Professional Documents
Culture Documents
Chapter 016
Uploaded by
api-36973260 ratings0% found this document useful (0 votes)
34 views23 pagesCataracts, glaucoma, macular degeneration Age Family history Gender Ethnicity Smoking Alcohol Intake Medications Chronic diseases taking any medications? What? When did you start taking them? do you use eyedrops? for what reason? what kind of drops? how often? do you wear protective eyewear when playing sports? - Are there sparks or flying bits of metal that could injure eyes?
Original Description:
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCataracts, glaucoma, macular degeneration Age Family history Gender Ethnicity Smoking Alcohol Intake Medications Chronic diseases taking any medications? What? When did you start taking them? do you use eyedrops? for what reason? what kind of drops? how often? do you wear protective eyewear when playing sports? - Are there sparks or flying bits of metal that could injure eyes?
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
34 views23 pagesChapter 016
Uploaded by
api-3697326Cataracts, glaucoma, macular degeneration Age Family history Gender Ethnicity Smoking Alcohol Intake Medications Chronic diseases taking any medications? What? When did you start taking them? do you use eyedrops? for what reason? what kind of drops? how often? do you wear protective eyewear when playing sports? - Are there sparks or flying bits of metal that could injure eyes?
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 23
Eyes and Visual System
Chapter 16
Copyright © 2005, Mosby, Inc.All rights reserved
Health History: Risk Factors
Cataracts, glaucoma, macular degeneration
• Age
• Family history
• Gender
• Ethnicity
• Smoking
• Alcohol Intake
• Medications
• Chronic diseases
• Cataracts
• Glaucoma
• Macular degeneration
Copyright © 2005, Mosby, Inc.All rights reserved
General Health History
Present health status
• Have you noticed changes in vision?
• When was last eye examination? Outcome?
Have you been tested for glaucoma?
• Do you smoke? If yes, how much and for how
long?
• Do you drink alcohol? How much? How often?
• Chronic illnesses or conditions such as diabetes
mellitus or hypertension?
• Taking any medications? What? When did you
start taking them?
Copyright © 2005, Mosby, Inc.All rights reserved
General Health History
Present health status (cont.)
• Do you use eyedrops? For what reason? What kind
of drops? How often?
• Do you wear contact lenses or glasses?
– When were they prescribed? For what problem? Are
contact lenses soft, hard, or extended wear? Do you ever
sleep with contact lenses? How often do you clean
glasses? Contact lenses? How do you clean them?
Copyright © 2005, Mosby, Inc.All rights reserved
General Health History
Present health status (cont.)
• Do you wear sunglasses in sunlight?
• Do you wear protective eyewear when playing
sports?
• Does your job involve vision risks?
– Are there sparks or flying bits of metal that could
injure eyes? What actions do you take to protect
eyes? Safety goggles?
Copyright © 2005, Mosby, Inc.All rights reserved
General Health History
Past medical history
• Had any problems with eyes or vision?
– Past problems with eye, such as infections, may recur
and may help explain current visual problems
• Had any surgery on eyes? What procedure,
when, and what outcome? Had injury or trauma
to eyes?
– Incidence of injury or surgery may provide information
about eye or visual problems (eye surgery is a risk
factor for glaucoma)
Copyright © 2005, Mosby, Inc.All rights reserved
General Health History
Family history
• Does anyone in your family have cataracts?
• Glaucoma?
• Diabetes mellitus?
• Nearsightedness (myopia)?
• Farsightedness (hyperopia)?
All these conditions have familial tendencies,
and may affect vision. If there is a positive
answer to any of these conditions, the client’s
risk of developing them increases
Copyright © 2005, Mosby, Inc.All rights reserved
Problem-Based History
• Principal areas to be investigated are:
– Difficulty with vision
– Pain
– Erythema or edema (or both)
– Watering or discharge
As with symptoms in all areas of health
assessment, a symptom analysis is completed
that includes location, quality, quantity,
chronology, setting, associated manifestations,
alleviating factors, and aggravating factors
Copyright © 2005, Mosby, Inc.All rights reserved
Problem-Based History
• Difficulty with vision
– What type of difficulty are you having with vision?
