, Dalit, Tribal and Adivasi Perspectives (Course Code: BC 107)Document8 pagesReading The Bible From Feminist, Dalit, Tribal and Adivasi Perspectives (Course Code: BC 107)Arun Stanley100% (2)
- SFC PresentationDocument51 pagesSFC PresentationjmtriggerzNo ratings yet
- Optimizing Patient Flow: Innovation Series 2003Document16 pagesOptimizing Patient Flow: Innovation Series 2003Jeff SavageNo ratings yet
- LoperAmid 1Document5 pagesLoperAmid 1Hemma KusumaningrumNo ratings yet
- LADA Niva 1600rebuild1Document39 pagesLADA Niva 1600rebuild1Douglas Antonio Paredes MarquinaNo ratings yet
- A Child With Fever and Hemorrhagic RashDocument3 pagesA Child With Fever and Hemorrhagic RashCynthia GNo ratings yet
- Vertical Transportation: Commercial, Hotel, Hospital, Etc)Document5 pagesVertical Transportation: Commercial, Hotel, Hospital, Etc)fdarchitectNo ratings yet
- Neonatal Resuscitation ProgramDocument6 pagesNeonatal Resuscitation ProgramRick Frea100% (5)
- Historic Trial of Ali Brothers and Shankaracharya-1921Document276 pagesHistoric Trial of Ali Brothers and Shankaracharya-1921Sampath Bulusu100% (3)
- Student Exploration: Magnetism (Find Gizmo Icon On Eclass)Document4 pagesStudent Exploration: Magnetism (Find Gizmo Icon On Eclass)Abdel Majeed Tuffaha0% (1)
- Liebherr PR 712 Litronic Final DrivesDocument8 pagesLiebherr PR 712 Litronic Final DrivesLiebherr75% (4)
- High Performance ComputingDocument294 pagesHigh Performance Computingsorinbazavan100% (1)
- Project Report - Performance Anaylysis of Mutual Funds in IndiaDocument52 pagesProject Report - Performance Anaylysis of Mutual Funds in Indiapankaj100% (1)
- Australia Harvesting Rainwater For Environment, Conservation & Education: Some Australian Case Studies - University of TechnologyDocument8 pagesAustralia Harvesting Rainwater For Environment, Conservation & Education: Some Australian Case Studies - University of TechnologyFree Rain Garden ManualsNo ratings yet
- FPA 03-A.01 Permohonan Akreditasi LP LK LI LM PUP PBADocument595 pagesFPA 03-A.01 Permohonan Akreditasi LP LK LI LM PUP PBAabimanyubawonoNo ratings yet
- Preliminary Exam (Primark)Document4 pagesPreliminary Exam (Primark)Zybel RosalesNo ratings yet
- ErtlDocument64 pagesErtlManpreet SinghNo ratings yet
- 5 Waves AnswersDocument2 pages5 Waves AnswersNoor Ulain NabeelaNo ratings yet
- Effect of Social Economic Factors On Profitability of Soya Bean in RwandaDocument7 pagesEffect of Social Economic Factors On Profitability of Soya Bean in RwandaMarjery Fiona ReyesNo ratings yet
- FPI - Study Permit Application GuideDocument9 pagesFPI - Study Permit Application GuideKian Mark DarioNo ratings yet
- Elaborare Modele de Rating in Conformitate Cu IFRS 9Document8 pagesElaborare Modele de Rating in Conformitate Cu IFRS 9MstefNo ratings yet
- Central Venous PressureDocument3 pagesCentral Venous PressureHuy NguyễnNo ratings yet