Professional Documents
Culture Documents
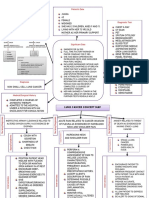
Cor Pulmonale
Uploaded by
Haya0 ratings0% found this document useful (0 votes)
100 views13 pagesCor pulmonale is pulmonary heart disease caused by dilation and hypertrophy of the right ventricle in response to lung or pulmonary vascular diseases. It develops due to chronic pulmonary hypertension and causes worsening prognosis. Acute cor pulmonale occurs rapidly from severe stimuli like pulmonary embolism, while chronic cor pulmonale progresses more slowly. Signs include elevated jugular pressure, edema and cyanosis late. Treatment targets the underlying lung or pulmonary disease to reduce pressure on the right ventricle.
Original Description:
CARDIO
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCor pulmonale is pulmonary heart disease caused by dilation and hypertrophy of the right ventricle in response to lung or pulmonary vascular diseases. It develops due to chronic pulmonary hypertension and causes worsening prognosis. Acute cor pulmonale occurs rapidly from severe stimuli like pulmonary embolism, while chronic cor pulmonale progresses more slowly. Signs include elevated jugular pressure, edema and cyanosis late. Treatment targets the underlying lung or pulmonary disease to reduce pressure on the right ventricle.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
100 views13 pagesCor Pulmonale
Uploaded by
HayaCor pulmonale is pulmonary heart disease caused by dilation and hypertrophy of the right ventricle in response to lung or pulmonary vascular diseases. It develops due to chronic pulmonary hypertension and causes worsening prognosis. Acute cor pulmonale occurs rapidly from severe stimuli like pulmonary embolism, while chronic cor pulmonale progresses more slowly. Signs include elevated jugular pressure, edema and cyanosis late. Treatment targets the underlying lung or pulmonary disease to reduce pressure on the right ventricle.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 13
Cor Pulmonale
Definition
• Cor Pulmonale
– pulmonary heart disease
– dilation and hypertrophy of the right ventricle (RV)
in response to diseases of the pulmonary
vasculature and/or lung parenchyma.
– excluded congenital heart disease and those
diseases in which the right heart fails secondary to
dysfunction of the left side of the heart
Etiology and Epidemiology
• develops in response to acute or chronic
changes in the pulmonary vasculature
• Changes that are sufficient to cause
pulmonary hypertension
• Once patients with chronic pulmonary or
pulmonary vascular disease develop cor
pulmonale, their prognosis worsens
Pathophysiology
• pulmonary hypertension that is sufficient to
lead to RV dilation, with or without the
development of concomitant RV hypertrophy
• Right ventricle: thin walled, compliant
– Better suited for high volumes than high pressure
• Sustained pressure overload (pulm HPN) and
increased vascular resistance causes RV to fail
Pathophysiology
• Acute Cor Pulmonale
– occurs after a sudden and severe stimulus with RV
dilatation and failure but no RV hypertrophy
• e.g massive pulmonary embolus
• Chronic Cor pulmonale
– more slowly evolving and slowly progressive
pulmonary hypertension that leads to RV dilation
and hypertrophy
Factors that determine severity
• hypoxia secondary to alterations in gas
exchange
• Hypercapnia
• Acidosis
• alterations in RV volume overload that are
affected by:
• exercise, heart rate, polycythemia, or increased salt and
retention because of a fall in cardiac output
Clinical presentation
• Symptoms:
– Dyspnea, the most common symptom
– usually the result of the increased work of breathing
secondary to changes in elastic recoil of the lung (fibrosing