When did it begin? Suddenly or gradually? Affect
one eye or both? Constant, or come and go?
Blurring? Cloudiness? Images out of focus?
Spots (floaters) in front of your eyes?
– See a halo or multicolored rings around objects
or lights?
– Noticed a “blind spot”? Does it move as you shift
gaze? Has peripheral vision decreased?
Copyright © 2005, Mosby, Inc.All rights reserved
Problem-Based History
• Difficulty with vision (cont.)
– Have vision problems interfered with daily life? Describe
how. Do you require books with large print, on audiotape,
or in Braille?
– See a curtain coming down across line of vision in one or
both eyes? Do you have difficulty seeing at night? Clients
with detached retina report curtain coming down over
affected eye
– Difficulty seeing at night? Night blindness can occur in
optic atrophy, glaucoma, or vitamin A deficiency
Copyright © 2005, Mosby, Inc.All rights reserved
Problem-Based History
• Eye pain
– Describe the pain. Is it sharp? Dull? Throbbing?
Burning? Itching? How intense is pain on a scale of 0 to
10?
– When did the eye pain start? Did it begin suddenly or
gradually? Where is it felt? Sudden onset may be from a
detached retina and requires immediate medical care
– What do you think is causing the pain? Do you feel that
there is something in your eye? Do you have a
headache?
– What makes the pain worse? What makes it better? How
have you treated it? How effective was the treatment?
Copyright © 2005, Mosby, Inc.All rights reserved
Examination: Overview
• Not all techniques are included with every examination;
you may perform some of these techniques only
occasionally
• Exam techniques depend on many variables, including
the reason for the exam, setting, condition and age of
client, skill level of nurse
• Specific findings detected during the examination may
warrant use of additional examination techniques
• It is the nurse’s decision to determine which techniques
are indicated for each examination
Copyright © 2005, Mosby, Inc.All rights reserved
Examination: Vision
• Test visual acuity (distant vision) using Snellen’s chart
• Test visual acuity (near vision)
– With age there is loss of lens elasticity; this is
presbyopia (the client must move the card farther
away to see it clearly)
• Assess visual fields for peripheral vision using the
confrontation test
• Inspect the extraocular muscles for movement
• Inspect the corneal light reflex for symmetry
(Hirschberg’s test)
Copyright © 2005, Mosby, Inc.All rights reserved
Examination: External Ocular
Structures
• Inspect eyebrows for hair distribution, underlying
skin, and symmetry
• Inspect eyelids and eyelashes for symmetry,
position, closure, blinking, discharge, and color
• Inspect and palpate globe in bony socket for
position and indentation
• Inspect lacrimal puncta for color, moisture,
discharge, tenderness, and nodules
• Inspect bulbar conjunctiva for color and clarity
Copyright © 2005, Mosby, Inc.All rights reserved
Examination: Globe of the Eye
• Inspect sclera for color and clarity; sclera should be
white and clear
• Inspect cornea for transparency and surface
characteristics
• Inspect iris for shape and color
• Inspect pupils for size, shape, reaction to light,
consensual reaction, and accommodation
Copyright © 2005, Mosby, Inc.All rights reserved
Age-Related Variations: Older Adults
• History
– Do you have any trouble with vision when climbing stairs
or driving? (older adults lose depth perception)
– Do you feel that you have lost any peripheral vision? Do
you have problems with night vision? Have you noticed a
change in recognizing colors?
– Do you have cataracts? Have you had cataracts
removed? Have cataracts progressed, causing
decreased vision?
– Do your eyes feel dry or burn? Do you have increased or
decreased tearing? What do you do for these problems?
(tears decrease in quantity, causing dry eyes, which can
be treated with artificial tears)
Copyright © 2005, Mosby, Inc.All rights reserved
Age-Related Variations:
Older Adults
• Examination: procedures and techniques
• Eye examination conducted the same as
for younger adults
Copyright © 2005, Mosby, Inc.All rights reserved
Age-Related Variations: Older Adults
• Normal and abnormal findings: normal findings expected of
an older adult may be difficult to distinguish from abnormal
findings
– Central and peripheral vision may decrease after age 70
– Acuity of 20/20 or 20/30 with corrective lenses is
common; accommodation takes longer
– Eyebrows may be thin along the outer edge and
remaining brow hair may appear coarse
– Actual ptosis may occur
– Orbital fat may have decreased, so eyes appear sunken,
or may herniate, causing bulging on lower lid or inner
third the upper lid
Copyright © 2005, Mosby, Inc.All rights reserved
Clients with Situational Variations
• Clients with decreased or absent vision
– When performing physical assessment on a blind
person, remember to alert client to all actions before
you perform them
– History questions revised to delete those relating to
vision and ocular problems. Questions about pain,
edema, watering, discharge still appropriate
– Additional questions needed concerning how
individual has adapted to loss of sight. Physical
examination includes only inspection of the external
eye structures as described for adult
Copyright © 2005, Mosby, Inc.All rights reserved
Clients with Situational Variations
• Clients with prosthetic eye
– Clients with enucleation of an eye replaced by
a prosthesis appear to have binocular vision
but have no sight on affected side and must
be approached from sighted side
– Some artificial eyes are permanently
implanted. Others are removed for daily
cleaning
Copyright © 2005, Mosby, Inc.All rights reserved
Common Problems and Conditions:
External Eye
• Hordeolum (sty): acute infection
originating in sebaceous gland of eyelid
• Conjunctivitis: inflammation of palpebral or
bulbar conjunctiva caused by local
infection of bacteria or virus, or by allergic
reaction, systemic infection, or chemical
irritation
Copyright © 2005, Mosby, Inc.All rights reserved
Common Problems and Conditions
Extraocular muscles: strabismus
• Abnormal ocular alignment in which the visual
axes do not meet at the desired point is termed
strabismus.
• Nonparalytic strabismus caused by muscle
weakness, focusing difficulties, unilateral refractive
error, or anatomic differences in eyes
• Paralytic strabismus is a motor imbalance caused
by paresis or paralysis of an extraocular muscle
Copyright © 2005, Mosby, Inc.All rights reserved
Common Problems and Conditions:
Internal Eye
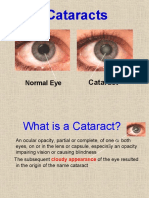
• Cataract: opacity of crystalline lens, commonly
occurs from denaturation of lens protein caused by
aging
– Cataracts caused by aging usually are central, but
peripheral cataracts are seen in hypoparathyroidism
– Congenital cataracts can result from maternal rubella or
other fetal insults during first trimester of pregnancy
– Trauma to eye can also cause cataracts
• Diabetic retinopathy: visual alteration caused by
diabetes mellitus; changes in retinal capillaries; is