lung diseases) or altered respiratory mechanics
– Orthopnea and paroxysmal nocturnal dyspnea are
rarely symptoms of isolated right HF
– reflect the increased work of breathing in the supine position
that results from compromised excursion of the diaphragm
Clinical presentation
• Symptoms:
– Tussive or effort-related syncope
– because of the inability of the RV to deliver blood adequately
to the left side of the heart
– Abdominal pain and ascites
– Due to right heart failure
– Lower extremity edema
– secondary to neurohormonal activation, elevated RV filling
pressures, or increased levels of carbon dioxide and hypoxia,
Clinical presentation
• Signs
– tachypnea
– elevated jugular venous pressures
– hepatomegaly
– lower-extremity edema
– Cyanosis is a late finding
Diagnosis
• ECG
– P pulmonale, right axis deviation, and RV
hypertrophy
• Chest X Ray
– enlargement of the main pulmonary artery, hilar
vessels, and the descending right pulmonary
artery
• Spiral CT
– acute thromboembolic disease
Diagnosis
• 2D echo
– measuring RV thickness and chamber dimensions
• Doppler echocardiography
– assess pulmonary artery pressures
• MRI
– assessing RV structure and function, particularly in
patients who are difficult to image with 2-D
echocardiography because of severe lung disease
Treatment
• Primary goal: target the underlying pulmonary
disease
• decrease in pulmonary vascular resistance and relieve the
pressure overload on the RV
• General principles:
• decreasing the work of breathing using noninvasive
mechanical ventilation, bronchodilation, and steroids
• treating any underlying infection
– Adequate oxygenation (oxygen saturation 90–92%)
will also decrease pulmonary vascular resistance and
reduce the demands on the RV
– Diuretics
You might also like
- Cor Pulmonale Definition, Causes, Symptoms and TreatmentDocument13 pagesCor Pulmonale Definition, Causes, Symptoms and TreatmentRizki JaneldiNo ratings yet
- Cor Pulmonale: Dr. Gerrard UyDocument13 pagesCor Pulmonale: Dr. Gerrard UymuthiaraNo ratings yet
- Cor Pulmonale: Dr. Gerrard UyDocument13 pagesCor Pulmonale: Dr. Gerrard Uyfaridah azzah sariNo ratings yet
- Kuliah 16 Cor PulmonaleDocument41 pagesKuliah 16 Cor PulmonalecaturwiraNo ratings yet
- Manage and Diagnose Acute and Chronic Cor PulmonaleDocument42 pagesManage and Diagnose Acute and Chronic Cor PulmonaleNym Angga SantosaNo ratings yet
- Pulmonary HypertensionDocument54 pagesPulmonary HypertensionmendaimashokombaNo ratings yet
- Pemicu 6 Eko Blok KGDDocument128 pagesPemicu 6 Eko Blok KGDEko SiswantoNo ratings yet
- Pulmonary Hypertension: Saurabh Biswas PGT, Dept. of Chest Medicine, CNMCHDocument59 pagesPulmonary Hypertension: Saurabh Biswas PGT, Dept. of Chest Medicine, CNMCHbsaurabh20No ratings yet
- Heart Failure: Classification, Risk Factors and Clinical FeaturesDocument48 pagesHeart Failure: Classification, Risk Factors and Clinical FeaturesMaria Cristina Sierralta SimonNo ratings yet
- Cor PulmonaleDocument21 pagesCor Pulmonalemaibejose100% (1)
- KP 2.5.5.3 Cor PulmonaleDocument17 pagesKP 2.5.5.3 Cor Pulmonalenurul ramadhiniNo ratings yet
- 8) Chronic Cor PulmonaleDocument2 pages8) Chronic Cor PulmonaleAris PaparisNo ratings yet
- Pulmonary EmbolismDocument8 pagesPulmonary EmbolismspoilttbrattNo ratings yet
- Heart Failure: Classification, Risk Factors and Clinical FeaturesDocument28 pagesHeart Failure: Classification, Risk Factors and Clinical FeaturesfredyNo ratings yet
- Hypertensive Heart DiseaseDocument7 pagesHypertensive Heart DiseaseMirajwati AdikusumaNo ratings yet
- HEMODYNAMICSDocument28 pagesHEMODYNAMICSaries0411No ratings yet