leading cause of blindness from ages 20 to 75;
divided into background and proliferative
Copyright © 2005, Mosby, Inc.All rights reserved
You might also like
- Difference Between An Ophthalmologist, Optometrist and Optician PDFDocument2 pagesDifference Between An Ophthalmologist, Optometrist and Optician PDFSHASHANKNo ratings yet
- Ophthobook PDFDocument135 pagesOphthobook PDFl33t54r62No ratings yet
- O&M Manual For Vms PumpDocument11 pagesO&M Manual For Vms PumpKaushik ChakrabortyNo ratings yet
- I. Leadership/ Potential and Accomplishments Criteria A. InnovationsDocument5 pagesI. Leadership/ Potential and Accomplishments Criteria A. InnovationsDEXTER LLOYD CATIAG100% (1)
- PM PillarDocument56 pagesPM PillarNavneet Sharma75% (4)
- Blackboard1 150313105122 Conversion Gate01Document45 pagesBlackboard1 150313105122 Conversion Gate01jessajoy deslateNo ratings yet
- Cataract FinalDocument14 pagesCataract FinalSubha MaheswariNo ratings yet
- Chapter 015Document21 pagesChapter 015api-3697326No ratings yet
- Cataract SenilisDocument54 pagesCataract Senilismayo djitroNo ratings yet
- Aetcom QuesDocument11 pagesAetcom QuesDiyNo ratings yet
- Sensation: Hearing, Vision, Taste, Touch, and SmellDocument99 pagesSensation: Hearing, Vision, Taste, Touch, and SmellMichelle LindsayNo ratings yet
- Strabismus: By: Audra Bishop Beth Moline Elisabeth CohenDocument60 pagesStrabismus: By: Audra Bishop Beth Moline Elisabeth CohenmalathiNo ratings yet
- MYOPIADocument21 pagesMYOPIARimi Sree DasNo ratings yet
- Cataract InformationDocument25 pagesCataract Informationvasanth_1515No ratings yet
- Chapter 025Document34 pagesChapter 025api-3697326No ratings yet
- Children's Eyes and Vision Children's Eyes and Vision: Presented by Dr. (Name Here)Document33 pagesChildren's Eyes and Vision Children's Eyes and Vision: Presented by Dr. (Name Here)Wagner de AvizNo ratings yet
- 3 - Assessing EyeDocument13 pages3 - Assessing EyeFrancine Julia MorilloNo ratings yet
- Op Thom OlogyDocument88 pagesOp Thom OlogyFareed KhanNo ratings yet
- Do You Think You Need An Eye Test?Document2 pagesDo You Think You Need An Eye Test?Lyka Antonette YuNo ratings yet
- Difference Between An Ophthalmologist, Optometrist and Optician PDFDocument2 pagesDifference Between An Ophthalmologist, Optometrist and Optician PDFRoll KingsNo ratings yet
- Difference Between An Ophthalmologist, Optometrist and OpticianDocument2 pagesDifference Between An Ophthalmologist, Optometrist and OpticianMuhammad NaveedNo ratings yet
- Ophthalmologist, Optometrist and Optician111123 PDFDocument2 pagesOphthalmologist, Optometrist and Optician111123 PDFLay EcanNo ratings yet
- Difference Between An Ophthalmologist, Optometrist and Optician PDFDocument2 pagesDifference Between An Ophthalmologist, Optometrist and Optician PDFSHASHANKNo ratings yet
- Differences Between Ophthalmologist, and OpticianDocument2 pagesDifferences Between Ophthalmologist, and OpticianLay EcanNo ratings yet
- AMETROPIADocument48 pagesAMETROPIARahul KirkNo ratings yet
- University of Gondar: AmblyopiaDocument36 pagesUniversity of Gondar: Amblyopiaendalew mulugetaNo ratings yet
- Chapter 11 Eye & Vision DisordersDocument72 pagesChapter 11 Eye & Vision DisordersMYLENE GRACE ELARCOSANo ratings yet
- Eye Myths FactsDocument29 pagesEye Myths FactsZaire VillaNo ratings yet
- Triage MataDocument33 pagesTriage MataastroirmaNo ratings yet
- Your EyesDocument71 pagesYour EyessdgouseNo ratings yet
- Eye Care Optometrists PDFDocument2 pagesEye Care Optometrists PDFkapczukNo ratings yet
- 1.3 Examination of The Anterior SegmentDocument95 pages1.3 Examination of The Anterior SegmentMiguel Angel Palacios BlazquezNo ratings yet
- VI Psa Pres Common Eye Conditions2Document58 pagesVI Psa Pres Common Eye Conditions2PopeyeNo ratings yet
- Strabismus 10Document25 pagesStrabismus 10william williamNo ratings yet
- Strabismus: By: Audra Bishop Beth Moline Elisabeth CohenDocument25 pagesStrabismus: By: Audra Bishop Beth Moline Elisabeth CohenNisaNo ratings yet
- Advance Trends in Eye Care: DR Divya Kesarwani Consultant Cataract and Glaucoma ServicesDocument42 pagesAdvance Trends in Eye Care: DR Divya Kesarwani Consultant Cataract and Glaucoma ServicesdrdivyakesarwaniNo ratings yet
- Ears, Eyes, Nose & ThroatDocument132 pagesEars, Eyes, Nose & ThroatMarnelli_Iris__4261No ratings yet
- Vi Psa Pres Common Eye Conditions Aug10 3.08.29 PMDocument58 pagesVi Psa Pres Common Eye Conditions Aug10 3.08.29 PMSarthak KabiNo ratings yet
- Congenital Strabismus: S. Vanitha, B.optom, 3 YearDocument23 pagesCongenital Strabismus: S. Vanitha, B.optom, 3 YearDivya Priya Dharmalingam100% (1)
- StrabismusDocument30 pagesStrabismusEjay Jacob Ricamara100% (1)
- Visual ProblemsDocument151 pagesVisual Problemskatrina_rn09No ratings yet
- Eye Disorders: Structure of The EyeDocument13 pagesEye Disorders: Structure of The Eyeapi-3822433No ratings yet
- Eye HXDocument2 pagesEye HXAnishilNo ratings yet
- Cataract InformationDocument25 pagesCataract InformationDr.K.M. AbdullaNo ratings yet
- Pediatric Ocular EmergenciesDocument71 pagesPediatric Ocular EmergenciesenzomontresolNo ratings yet
- Health Assessment - EYES ReviewerDocument6 pagesHealth Assessment - EYES ReviewerAnna Juliana SitoNo ratings yet
- Patrick Duah - Vision Spring.Document8 pagesPatrick Duah - Vision Spring.harryNo ratings yet
- Congenital CataractsDocument123 pagesCongenital CataractsRizqy AbdullahNo ratings yet
- 5-History Taking and Examination Part 1Document42 pages5-History Taking and Examination Part 1AmrNo ratings yet
- 04 CataractsurgeryDocument16 pages04 Cataractsurgeryapi-3695929No ratings yet
- Cortical Visual Impairment and Blindness-PPT-HadleyDocument55 pagesCortical Visual Impairment and Blindness-PPT-HadleyIntanOktavianaAdiyanto100% (1)
- Eye Movement ProblemsDocument8 pagesEye Movement Problemsvenkat techNo ratings yet
- Ophthalmology Clerks: Alea, Denz Marc Custodio, Audreyfil Perez, Francis MiguelDocument14 pagesOphthalmology Clerks: Alea, Denz Marc Custodio, Audreyfil Perez, Francis MiguelDenz Marc AleaNo ratings yet
- Impaired Vision and BlindnessDocument44 pagesImpaired Vision and BlindnessYujenNo ratings yet
- Glaucoma New Zealand - A Charitable TrustDocument49 pagesGlaucoma New Zealand - A Charitable TrustMiazan SheikhNo ratings yet
- Dr. Ashraf Sayeed: Department of OphthalmologyDocument49 pagesDr. Ashraf Sayeed: Department of Ophthalmologysaiful haque100% (1)
- Glaucoma and CataractDocument30 pagesGlaucoma and CataractJayselle ArvieNo ratings yet