- ModuleIV RespiratoryEmergencies CHF COPD AsthmaDocument96 pagesModuleIV RespiratoryEmergencies CHF COPD AsthmaSaiKiranNo ratings yet
- COR PULMONALE - MahasiswaDocument14 pagesCOR PULMONALE - MahasiswaGalih Maygananda PutraNo ratings yet
- Cor PulmonaleDocument19 pagesCor PulmonaleMartina RizkiNo ratings yet
- Congestive Heart Failure LathaDocument68 pagesCongestive Heart Failure LathaLatha GhanesanNo ratings yet
- Eisenmenger Syndrome: Clinical DefinitionDocument3 pagesEisenmenger Syndrome: Clinical Definition22194No ratings yet
- Pulmonary Edema: Prepared By: South West Education CommitteeDocument65 pagesPulmonary Edema: Prepared By: South West Education CommitteedanradulescuNo ratings yet
- Pulmonary HypertensionDocument36 pagesPulmonary HypertensionDiana_anca6100% (2)
- Cardiogenic Shock ManagementDocument66 pagesCardiogenic Shock ManagementdrkurniatiNo ratings yet
- Heart FailureDocument72 pagesHeart FailuremacNo ratings yet
- Cardiac Tamponade (Suryani)Document72 pagesCardiac Tamponade (Suryani)Hamdani UsmanNo ratings yet
- KOR PULMONAL Revisi Maret 2017 SGLDocument17 pagesKOR PULMONAL Revisi Maret 2017 SGLrumaisyah alkatiriNo ratings yet
- Pleno Minggu 3 Blok 3.2Document57 pagesPleno Minggu 3 Blok 3.2ima_nekonayagiNo ratings yet
- Cor Pulmonal and CHDDocument44 pagesCor Pulmonal and CHDamir iksanNo ratings yet
- Congestive Cardiac Failure GuideDocument61 pagesCongestive Cardiac Failure GuideYAMINIPRIYANNo ratings yet
- Zoom Final PA CathetherDocument45 pagesZoom Final PA Cathetherhasanafridi.mechNo ratings yet
- Evaluation and Management of Right-SidedDocument65 pagesEvaluation and Management of Right-SidedJevin JameriaNo ratings yet
- Pulmonary Emolism PresentationDocument17 pagesPulmonary Emolism PresentationKennedy Ng'andweNo ratings yet
- Cardiac Tamponade: Mrs. D.Melba Sahaya Sweety.D M.SC Nursing GimsarDocument23 pagesCardiac Tamponade: Mrs. D.Melba Sahaya Sweety.D M.SC Nursing GimsarD. Melba S.S ChinnaNo ratings yet
- Valvular Heart DiseaseDocument2 pagesValvular Heart DiseaseAnonymous TVk12eX4No ratings yet
- Cyanotic Heart DiseaseDocument47 pagesCyanotic Heart Disease87-Saranya MNo ratings yet
- New HematologyOncology FAE2016Document108 pagesNew HematologyOncology FAE2016omarNo ratings yet
- Cardio-Vascular Disease: Mitral Stenosis & Mitral RegurgitationDocument25 pagesCardio-Vascular Disease: Mitral Stenosis & Mitral Regurgitationyulia silviNo ratings yet
- Respiratory System Muamar Aldalaeen, RN, Mba, HCRM, Cic, Ipm, MSN, PHD - Haneen Alnuaimi, MSNDocument46 pagesRespiratory System Muamar Aldalaeen, RN, Mba, HCRM, Cic, Ipm, MSN, PHD - Haneen Alnuaimi, MSNAboodsha ShNo ratings yet
- Cardiac Catheterization Hemodynamic Monitoring GuideDocument38 pagesCardiac Catheterization Hemodynamic Monitoring GuideMoch Irvan BadriNo ratings yet
- Pulmonary Heart DiseasesDocument26 pagesPulmonary Heart DiseasesmalekNo ratings yet
- Pulmonary Ventilation/Perfusion Relationships & DiagnosticsDocument38 pagesPulmonary Ventilation/Perfusion Relationships & DiagnosticsAbdallah AlasalNo ratings yet
- Pulmonary Hypertension: Causes, Diagnosis, Treatment and ClassificationDocument58 pagesPulmonary Hypertension: Causes, Diagnosis, Treatment and ClassificationDevashish VermaNo ratings yet
- Cyanotic Heart LesionsDocument40 pagesCyanotic Heart LesionsRaison D'etreNo ratings yet
- Ratheesh R.LDocument23 pagesRatheesh R.LvaishnaviNo ratings yet
- Pulmonary EdemaDocument59 pagesPulmonary EdemamaibejoseNo ratings yet
- COPD and Pulmonary Hypertension Cause Right Heart FailureDocument19 pagesCOPD and Pulmonary Hypertension Cause Right Heart FailureIka Lukita SariNo ratings yet
- Pulmonary Hypertension: An Overview of Causes, Symptoms and DiagnosisDocument40 pagesPulmonary Hypertension: An Overview of Causes, Symptoms and DiagnosisAlexander Santiago ParelNo ratings yet
- Acute Respiratory FailureDocument51 pagesAcute Respiratory Failureigorhorenko15No ratings yet
- Presentation 3Document14 pagesPresentation 3mbbs03032022No ratings yet
- In The Name of God: Cardiogenic Pulmonary EdemaDocument51 pagesIn The Name of God: Cardiogenic Pulmonary EdemaaldiansyahraufNo ratings yet
- V. Complications of CVDDocument26 pagesV. Complications of CVDJan Federick BantayNo ratings yet
- Pulmonary Vascular Disorders and Respiratory FailureDocument5 pagesPulmonary Vascular Disorders and Respiratory FailureTrishia GuillermoNo ratings yet
- Cor Pulmonale: Right Heart Failure Due to Lung DiseaseDocument62 pagesCor Pulmonale: Right Heart Failure Due to Lung DiseaseAlbert NixonNo ratings yet
- 4th Problem KGD DanielDocument130 pages4th Problem KGD DanielSelly HerliaNo ratings yet
- Approach To The Patient With Shortness of Breath: Colin EdwardsDocument37 pagesApproach To The Patient With Shortness of Breath: Colin EdwardsNur FadzilahNo ratings yet
- Cyanotic Congenital Heart DiseaseDocument50 pagesCyanotic Congenital Heart DiseaseSasi KumarNo ratings yet
- Manage Acute Pulmonary Oedema in 38 CharactersDocument4 pagesManage Acute Pulmonary Oedema in 38 CharactersTze SiangNo ratings yet
- ECMO Cardiopulmonary Support in Critically Ill ChildrenDocument68 pagesECMO Cardiopulmonary Support in Critically Ill Childrenapi-3831614No ratings yet
- 281 481 1 SMDocument7 pages281 481 1 SMYuli MayasariNo ratings yet
- Cns Vascularization DR - Dianayu Hamama Pitra, SP.S, M.BiomedDocument43 pagesCns Vascularization DR - Dianayu Hamama Pitra, SP.S, M.BiomedHayaNo ratings yet
- ST Segment DepressiDocument16 pagesST Segment DepressiHayaNo ratings yet
- Drug Doses 2017Document127 pagesDrug Doses 2017Yuliawati HarunaNo ratings yet
- Parasit SkemaDocument12 pagesParasit SkemaFahlia Bena Pratama100% (1)
- Limping ChildDocument54 pagesLimping ChildHayaNo ratings yet
- Kelainan Kongenital Pada Tulang BelakangDocument16 pagesKelainan Kongenital Pada Tulang BelakangHayaNo ratings yet
- Neuro of Tal Molog IDocument42 pagesNeuro of Tal Molog IHayaNo ratings yet
- Kanker ServikDocument34 pagesKanker ServikRezky KotoNo ratings yet
- Diabetic Foot UlcerDocument33 pagesDiabetic Foot UlceragieajNo ratings yet
- Patogenesis ACSDocument124 pagesPatogenesis ACSHayaNo ratings yet
- Pathophysiology of HFDocument40 pagesPathophysiology of HFHayaNo ratings yet
- Digestion AnatomyDocument68 pagesDigestion Anatomysunil19854503No ratings yet
- Chest Injuries GuideDocument19 pagesChest Injuries GuideAbdi Kumala100% (1)
- Musculoskeletal tumor classification and treatmentDocument89 pagesMusculoskeletal tumor classification and treatmentHayaNo ratings yet
- Print Skill LabDocument1 pagePrint Skill LabHayaNo ratings yet
- Cryptorchidism Guide: Embryology, Causes, ClassificationDocument50 pagesCryptorchidism Guide: Embryology, Causes, ClassificationAlvin GfNo ratings yet
- Haya's English TaskDocument2 pagesHaya's English TaskHayaNo ratings yet
- Limping ChildDocument54 pagesLimping ChildHayaNo ratings yet
- Uro PrintDocument3 pagesUro PrintHayaNo ratings yet
- Colon 04Document28 pagesColon 04Yelsa NoritaNo ratings yet
- Dialogue SSDocument22 pagesDialogue SSHayaNo ratings yet
- SungsangDocument19 pagesSungsangHayaNo ratings yet
- English TaskDocument2 pagesEnglish TaskHayaNo ratings yet
- Print Skill LabDocument1 pagePrint Skill LabHayaNo ratings yet
- Sung SangDocument19 pagesSung SangHayaNo ratings yet
- Clinical Approach in NeuropathyDocument43 pagesClinical Approach in NeuropathyHayaNo ratings yet
- Dialogue SSDocument22 pagesDialogue SSHayaNo ratings yet
- Reaksi AnafilaksisDocument34 pagesReaksi AnafilaksisPutri Reno IntanNo ratings yet