- CataractDocument5 pagesCataractAbhinandan SharmaNo ratings yet
- Thesis On Refractive ErrorsDocument7 pagesThesis On Refractive ErrorsLuz Martinez100% (2)
- Age-Related Macular Degeneration: by Lohit Valleru Course - Rehabilitation Engineering Professor - Joel MyklebustDocument34 pagesAge-Related Macular Degeneration: by Lohit Valleru Course - Rehabilitation Engineering Professor - Joel Myklebustlohitv9No ratings yet
- Glaukoma Dan KonjungtivitisDocument24 pagesGlaukoma Dan KonjungtivitisAnnisa DeasyNo ratings yet
- Osteoporosis Mary AignerDocument45 pagesOsteoporosis Mary Aignerapi-3697326No ratings yet
- Family Planning Presentation Kaylar GriffinDocument60 pagesFamily Planning Presentation Kaylar Griffinapi-3697326No ratings yet
- Mental Health and Mental IllnessDocument13 pagesMental Health and Mental Illnessapi-36973260% (1)
- Review For CBF Exam ONEDocument2 pagesReview For CBF Exam ONEapi-3697326No ratings yet
- StressDocument25 pagesStressapi-3697326No ratings yet
- Instructors's DP Spring 07Document1 pageInstructors's DP Spring 07api-3697326No ratings yet
- 9cc97fec Bbed 44bf b69c 5e52a52a9faeDocument49 pages9cc97fec Bbed 44bf b69c 5e52a52a9faeapi-3697326No ratings yet
- Learning GuideDocument42 pagesLearning Guideapi-3697326100% (1)
- Cha 0013Document25 pagesCha 0013api-3697326No ratings yet
- Cha 0011Document7 pagesCha 0011api-3697326No ratings yet
- Daily PlanDocument2 pagesDaily Planapi-3697326100% (1)
- Cha 0012Document6 pagesCha 0012api-3697326100% (1)
- Cha 0014Document9 pagesCha 0014api-3697326No ratings yet
- Cha 0009Document8 pagesCha 0009api-3697326No ratings yet
- RNSG 1331 Exam 2 Blueprint v2Document2 pagesRNSG 1331 Exam 2 Blueprint v2api-3697326No ratings yet
- Cha 0010Document12 pagesCha 0010api-3697326100% (1)
- Cha 0001Document7 pagesCha 0001api-3697326No ratings yet
- CH 09Document20 pagesCH 09api-3697326100% (1)
- Respiratory 4 Spring 07Document26 pagesRespiratory 4 Spring 07api-3697326No ratings yet
- Cha 0002Document13 pagesCha 0002api-3697326No ratings yet
- 9cc97fec Bbed 44bf b69c 5e52a52a9faeDocument49 pages9cc97fec Bbed 44bf b69c 5e52a52a9faeapi-3697326No ratings yet
- Peripheral Arterial Disease of The Lower ExtremitiesDocument25 pagesPeripheral Arterial Disease of The Lower Extremitiesapi-3697326100% (1)
- Anxiety Anxiety DefensesDocument14 pagesAnxiety Anxiety Defensesapi-3697326100% (1)
- Respiratory 3Document36 pagesRespiratory 3api-3697326No ratings yet
- P A I N 1my Power PointDocument38 pagesP A I N 1my Power Pointapi-3697326100% (1)
- Learning Guide: Central Texas College Department of NursingDocument26 pagesLearning Guide: Central Texas College Department of Nursingapi-3697326No ratings yet
- Respirations 1Document42 pagesRespirations 1api-3697326No ratings yet
- SyllabusDocument9 pagesSyllabusapi-3697326No ratings yet
- Lions and Tigers and BearsDocument20 pagesLions and Tigers and Bearsapi-369732650% (2)
- Fe 4Document36 pagesFe 4api-3697326No ratings yet
- Diesel Engine Lab ReportDocument27 pagesDiesel Engine Lab ReportParadoodleNo ratings yet
- Whisper 500 Spec SheetDocument1 pageWhisper 500 Spec Sheetfranco cuaylaNo ratings yet
- Silicon Epitaxial Planar Transistor 2SA1179: Galaxy ElectricalDocument5 pagesSilicon Epitaxial Planar Transistor 2SA1179: Galaxy ElectricalsacralNo ratings yet