- Inocencio School Student Health Declaration SheetDocument2 pagesInocencio School Student Health Declaration SheetCrunchy Fried RiceNo ratings yet
- Nursing Care Plan For Upper Resrpiratory Tract InfectionDocument2 pagesNursing Care Plan For Upper Resrpiratory Tract Infectionmariejo90% (30)
- Pneumothorax and lung lesions seen on chest X-raysDocument90 pagesPneumothorax and lung lesions seen on chest X-raysdsekulic_1100% (1)
- Kołtuniuk Et Al., 2017 PDFDocument11 pagesKołtuniuk Et Al., 2017 PDFDiba Eka DiputriNo ratings yet
- EMT NotesDocument58 pagesEMT NotesJosue PasillasNo ratings yet
- Lung Cancer Concept Map-Group 2Document2 pagesLung Cancer Concept Map-Group 2Maria Cristina100% (2)
- Clinical Practice Experience (CPE) Record 5 Phase 1Document11 pagesClinical Practice Experience (CPE) Record 5 Phase 1Sammy ChegeNo ratings yet
- Day 1. Mohd Sami 1Document67 pagesDay 1. Mohd Sami 1Baebee LouNo ratings yet
- Emergencies in Palliative CareDocument3 pagesEmergencies in Palliative CareJorge Cortina GonzalesNo ratings yet
- Penugasan B.ing (Ing)Document4 pagesPenugasan B.ing (Ing)ismail officialNo ratings yet
- Medical Surgical NursingDocument146 pagesMedical Surgical Nursingnisha jomonNo ratings yet
- Paed Osce ChecklistDocument40 pagesPaed Osce ChecklistLeCetraNo ratings yet
- ACUTE DECOMPENSATED HEART FAILUREDocument71 pagesACUTE DECOMPENSATED HEART FAILUREVivek Anandan100% (1)
- Devlin2020 PDFDocument8 pagesDevlin2020 PDFMatias FlammNo ratings yet
- Nursing considerations for clients on loop diuretics and beta blockersDocument59 pagesNursing considerations for clients on loop diuretics and beta blockersGil Raphael GanibanNo ratings yet
- TCAA's Safe Return-To-School Health PlanDocument12 pagesTCAA's Safe Return-To-School Health PlanGarfield The greatNo ratings yet
- Care of Patients With Noninfectious Lower Respiratory ProblemsDocument46 pagesCare of Patients With Noninfectious Lower Respiratory Problemsjrflores1284No ratings yet
- Respiratory System: Assessment: ObjectivesDocument19 pagesRespiratory System: Assessment: ObjectivesNURSES- NOOK & CORNERNo ratings yet
- Case # 4 Difficulty of BreathingDocument6 pagesCase # 4 Difficulty of BreathingGrace TanajuraNo ratings yet
- LP2 MAJOR EXAM 4 Files Merged 2 Files MergedDocument285 pagesLP2 MAJOR EXAM 4 Files Merged 2 Files MergedBianca ArceNo ratings yet
- Byssinosis-Health Hazards From Cotton DustDocument32 pagesByssinosis-Health Hazards From Cotton DustRajesh Dwivedi100% (1)
- Pratice Questions For NCLEX PDFDocument413 pagesPratice Questions For NCLEX PDFEmily97% (29)
- Nur 101 Data Base 1Document23 pagesNur 101 Data Base 1api-337919180No ratings yet
- PressedDocument71 pagesPressedGabriela ChristianNo ratings yet
- Andrade, Ban, Salleva - Liver Cirrhosis - Objectives, Manifestations, Drug StudyDocument9 pagesAndrade, Ban, Salleva - Liver Cirrhosis - Objectives, Manifestations, Drug StudyWindi Dawn SallevaNo ratings yet
- TB transmission, diagnosis, and treatmentDocument10 pagesTB transmission, diagnosis, and treatmentSahara Sahjz MacabangunNo ratings yet
- 1.5A Copd: OutlineDocument12 pages1.5A Copd: OutlineCecille Ann CayetanoNo ratings yet
- Assessment Planning Intervention Rationale Evaluation: Nursing DiagnosisDocument2 pagesAssessment Planning Intervention Rationale Evaluation: Nursing DiagnosisLovely CacapitNo ratings yet
- Professional Examination Board Group-2 Recruitment Test QuestionsDocument64 pagesProfessional Examination Board Group-2 Recruitment Test Questionsraghu051084No ratings yet
- COVID-19 Report on Virus Outbreak, Symptoms and TreatmentDocument16 pagesCOVID-19 Report on Virus Outbreak, Symptoms and TreatmentSara GuptaNo ratings yet