- Comparatives and SuperlativesDocument2 pagesComparatives and Superlativesjcarlosgf60% (5)
- Magic Coco Tiles: Green Building MaterialDocument17 pagesMagic Coco Tiles: Green Building MaterialnikoNo ratings yet
- Nurs 512 Andersen Behavioral TheoryDocument7 pagesNurs 512 Andersen Behavioral Theoryapi-251235373No ratings yet
- By Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSDocument9 pagesBy Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSAngela SaldajenoNo ratings yet
- Full Download Test Bank For Nursing A Concept Based Approach To Learning Volume II 3rd Edition 3rd Edition PDF Full ChapterDocument36 pagesFull Download Test Bank For Nursing A Concept Based Approach To Learning Volume II 3rd Edition 3rd Edition PDF Full Chaptersignor.truss.j26uk100% (17)
- 4a-Ancient Indian Engineering BotanyDocument44 pages4a-Ancient Indian Engineering BotanyAshok NeneNo ratings yet
- Recipes For Ceviche, Pebre and Pisco SourDocument4 pagesRecipes For Ceviche, Pebre and Pisco SourJoaquín Rolón CarrerasNo ratings yet
- New Microsoft Office Word DocumentDocument3 pagesNew Microsoft Office Word DocumentSunija SelvamNo ratings yet
- Boroscope Inspection Procedure 7th Stage StatorDocument15 pagesBoroscope Inspection Procedure 7th Stage StatorAPU SHOP BTH MS100% (2)
- 1198-Article Text-5716-1-10-20221219Document9 pages1198-Article Text-5716-1-10-20221219Hendarko AriNo ratings yet
- Presentation On Dysuria 1Document25 pagesPresentation On Dysuria 1ankur acharyaNo ratings yet
- Carjackked TrainingDocument7 pagesCarjackked TrainingErios 50No ratings yet
- LOKRING Technical Documentation Submittal Brass enDocument32 pagesLOKRING Technical Documentation Submittal Brass enYamilelcNo ratings yet
- RNA and Protein Synthesis Problem SetDocument6 pagesRNA and Protein Synthesis Problem Setpalms thatshatterNo ratings yet
- 250 Watt Solar Panel SpecificationsDocument2 pages250 Watt Solar Panel Specificationsfopoku2k20% (1)
- "Mode One" Author & Dating Coach Alan Roger Currie Releases Criticism of Alleged Harvey Weinstein BehaviorDocument3 pages"Mode One" Author & Dating Coach Alan Roger Currie Releases Criticism of Alleged Harvey Weinstein BehaviorPR.com100% (1)
- Carbonyl Compounds: Unit 4 Rates, Equilibria and Further Organic ChemistryDocument5 pagesCarbonyl Compounds: Unit 4 Rates, Equilibria and Further Organic ChemistryKirusaanth SathiyathasanNo ratings yet
- Hindustan Coca-Cola Beverages PVT LTD B-91 Mayapuri Industrial Area Phase-I New DelhiDocument2 pagesHindustan Coca-Cola Beverages PVT LTD B-91 Mayapuri Industrial Area Phase-I New DelhiUtkarsh KadamNo ratings yet
- The Consumption of WaterDocument2 pagesThe Consumption of WaterasungapeNo ratings yet
- English The RainDocument2 pagesEnglish The RainsmitaNo ratings yet
- Industrial Diesel Generator Set - 50 HZ: General Specifications KOHLER Premium QualityDocument7 pagesIndustrial Diesel Generator Set - 50 HZ: General Specifications KOHLER Premium QualityABCD123655No ratings yet
- Employement ExchangeDocument22 pagesEmployement ExchangeNeelam ThakurNo ratings yet
- Plumbing Specifications: Catch Basin PlanDocument1 pagePlumbing Specifications: Catch Basin PlanMark Allan RojoNo ratings yet
- Hilti AnchorsDocument202 pagesHilti AnchorsmwendaNo ratings yet